Epicardial adipose tissue in obesity with heart failure with preserved ejection fraction: Cardiovascular magnetic resonance biomarker study
Ju-Wei Shao,Bing-Hua Chen,Kamil Abu-Shaban,Ahmad Baiyasi,Lian-Ming Wu,Jing Ma
Abstract BACKGROUND Obesity has become a serious public health issue,significantly elevating the risk of various complications.It is a well-established contributor to Heart failure with preserved ejection fraction (HFpEF).Evaluating HFpEF in obesity is crucial.Epicardial adipose tissue (EAT) has emerged as a valuable tool for validating prognostic biomarkers and guiding treatment targets.Hence,assessing EAT is of paramount importance.Cardiovascular magnetic resonance (CMR) imaging is acknowledged as the gold standard for analyzing cardiac function and morphology.We hope to use CMR to assess EAT as a bioimaging marker to evaluate HFpEF in obese patients.AIM To assess the diagnostic utility of CMR for evaluating heart failure with preserved ejection fraction [HFpEF;left ventricular (LV) ejection fraction ≥ 50%] by measuring the epicardial adipose tissue (EAT) volumes and EAT mass in obese patients.METHODS Sixty-two obese patients were divided into two groups for a case-control study based on whether or not they had heart failure with HFpEF.The two groups were defined as HFpEF+and HFpEF-.LV geometry,global systolic function,EAT volumes and EAT mass of all subjects were obtained using cine magnetic resonance sequences.RESULTS Forty-five patients of HFpEF-group and seventeen patients of HFpEF+group were included.LV mass index (g/m2) of HFpEF+group was higher than HFpEF-group (P < 0.05).In HFpEF+group,EAT volumes,EAT volume index,EAT mass,EAT mass index and the ratio of EAT/[left atrial (LA) left-right (LR) diameter] were higher compared to HFpEF-group (P < 0.05).In multivariate analysis,Higher EAT/LA LR diameter ratio was associated with higher odds ratio of HFpEF.CONCLUSION EAT/LA LR diameter ratio is highly associated with HFpEF in obese patients.It is plausible that there may be utility in CMR for assessing obese patients for HFpEF using EAT/LA LR diameter ratio as a diagnostic biomarker.Further prospective studies,are needed to validate these proof-of-concept findings.
Key Words: Heart failure with preserved ejection fraction;Epicardial adipose tissue;Obesity;Cardiac magnetic resonance
INTRODUCTION
Obesity has become a serious public health issue,significantly elevating the risk of various complications,including heart disease,type 2 diabetes,and hypertension[1].It is a well-established contributor to heart failure (HF)[2].Heart failure with preserved ejection fraction (HFpEF) is a prevalent and deadly clinical syndrome characterized by HF with a left ventricular ejection fraction (LVEF) ≥ 50%.Within the broader HFpEF population,the obesity-HFpEF phenotype has been identified as a distinct subset,potentially necessitating specific treatments[3].Recently,there is growing recognition of the importance of anti-atherogenic and anti-inflammatory effects,known as 'meta-inflammatory' mechanisms,in the treatment of "obese HFpEF"[4].Therefore,evaluating HFpEF in obesity is crucial.
Epicardial adipose tissue (EAT) refers to the fat surrounding the heart in the epicardium,also known as visceral fat[5].Studies have linked EAT with HF,revealing higher EAT volume in HF patients with HFpEF[6,7].Consequently,EAT has emerged as a valuable tool for validating prognostic biomarkers and guiding treatment targets[8,9].Hence,assessing EAT is of paramount importance.
Accurate detection and quantification of EAT can be accomplished through 2-dimensional (2D) echocardiography,contrast-free computed tomography (CT),and magnetic resonance imaging (MRI)[10].Echocardiography,a widely used cardiac imaging method for EAT measurement,does not expose patients to ionizing radiation[11,12].However,it predominantly provides 2D cardiac images,measuring only the thickness,not the volume or mass of EAT[13].Additionally,echocardiography-derived measurements may be more prone to inter-observer errors compared to crosssectional modalities.Consequently,echocardiography is only accurate for measuring the maximum EAT thickness[14].Nevertheless,the definitive EAT thickness threshold for use as a prognostic biomarker is yet to be determined[15].Moreover,the applicability of EAT thickness is often constrained by suboptimal acoustic windows in obese patients.
More recently,the heightened EAT in patients exhibiting the HFpEF phenotype can be assessed through CT,potentially indicating adverse cardiac function[16].Evaluation of cardiac function is feasible.However,CT is constrained by radiation exposure.Cardiovascular magnetic resonance (CMR) imaging is acknowledged as the gold standard for analyzing cardiac function and morphology[17].Utilizing three-dimensional cine images,CMR enables accurate and reproducible quantification of EAT thickness,volume,and mass.Some recent CMR studies have compared EAT quantities in HFpEF groups with controls,emphasizing the need to focus on EAT beyond an individual's overall body fat concerning HFpEF[18,19].However,it is conceivable that obesity could confound such findings due to the general increase in adipose tissue throughout the body.To our knowledge,no studies have investigated EAT metrics (including volume or mass) in obese patients using CMR to determine the association with HFpEF and whether EAT metrics could serve as a biomarker for predicting HFpEF in the obese population.Therefore,this study aims to employ CMR to examine EAT in the obese population with and without HFpEF,considering the association with co-morbidities,biomarkers,contractility parameters,and myocardial function assessed by CMR.
MATERIALS AND METHODS
Study participants
The study followed a case-control,prospective clinical design,enrolling 69 obese individuals from October 2019 to August 2020 at Shanghai Jiao Tong University School of Medicine Affiliated Renji Hospital.HFpEF patients meeting specific criteria were included: (1) Left ventricular (LV) ejection fraction ≥ 50%,assessed by echocardiography;(2) New York Heart Association class ≥ II,with either E/e′ > 13 and mean e′septal and lateral wall < 9 cm/s on echocardiography;(3) plasma brain natriuretic peptide (BNP) > 35 pg/mL[20].Exclusion criteria were: (1) general contraindication to CMR;(2) poor imaging quality;(3) heart failure with mid-range ejection fraction (HFmrEF) and heart failure with reduced ejection fraction (HFrEF);(4) congenital heart disease;(5) acute ischemic cardiac injury;(6) hypertrophic cardiomyopathy;(7) greater than moderate valvular disease;(8) sarcoidosis;(9) amyloidosis;(10) thalassemia;and (11) hemochromatosis.The study complied with the 1964 Declaration of Helsinki and subsequent amendments.
Five patients were excluded due to exclusion criteria,and 2 were excluded for poor image quality and MRI contraindications.Seventeen obese patients with HFpEF and 45 obese patients without HFpEF,meeting inclusion criteria with matched gender and age,were recruited.Obesity was defined as a body mass index (BMI) ≥ 30.0 kg/m2,following Asian-Pacific cutoff points[21].All participants provided written,informed consent.BMI (kg/m2) was calculated,and measurements included blood pressure,serum cholesterol,serum triglycerides,serum high-density lipoprotein cholesterol,and serum low-density lipoprotein cholesterol.Fasting glucose and hemoglobin A1c levels were also assessed.The study flow diagram is depicted in Figure 1.
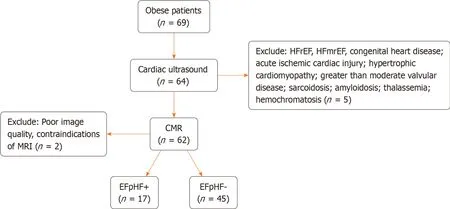
Figure 1 The study flow diagram. HFrEF: Heart failure with reduced ejection fraction;HFmrEF: Heart failure with mid-range ejection fraction;MRI: Magnetic resonance imaging.
Magnetic resonance protocol
All examination data were obtained using a 3.0 Tesla magnetic resonance scanner (Prisma,Siemens,Erlangen,Germany) equipped with a 32-channel cardiac coil.Cine imaging was acquired through retrospective ECG gating with balanced steady-state free-precession during horizontal and vertical long-axis views,and in 16 short-axis slices covering the entire left ventricle to evaluate left ventricular function and cardiac mechanics.Data in the short-axis plane were collected at the mid-ventricular level.Imaging parameters comprised a repetition time of 326.6 ms,echo time of 1.09 ms,flip angle of 35°,field of view of 385 × 385 mm2,matrix of 156 × 192,slice thickness of 8 mm,slice gap of 4 mm,receiver bandwidth of 1085 Hz/px,GRAPPA acceleration factor 2,linear phase-encoding ordering,and 25 cardiac phases.
Data analysis
EAT was defined as the fat between the myocardium and the visceral pericardium.The borders of the EAT image were manually delineated on contiguous end-diastolic short-axis slices from the base to the apex using commercially available software (cvi42,Circle Cardiovascular Imaging Inc.,Calgary,Canada) (Figure 2).Additionally,LV endocardial and epicardial borders were manually outlined slice by slice based on the initial contour set at end-diastole.EAT mass was estimated by multiplying the EAT volume by 0.92[22].CMR image analyses were independently conducted by two experienced radiologists who were blinded to the study.LV end-diastolic volume (LVEDV),LV end-systolic volume (LVESV),and LV mass were measured and normalized to body surface area.LV stroke volume (LVSV) was calculated by subtracting LVESV from LVEDV.LVEF was computed as LVSV/LVEDV × 100%.The measurement of left atrial anteriorposterior (LA AP) diameter and left atrial left-right (LA LR) diameter followed a previously reported method[23].
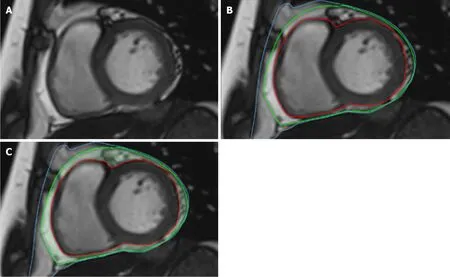
Figure 2 Epicardial adipose tissue image. A: Volume measurement of epicardial adipose tissue outlining the contours of the myocardium in short-axis images of end-diastole;B: The visceral pericardium (green line),myocardium (red line) and the parietal (blue line) in the same short-axis image;C: EAT: Epicardial adipose tissue (laurel-green area).
Statistical analysis
The normality of continuous samples was assessed using the Kolmogorov-Smirnov test for normal distribution.Group comparisons were conducted using Student’s t-test for continuous variables or Fisher’s exact test for categorical variables.Initial univariate analyses and stepwise multivariate linear regression analyses were executed to identify predictors of the odds of HFpEF in the obese population.Covariates with a univariatePvalue < 0.10 were included in the multivariate logistic regression analysis[24,25].Pearson’s correlation coefficient was employed for correlation analyses.APvalue < 0.05 was considered significant.Intra-and inter-observer repeatability of parameters derived from CMR were assessed using the intra-class correlation coefficient (ICC) in 30 randomly selected patients from the same cohort[26].An ICC > 0.75 was considered indicative of good agreement[27].Descriptive and comparative statistical analyses were carried out using SPSS version 23.0 (IBM Corp.,Armonk,United States) and GraphPad Prism v.8.0 (GraphPad Software,Inc.,CA,United States).
RESULTS
Baseline characteristics
Table 1 summarizes the baseline characteristics.The mean ages of the obese populations with HFpEF (HFpEF+) and without HFpEF (HFpEF-) were 42.94 ± 3.37 years and 36.60 ± 1.80 years,respectively (P> 0.05).In the HFpEF+group,17.6% were older than 60 years,compared to 0.02% in the HFpEF-group.Among HFpEF+patients,64.7% were males,while 55.6% of HFpEF-patients were males.No significant differences were observed in body surface area (BSA),BMI,BNP,and resting diastolic blood pressure,but there were significant differences between the two groups (P< 0.05).The prevalence of fatty liver was higher in the HFpEF-group (58.8%) compared to the HFpEF+group (28.9%) (P=0.0253),with no significant differences in other complications.Resting systolic blood pressure (SBP),regardless of medication control,was significantly higher in HFpEF+patients than in the HFpEF-group (P=0.0370).
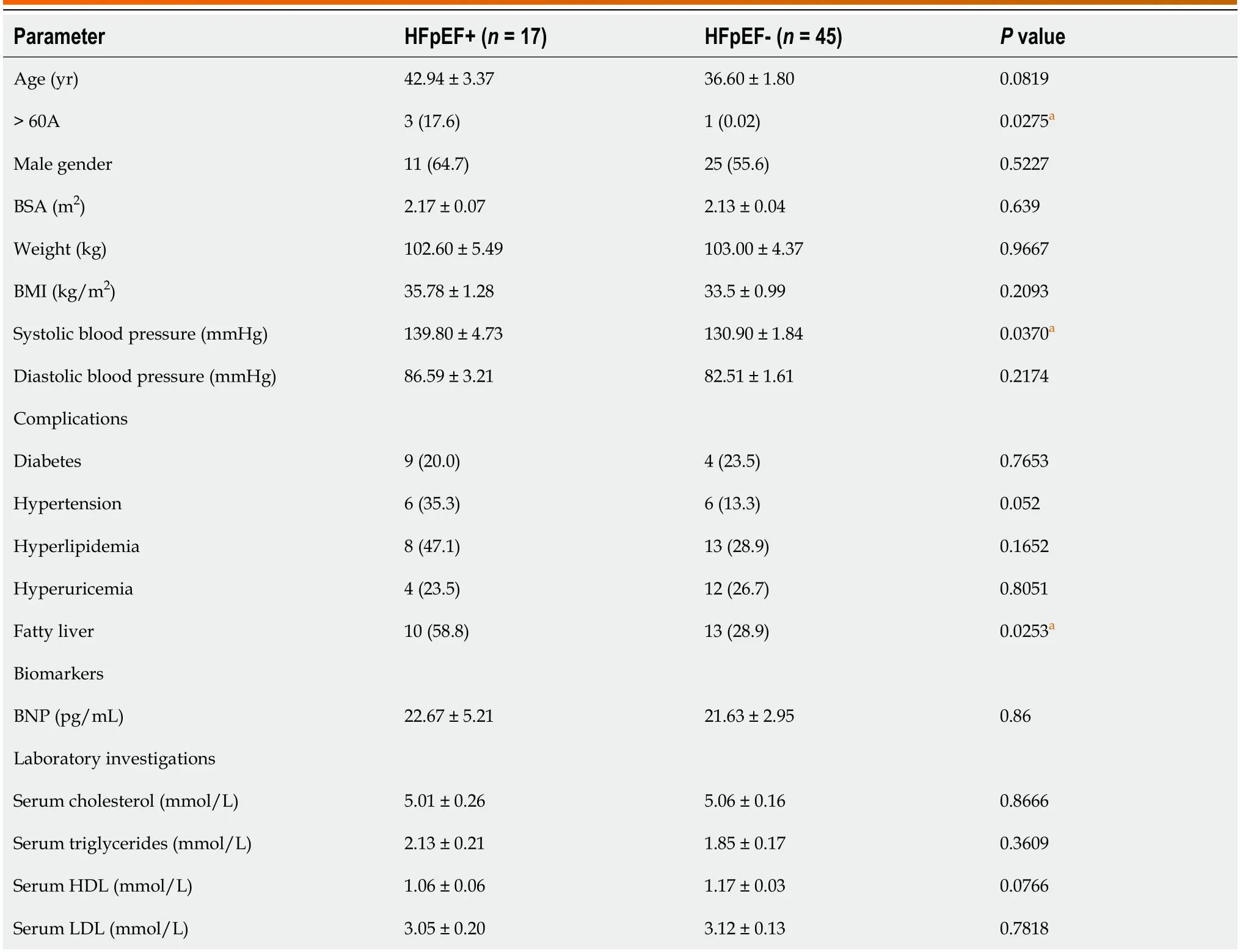
Table 1 Baseline characteristics and laboratory findings of the obesity in populations with and without heart failure with preserved ejection fraction,n (%)
CMR parameters of left ventricular morphology and function epicardial adipose tissue of the obesity in populations with and without HFpEF
The measurements' results are detailed in Table 2.In terms of morphological characteristics,the HFpEF+group displayedsignificant remodeling with a greater LV mass index compared to the HFpEF-group.No significant differences were observed in other morphological and functional parameters between the two groups.Regarding epicardial adipose tissue,both EAT volume and EAT mass were significantly larger in HFpEF+individuals,and these differences persisted after adjustment for BSA (P=0.04 for EAT volume/BSA andP=0.04 for EAT mass/BSA).A significant difference in the EAT/LA LR diameter ratio was observed between the two groups (P=0.02) (Figure 3).

Figure 3 Comparison of different epicardial adipose tissue parameters in obese population with and without heart failure with preserved ejection fraction. A: Epicardial adipose tissue volume group;B: Epicardial adipose tissue index group;C: Epicardial adipose tissue mass group;D: Epicardial adipose tissue mass index group;E: Epicardial adipose tissue/left atrial left-right diameter ratio group.EAT: Epicardial adipose tissue;LA: Left atrial;LR: Left-right diameter;HFpEF: Heart failure with preserved ejection fraction.
Associations of epicardial adipose tissue and morphological and functional parameters in HFpEF+ group
The correlation analysis results of all four epicardial adipose tissue parameters (EAT volume,EATi,EAT mass,EAT mass index) with eight CMR-measured LV morphological and functional parameters are presented in Table 3.No significant correlations were observed.
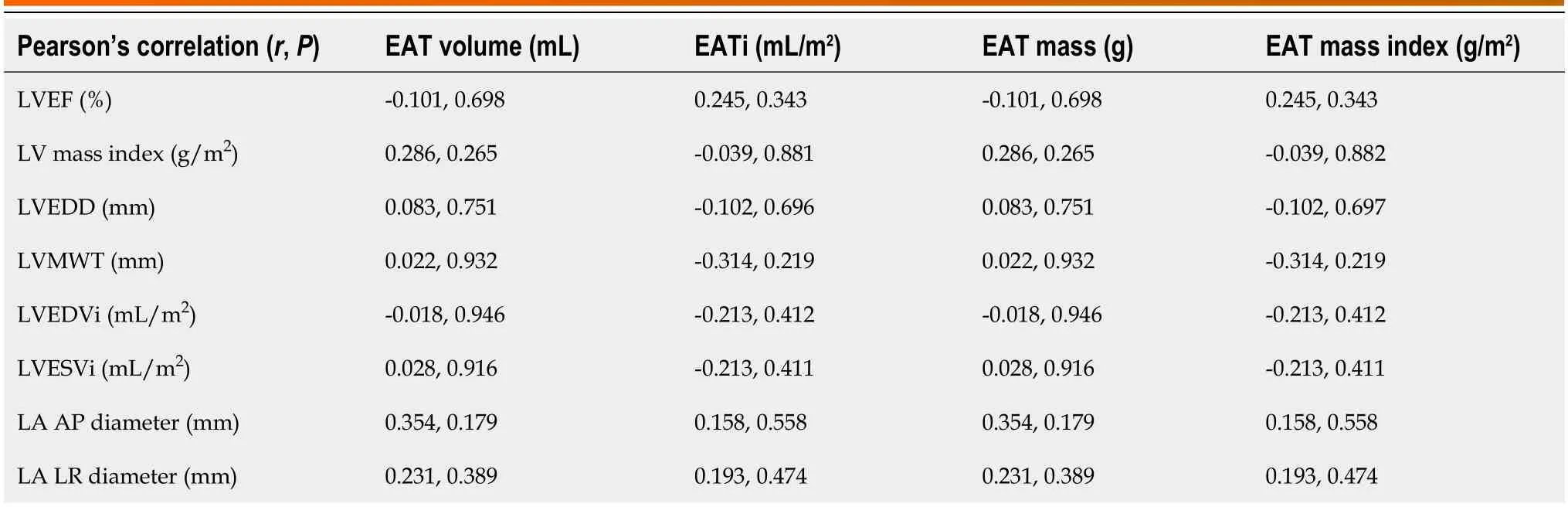
Table 3 Relationships between epicardial adipose tissue and morphological and functional parameters in heart failure with preserved ejection fraction positive group
Logistic regression analysis
In univariate logistic regression analysis,EAT mass index [odds ratio (OR)=1.05,P=0.04,95%CI: 1.00-1.10],EATi (OR=1.05,P=0.04,95%CI: 1.00-1.09),and EAT/LA LR diameter ratio (OR=3.99,P=0.03,95%CI: 1.17-13.58) showed significant associations with HFpEF.EAT volume (OR=1.02,P=0.051,95%CI: 1.00-1.04) trended toward an association with HFpEF.In multivariate analysis,the variable associated with HFpEF in the obese population was the EAT/LA LR diameter ratio (OR=4.60,P=0.02,95%CI: 1.22-17.35) (Table 4).
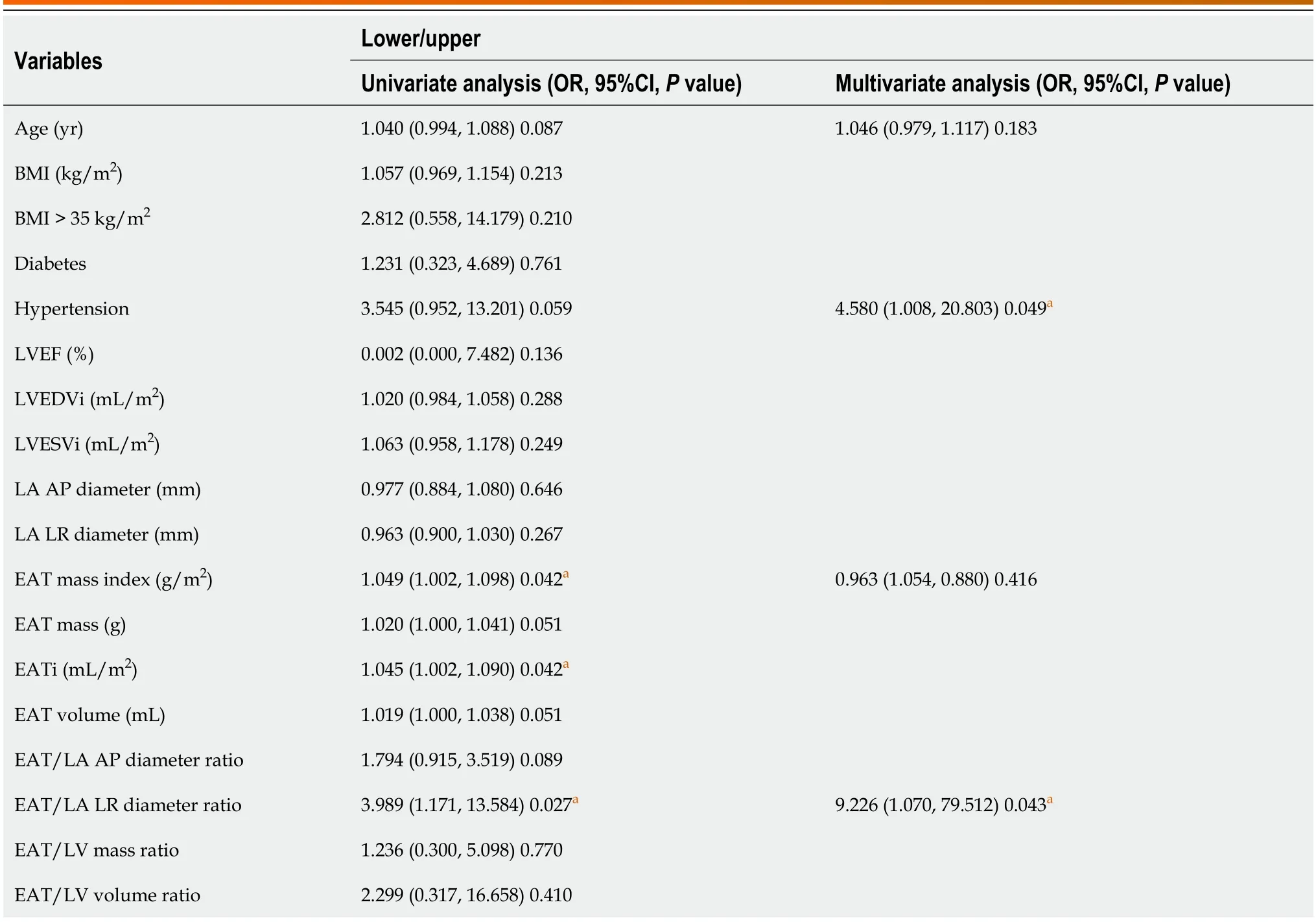
Table 4 Variables associated with the heart failure with preserved ejection fraction in obesity population
Intraobserver and interobserver variability
Table 5 summarizes the ICC values for both intraobserver and interobserver reproducibility.The eight CMR-measured parameters demonstrated high reproducibility,ranging from 0.71 to 0.93 for intra-observer and 0.88 to 0.98 for interobserver,respectively.
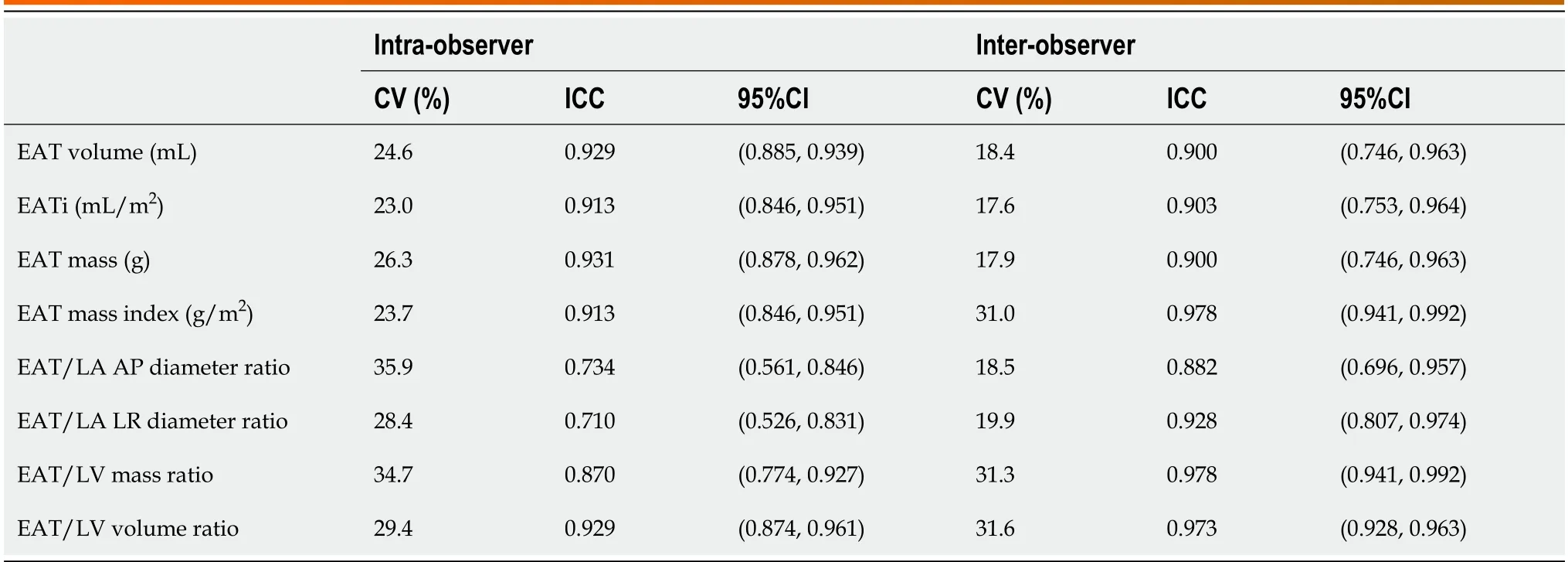
Table 5 Intra-observer and inter-observer reproducibility for epicardial adipose tissue parameters
DISCUSSION
In this study,we conducted a comprehensive comparison of EAT volume,mass,and functional characteristics,as determined by CMR,among individuals with obesity in the absence of HFpEF (HFpEF-) and HFpEF+groups.The main findings of our study are as follows: (1) EAT volume and EAT mass were significantly increased in the obese HFpEF+group compared to the obese HFpEF-group,and these differences persisted after adjustment for BSA;(2) in the obese population,the EAT/LA LR diameter ratio can serve as an alternative method to differentiate between HFpEF+and HFpEF-groups;and (3) a higher EAT/LA LR diameter ratio was associated with a higher risk of HFpEF after adjusting for potential confounders.
The utilization of CMR for EAT measurement in our study provides a comprehensive assessment of cardiac structure and function in individuals with HFpEF[28].Additionally,our study contributes to the existing literature by implementing and evaluating the quantification of EAT using MRI during diastole[29].In a prior study,we demonstrated CMR's sensitivity and accuracy in detecting conventional atrial geometry in dialysis patients with HFpEF[30].The present study,employing CMR to measure EAT,holds significant strengths over prior investigations examining the association between EAT and HFpEF in an obese population.
Our findings revealed that EAT volume and EAT mass,determined by CMR,were significantly higher in the HFpEF+group compared to the HFpEF-group,with significant differences in EATi and EAT mass index as well.EAT,recognized as a risk factor for heart failure,particularly in the obese population[30,31],is implicated as an independent risk factor for HFpEF[32,33].EAT's invasion into and around coronary arteries contributes to microvascular dysfunction,ventricular dilatation,and heart failure[12].Adipocytes within EAT possess endocrine functions,synthesizing aldosterone and angiotensinogen[34].Moreover,EAT serves as a marker for inflammatory factors[35].Consistent with previous echocardiographic studies associating EAT thickness with HFpEF[36],our results further support this relationship.
In our study,there was a significant increase in LV mass index in the HFpEF+group compared to the HFpEF-group.The space between the myocardial surface and the visceral pericardium may be filled with EAT,potentially covering the entire epicardium[37].In the obese population,the excess EAT could impose an increased burden on both ventricles,ultimately leading to left ventricular hypertrophy[38].These findings are consistent with prior investigations into obesity.A previous study utilizing CMR demonstrated that individuals with uncomplicated obesity and HFpEF exhibited extensive LV geometric remodeling,impaired ventricular function,and increased myocardial thickness[39].
Our research revealed that the EAT/LA LR diameter ratio was higher in the HFpEF+group compared to the HFpEF-group,and this ratio was significantly associated with HFpEF.While no prior study has specifically investigated changes in the EAT/LA LR diameter ratio,it has been demonstrated to be impaired before left atrial enlargement in obese patients with HFpEF experiencing diastolic heart failure[40].A recent study utilizing transthoracic echocardiography indicated that increased EAT thickness was linked to poorer left atrial function in HFpEF[41].Additionally,another echocardiography-related study suggested that the presence of increased EAT is associated with a greater increase in cardiac filling pressures in patients with the obese phenotype of HFpEF[11].Thus,the utilization of EAT/LA LR,assessed through CMR,could play a crucial role in the differentiation and diagnosis of obese HFpEF in clinical practice in the future.The EAT/LA LR diameter ratio may serve as a novel imaging biomarker.
Our study demonstrated no correlation between the four epicardial adipose tissue parameters (EAT volume,EATi,EAT mass,EAT mass index) and CMR-measured LV morphological and functional parameters.This finding aligns with some of the current studies[39].It is plausible that our sample size is relatively small,and more conclusive results may emerge in the future with a larger sample size.
According to prior studies,age significantly contributes to EAT accumulation and may exert a substantial influence on its buildup[42].In our study,there was no significant difference in age between the two groups,indicating that the effect of age on EAT was excluded.Despite the lack of statistical significance,there appears to be a trend towards older age in patients with HFpEF,supported by a higher proportion of subjects aged over 60 years in the HFpEF+cohort.Additionally,resting SBP was significantly higher in HFpEF+patients than in the HFpEF-group.Patients with HFpEF exhibit reduced aortic distensibility and increased systolic blood pressure[43].Previous findings suggest that obesity has a detrimental impact on prehypertension and hypertension,irrespective of general obesity or abdominal obesity presence[44].
CONCLUSION
EAT/LA LR diameter ratio is highly associated with HFpEF in obese patients.It is plausible that there may be utility in CMR for assessing obese patients for HFpEF using EAT/LA LR diameter ratio as a diagnostic biomarker.Further prospective studies,are needed to validate these proof-of-concept findings.
ARTICLE HIGHLIGHTS
Research background
Obesity has become a serious public health issue,significantly elevating the risk of various complications.It is a wellestablished contributor to Heart failure with preserved ejection fraction (HFpEF).Evaluating HFpEF in obesity is crucial.Epicardial adipose tissue (EAT) has emerged as a valuable tool for validating prognostic biomarkers and guiding treatment targets.Hence,assessing EAT is of paramount importance.Cardiovascular magnetic resonance (CMR) imaging is acknowledged as the gold standard for analyzing cardiac function and morphology.We hope to use CMR to assess EAT as a bioimaging marker to evaluate HFpEF in obese patients.
Research motivation
The aim of this study was to clarify the utility of using CMR-measured EAT as a diagnostic biomarker for assessing HFpEF in obese patients.
Research objectives
This study aims to employ CMR to examine EAT in the obese population with and without HFpEF,considering the association with co-morbidities,biomarkers,contractility parameters,and myocardial function assessed by CMR.
Research methods
The study was designed as a case-control,prospective clinical study.Obese patients were divided into two groups for a case-control study based on whether or not they had heart failure with HFpEF.The two groups were defined as HFpEF+and HFpEF-.LV geometry,global systolic function,EAT volumes and EAT mass of all subjects were obtained using cine magnetic resonance sequences.The novelty of this study is to investigate EAT metrics (including volume or mass) in obese patients using CMR to determine whether or not EAT metrics are associated with HFpEF and whether EAT metrics appear to be a biomarker for predicting HFpEF in the obese population.
Research results
Forty-five patients of HFpEF-group and seventeen patients of HFpEF+group were included.LV mass index (g/m2) of HFpEF+group was higher than HFpEF-group (P< 0.05).In HFpEF+group,EAT volumes,EAT volume index,EAT mass,EAT mass index and EAT/ left atrial (LA) left-right (LR) diameter ratio were higher compared to HFpEF-group.In multivariate analysis,higher EAT/LA LR diameter ratio was independently associated with higher odds ratio (OR=4.597) of HFpEF.
Research conclusions
There was a strong correlation between increased EAT volumes and HFpEF in the obese.EAT/LA LR diameter ratio is highly associated with HFpEF in the obese.
Research perspectives
Given the significant findings,there may be some diagnostic utility in CMR for assessing the obese for HFpEF.
FOOTNOTES
Co-first authors:Ju-Wei Shao and Bing-Hua Chen.
Co-corresponding authors:Jing Ma and Lian-Ming Wu.
Author contributions:Shao JW and Wu LM were scientific study designers;Ma J,Chen BH,and Wu LM were involved in data collection;Shao JW and Chen BH contributed to data analysis;and Shao JW,Abu-Shaban K,Baiyasi A,and Wu LM were involved in manuscript writing and revision;All authors read and approved the final manuscript;Special thanks to Booth TC for revising the manuscript.Ma J and Wu LM as co-corresponding authors are threefold.First,the research was conducted through a joint effort,with co-corresponding authorship rightly mirroring the shared workload and commitment needed for both the study's execution and the ensuing publication.This approach also facilitates efficient handling of post-submission processes,thereby bolstering the paper's integrity and excellence.Second,the research group comprised individuals with varied specialties and backgrounds,making the appointment of cocorresponding authors a representation of this multidisciplinary nature.This arrangement allows for a thorough and nuanced exploration of the subject matter,thereby deepening the reader's comprehension through diverse expert insights.At last,Ma Jing and Wu LM made equally significant contributions throughout the research journey.Selecting them as co-corresponding authors honors their joint efforts,underscoring the importance of teamwork and cooperative spirit inherent in this project.
Supported byNational Natural Science Foundation of China,No.81 873887;National Natural Science Foundation of China Youth Project,No.82 101981;and Shanghai Jiao Tong University School of Medicine Double Hundred Outstanding Person Project,No.20191904.
Institutional review board statement:This is a retrospective study.All the data are from our database.All patients were anonymised and the data collection was a health check.
Clinical trial registration statement:We didn't register this trial on the Clinical Trial Registration platform prior to this trial.
Informed consent statement:This is a retrospective study.All the data are from our database.All patients were anonymised and the data collection was a health check.We have signed Informed Consent Form for this study.
Conflict-of-interest statement:All authors have no conflicts of interest to disclose.
Data sharing statement:No additional data are available.
CONSORT 2010 statement:The authors have read the CONSORT 2010 statement,and the manuscript was prepared and revised according to the CONSORT 2010 statement.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Ju-Wei Shao 0000-0002-2271-1677;Lian-Ming Wu 0000-0001-7381-5436;Jing Ma 0009-0006-8115-9970.
S-Editor:Liu JH
L-Editor:A
P-Editor:Zheng XM
 World Journal of Cardiology2024年3期
World Journal of Cardiology2024年3期
- World Journal of Cardiology的其它文章
- Predictors of permanent pacemaker implantation following transcatheter aortic valve replacement-the search is still on!
- Mechanistic insights into fasting-induced autophagy in the aging heart
- Interest of thoracic ultrasound after cardiac surgery or interventional cardiology
- Cardiac arrest,stony heart,and cardiopulmonary resuscitation: An updated revisit
- Sex and racial disparities in non-alcoholic fatty liver disease-related cardiovascular events: National inpatient sample analysis (2019)
- Severe hypoxemia after radiofrequency ablation for atrial fibrillation in palliatively repaired tetralogy of Fallot: A case report
