左西孟旦对心力衰竭危重患者死亡率影响的Meta分析
何芳,杨国杰
左西孟旦对心力衰竭危重患者死亡率影响的Meta分析
何芳,杨国杰
目的:研究左西孟旦对心力衰竭(心衰) 危重患者死亡率的影响。
方法:在PubMed、EMBASE、Cochrane心血管组数据库中收集左西孟旦与其他干预措施的随机对照研究,文献检索时间从各数据库建库时间至 2014-07。根据Jadad量表评价纳入文献的质量并提取资料。对符合质量标准的对照研究(无剂量及给药方式的限制)采用 Rev Man 5.2 进行Meta 分析。根据纳入标准最终入选37篇文献,共入选病例 4 470例。
结果:左西孟旦与对照组相比能降低心脏相关疾病所致心衰危重患者的死亡率[危险比(RR):0.85; 95%可信区间(CI):0.75~0.97;P=0.02],并能降低心脏手术所致心衰危重患者的死亡率(RR:0.49;95% CI:0.28~0.85;P=0.01)。与多巴酚丁胺进一步比较,左西孟旦能降低心衰危重患者的死亡率(RR:0.84;95%CI:0.73~0.98;P=0.02),并能降低缺血性心脏病所致心衰危重患者的死亡率(RR:0.85;95%CI:0.73~0.99;P=0.04)。
结论:左西孟旦能降低心脏相关疾病、心脏手术及缺血性心脏病所致心衰危重患者的死亡率。
左西孟旦;心力衰竭;死亡率
(Chinese Circulation Journal, 2015,30:422.)
2012年欧洲心脏病学会发布的心力衰竭(心衰)诊疗指南指出,急性心衰的治疗首先要改善症状,稳定血液动力学;当症状严重并对扩血管药及利尿剂等一线治疗药物无效时,需用正性肌力药阻止病情恶化[1]。但几乎所有大规模的随机对照试验(RCT)及Meta分析均证实,传统正性肌力药在提高心脏输出量、稳定患者症状的同时,会增加心肌缺血、心律失常的发生率,进一步增加心衰患者的死亡率。
左西孟旦的问世为心衰治疗提供了新的选择。它作为一种新型钙增敏剂,通过增强收缩蛋白对钙离子的敏感性而增加心肌收缩力,促进血管平滑肌及线粒体膜上三磷酸腺苷(ATP)依赖的钾通道开放而扩张外周血管,降低心脏前后负荷,改善心率变异性[2]。左西孟旦作为最新一代的心衰治疗药是否能够降低远期死亡率,目前争议较大。因此,我们通过Meta分析来评估左西孟旦对缺血性心脏病、心脏手术等所致心衰危重患者的死亡率的影响,从而为临床应用左西孟旦提供有力的证据。
1 资料与方法
文献检索和筛选:入选标准: (1)RCT; (2)患者符合纽约心脏协会(NYHA)心功能分级Ⅲ~Ⅵ级、急性失代偿性心衰; (3)左西孟旦与其他干预措施的对比。排除标准: (1)重复发表; (2)数据不完整; (3)非成人研究; (4)缺乏相关结局事件的数据。
文献检索(检索词、检索库):在PubMed、EMBASE、Cochrane心血管组数据库中检索截止至2014-07的有关左西孟旦在急性心衰患者中应用的相关研究,同时通过初始文献后的参考文献手动检索可能符合的研究。无语言、研究年限的限制。英文检索词为:levosimendan、 heart failure、mortality。检出相关文献185 篇,根据纳入标准最终入选 37 篇文献;共入选病例4 470 例。
资料提取和质量分析:对于每项研究我们均详细提取了研究的背景和特征(作者、发表时间、研究类型、研究对象、例数、剂量、用药持续时间、随访时间等)。应用评价RCT的Jadad量表对每项研究进行质量评估,该量表包括4个方面的评价:随机序列的产生、随机化隐藏、盲法、撤出与退出。评价后分数越高质量越好,1~3分视为低质量,4~7分视为高质量。
风险评估:提取临床异质性,采用Cochrane系统评价员手册5.1版偏倚风险评估标准对所有入选研究进行评估,评估内容包括分配隐藏、随机序列的产生、盲法的实施等方面。我们把可能的最长随访时间-死亡率作为分析的终点事件。
统计学分析:计数资料采用危险比(RR)为合并统计量,各统计量均以95% 可信区间(CI)表示;P<0.05 为差异有统计学意义。利用Revman5.2软件进行数据分析及合成。采用Cochrane Q检验对所有纳入的临床试验进行异质性分析,并通过I2值定量评估。P>0.05且I2<25%,表明各项研究同质性较好,采用M-H固定效应模型分析数据。以漏斗图的形式对入选试验的发表偏倚进行估计。
2 结果
文献检索结果:共检出185篇文献,通过阅读文题和摘要,排除病例报道、动物实验及与研究目的无关的文献123 篇,初筛出62篇文献;进一步阅读全文排除无相关数据16篇,非RCT 5篇,综述1篇,重复发表3篇,最终按照纳入和排除标准入选37篇文献[3-39]。
文献基本特征和质量评价:37篇研究共入选病例4 470例,纳入文献的背景信息见表1。所有研究均报告了左西孟旦组和对照组患者的住院死亡率;24篇研究完整报告了两组患者心脏相关疾病所致心衰的死亡率[3-7,9-12,14,17,19,20,23-26,30-32,36-39];11篇研究完整报告了两组患者心脏手术所致心衰的死亡率[8,13,15-16,18,22,27-28,33-35];16篇研究完整报告了左西孟旦与多巴酚丁胺对心衰危重患者的死亡率[3,10,19-32]的影响;14篇研究完整报告了左西孟旦与多巴酚丁胺对缺血性心脏病所致心衰危重患者的死亡率[3,10,19,20,22-28,30-32]的影响。Jadad量表评估的结果表明:总共37篇研究中4分为15篇,5分为11篇,6分为4篇,最高7分为7篇。
异质性分析及 Meta 分析:(1)左西孟旦组和对照组比较:①对心脏相关疾病所致心衰危重患者:试验组共纳入2 193例患者,其中住院期间全因死亡发生378 例;对照组共纳入1 725 例患者,住院期间发生全因死亡352例。异质性检验结果显示:24篇研究间不存在明显的异质性(χ2=19.50,P=0.55,I2=0%),采用固定效应模型进行 Meta 分析,分析结果显示(图 1):与对照组相比,左西孟旦组住院死亡率明显降低,差异具有统计学意义(RR:0.85;95% CI:0.75~0.97;P=0.02)。②对心脏手术所致心衰危重患者:试验组共纳入255例患者,其中住院期间发生全因死亡14例;对照组共纳入225例患者,住院期间发生全因死亡29例。异质性检验结果显示:11篇研究间不存在明显的异质性(χ2=9.46,P=0.31,I2=15%),采用固定效应模型进行 Meta 分析,分析结果显示(图2)。与对照组相比,左西孟旦组住院死亡率明显降低,差异具有统计学意义(RR:0.49;95% CI:0.28~0.85;P=0.01)。(2)左西孟旦和多巴酚丁胺比较:①对心衰危重患者:试验组共纳入1 198例患者,其中住院期间全因死亡发生246例;对照组共纳入1 167例患者,住院期间发生全因死亡293例。异质性检验结果显示:16篇研究间不存在明显的异质性(χ2=11.03,P=0.75,I2=0%),采用固定效应模型进行 Meta 分析,分析结果显示(图3):与多巴酚丁胺组相比,左西孟旦组住院死亡率明显降低,差异具有统计学意义(RR:0.84;95%CI:0.73~0.98; P=0.02)。②对缺血性心脏病所致心衰危重患者:试验组共纳入1 162例患者,其中住院期间全因死亡发生229例;对照组共纳入1 131例患者,住院期间全因死亡发生271例。异质性检验结果显示:14篇研究间不存在明显的异质性(χ2=10.83,P=0.62,I2=0%),采用固定效应模型进行 Meta 分析,分析结果显示(图4):与多巴酚丁胺相比,左西孟旦组住院死亡率明显降低,差异具有统计学意义(RR:0.85;95%CI:0.73~0.99;P=0.04)。 漏斗图分析 4组比较均应用漏斗图估计发表偏倚;漏斗图均大体对称,提示发表偏倚不明显。

表1 纳入37篇文献的基本信息

图1 左西孟旦组与对照组对心脏相关疾病所致心力衰竭危重患者死亡率比较的森林图

图2 左西孟旦组与对照组对心脏手术所致心力衰竭危重患者死亡率比较的森林图

图3 左西孟旦与多巴酚丁胺对心力衰竭危重患者死亡率影响比较的森林图
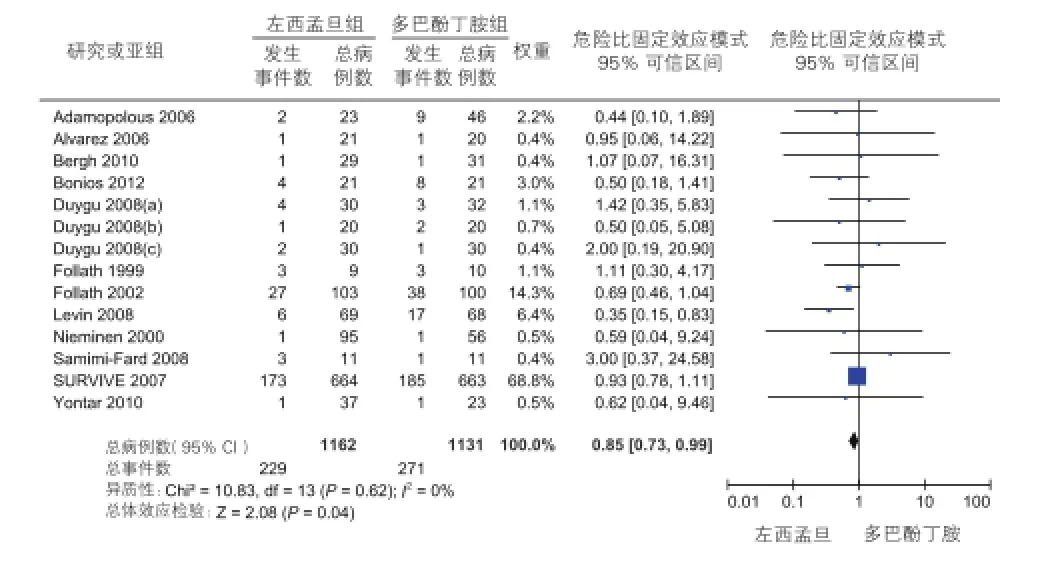
图4 左西孟旦与多巴酚丁胺对缺血性心脏疾病所致心力衰竭危重患者死亡率影响比较的森林图
3 讨论
37篇文献共4 470例患者纳入到本研究中,Meta分析的结果表明:与对照组相比,心脏相关疾病及心脏手术所致心衰危重患者应用左西孟旦可以降低死亡率;与多巴酚丁胺相比,心衰危重患者及缺血性心脏病所致心衰危重患者应用左西孟旦可以降低死亡率。
目前心衰治疗中应用传统正性肌力药有诸多限制和风险。大量研究显示传统正性肌力药可以迅速缓解症状,改善血流动力学,但会引起心肌损伤,增加心衰患者短期死亡率。而左西孟旦的问世为心衰的治疗提供了全新的视角。它能改善血流动力学,降低肺毛细血管楔压,增加心脏输出量,减轻心脏症状及降低住院率。
目前的临床试验在左西孟旦对心衰患者死亡率的影响上仍存在争议。本文对心脏相关疾病及心脏手术所致心衰进行了亚组分析。结果显示,左西孟旦与对照药物或安慰剂相比,能降低心脏相关疾病所致心衰危重患者的死亡率。与Silvetti 等[40]研究结果一致,他们的结果显示,间断应用左西孟旦可显著提高心衰患者中期的生存率(RR :0.55;95% CI:0.37~0.84;P=0.005)。相反,Huang等[41]研究表明,与多巴酚丁胺相比,左西孟旦不能降低心脏相关疾病所致心衰的死亡率(RR:0.88;95% CI:0.75~1.03;P=0.11)。不同的结果可能是与其比较的对照组不同所致。
Landoni 等[42]发现,应用左西孟旦可使心脏手术后患者生存率明显提高(OR:0.35;95% CI:0.18~0.71;P=0.003),并显著减低术后心肌肌钙蛋白的高峰释放。此外,Maharaj 等[43]指出,应用左西孟旦可使冠状动脉重建术后患者生存率提高(OR:0.40;95% CI:0.21~0.76;P=0.005)。本研究纳入的11项试验中5项关于冠状动脉旁路移植术[8,13,18,28,33],6项关于主动脉瓣膜手术[15,16,22,27,34,35]、腹主动脉瘤手术及其他类型[16]。研究发现,左西孟旦与药物或安慰剂组相比能显著降低心脏手术患者的死亡率。这与上述研究结果基本一致,提示左西孟旦具有抗缺血、心肌保护和扩血管效应,从而使冠脉血流增加,改善心功能,降低死亡率。
与多巴酚丁胺相比,左西孟旦降低心衰患者死亡率的机制是:(1)通过增强肌钙蛋白C对钙离子的敏感性增加心肌收缩力;(2)通过开放血管平滑肌细胞的ATP敏感钾通道(KATP)而扩张外周血管,降低心脏前、后负荷;(3)有磷酸二脂酶Ⅲ抑制作用[44]。Huang等[41]的研究显示,与多巴酚丁胺相比,左西孟旦可以降低心衰危重患者的死亡率(RR:0.81;95% CI:0.70~0.92;P=0.002)。此外,Delaney等[45]研究发现,与多巴酚丁胺比较时,左西孟旦可以提高患者生存率。本研究结果与上述报道是一致的。
急性心肌缺血引起心肌收缩功能下降,最终导致心脏泵衰竭。左西孟旦在增强心肌收缩力和扩张冠脉的同时不增加氧耗,对于急性心梗伴心原性休克的患者疗效较好。相反,多巴酚丁胺的致命弱点在于增加氧耗,进一步加重心肌损伤。Landoni等[42]的Meta分析发现,左西孟旦能降低心肌梗死等缺血性心脏病所致心衰患者的死亡率。同样,本研究结果显示,与多巴酚丁胺相比,左西孟旦能够降低缺血性心脏病所致心衰危重患者的死亡率。
本研究的优点:(1)本文不但与多巴酚丁胺这一传统的正性肌力药比较,并且还对缺血性心脏病、心脏手术等所致的心衰危重患者的死亡率进行了亚组分析,得出的结论具有说服力。(2)与既往相关文献相比,本文纳入的研究较全面、最新且剔除了低质量的研究。
研究的局限性:(1)随访时间长度不一,有的仅持续1天[31];(2)由于数据不足,对败血症的亚组分析不能得出清楚的结论,还有未能对呋塞米及前列腺素E进一步比较得出结论;(3)发表偏倚:虽然进行了大量的、广泛的检索,仍不能排除潜在的发表偏倚。但本Meta分析的漏斗图显示出对称图形,因此发表偏倚很低。
[1] McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail, 2012, 14: 803-869.
[2] 马兰, 金振一, 金壹伍, 等. 左西孟旦对急性失代偿性心力衰竭患者心率变异性的影响. 中国循环杂志, 2014, 29: 198-200.
[3] Nieminen MS, Akkila J, Hasenfuss G, et al. Hemodynamic and neurohumoral effects of continuous infusion of levosimendan in patients with congestive heart failure. J Am Coll Cardiol, 2000, 36: 1903-1912.
[4] Slawsky MT, Colucci WS, Gottlieb SS, et al. Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Study Investigators. Circulation, 2000, 102: 2222-2227.
[5] Moiseyev VS, Poder P, Andrejevs N, et al. Safety and efficacy of a novel calcium sensitizer, levosimendan, in patients with left ventricular failure due to an acute myocardial infarction: a randomized, placebocontrolled, double-blind study (RUSSLAN). Eur Heart J, 2002, 23: 1422-1432.
[6] Kivikko M, Lehtonen L, Colucci WS, et al. Sustained hemodynamic effects of intravenous levosimendan. Circulation, 2003, 107: 81-86.
[7] Packer M, Colucci WS, Fisher L, et al. Development of a comprehensive new endpoint for the evaluation of new treatments for acute decompensated heart failure: results with levosimendan in the REVIVE 1 study. J Card Fail , 2003, 9: S61.
[8] Barisin S, Husedzinovic I, Sonicki Z, et al. Levosimendan in offpump coronary artery bypass: A four-times masked controlled study. J Cardiovasc Pharmacol, 2004, 44: 703-708.
[9] Tziakas DN, Chalikias GK, Hatzinikolaou HI, et al. Levosimendan use reduces matrix metalloproteinase-2 in patients with decompensated heart failure. Cardiovasc Drugs Ther, 2005, 19: 399- 402.
[10] Adamopoulos S, Parissis JT, Iliodromitis EK, et al. Effects of levosimendan versus dobutamine on inflammatory and apoptotic pathways in acutely decompensated chronic heart failure. Am J Cardiol, 2006, 98: 102-106.
[11] Flevari P, Parissis JT, Leftheriotis D, et al. Effect of levosimendan on ventricular arrhythmias and prognostic autonomic indexes in patients with decompensated advanced heart failure secondary to ischemic or dilated cardiomyopathy. Am J Cardiol , 2006, 98: 1641-1645.
[12] Cleland JG, Freemantle N, Coletta AP, et al. Clinical trials update from the American Heart Association: REPAIR-AMI, ASTAMI, JELIS, MEGA, REVIVE-II, SURVIVE, and PROACTIVE. Eur J Heart Fail, 2006, 8: 105-110.
[13] Tritapepe L, De Santis V, Vitale D, et al. Preconditioning effects of levosimendan in coronary artery bypass grafting-a pilot study. Br J Anaesth, 2006, 96: 694-700.
[14] Ikonomidis I, Parissis JT, Paraskevaidis I, et al. Effects of levosimendan on coronary artery flow and cardiac performance in patients with advanced heart failure. Eur J Heart Fail, 2007, 9: 1172-1177.
[15] Järvelä K, Maaranen P, Sisto T, et al. Levosimendan in aortic valve surgery: Cardiac performance and recovery. J Cardiothorac Vasc Anesth, 2008, 22: 693- 698.
[16] Leppikangas H, Tenhunen JJ, Lindgren L, et al. Effects of levosimendan on indocyanine green plasma disappearance rate and the gastric mucosal-arterial pCO2gradient in abdominal aortic aneurysm surgery. Acta Anaesthesiol Scand, 2008, 52: 785-792.
[17] Kleber FX, Bollmann T, Borst MM, et al. Repetitive dosing of intravenous levosimendan improves pulmonary hemodynamics in patients with pulmonary hypertension: Results of a pilot study. J Clin Pharmacol , 2009, 49: 109-115.
[18] Ristikankare A, Pöyhiä R, Eriksson H, et al. Effects of Levosimendan on Renal Function in Patients Undergoing CoronaryArtery Surgery. J Cardiothorac Vasc Anesth, 2012, 26: 591-595.
[19] Follath F, Hinkka S, Jager D, et al. Dose-ranging and safety with intravenous levosimendan in low-output heart failure: experience in three pilot studies and outline of the levosimendan infusion versusdobutamine (LIDO) trial. Am J Cardiol, 1999, 83: 211-251.
[20] Follath F, Cleland JG, Just H, et al. Efficacy and safety of intravenous levosimendan comparedwith dobutamine in severe low output heart failure (the LIDO study): a randomized double-blind trial. Lancet, 2002, 360: 196-202.
[21] Morelli A, de Castro S, Teboul JL, et al. Effects of levosimendan on systemic and regional hemodynamics in septic myocardial depression. Intensive Care Med, 2005, 31: 638-644.
[22] Alvarez J, Bouzada M, Fernández AL, et al. Hemodynamic effects of levosimendan compared with dobutamine in patients with low cardiac output after cardiac surgery. Rev Esp Cardiol, 2006, 59: 338-345 .
[23] Mebazaa A, Nieminen MS, Packer M, et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE Randomized Trial. JAMA, 2007, 297 : 1883-1891.
[24] Duygu H, Ozerkan F, Nalbantgil S, et al. Effect of levosimendan on E/ E′ratio in patients with ischemic heart failure. Int J Cardiol, 2008, 123: 201-203.
[25] Duygu H, Turk U, Ozdogan O, et al. Levosimendan versus dobutamine in heart failure patients treated chronically with carvedilol. Cardiovasc Ther, 2008, 26: 182-188.
[26] Duygu H, Nalbantgil S, Ozerkan F, et al. Effects of levosimendan on left atrial functions in patients with ischemic heart failure. Clin Cardiol, 2008, 31: 607-613.
[27] Malfatto G, Rosa FD, Villani A, et al. Intermittent levosimendan infusions in advanced heartfailure: favourable effects on left ventricular function, neurohormonal balance, and one-year survival. J Cardiovasc Pharmacol , 2012, 60: 450-455.
[28] Levin R, Degrange MA, Porcile R, et al. The calcium sensitizer levosimendan gives superior results to dobutamine in postoperative low cardiac output syndrome. Rev Esp Cardiol, 2008, 61: 471-479.
[29] Alhashemi JA, Alotaibi QA, Abdullah GM, et al. Levosimendan vs dobutamine in septic shock. J Crit Care, 2009, 24: e14.
[30] Bergh CH, Andersson B, Dahlstrom U, et al. Intravenous levosimendan vs. dobutamine in acute decompensated heart failure patients on β-blockers. Eur J Heart Fail, 2010, 12: 404-410.
[31] Yontar OC, Yilmaz MB, Yalta K, et al . Acute effects of levosimendan and dobutamine on QRS duration in patients with heart failure. Arq Bras Cardiol, 2010, 95: 738-742.
[32] Bonios MJ, Terrovitis JV, Drakos SG, et al. Comparison of three different regimens of intermittent inotrope infusions for end stage heart failure. Int J Cardiol, 2012, 159: 225-229.
[33] Al-Shawaf E, Ayed A, Vislocky I, et al. Levosimendan or milrinone in the type 2 diabetic patient with low ejection fraction undergoing elective coronary artery surgery. J Cardiothorac Vasc Anesth , 2006, 20: 353-357.
[34] De Hert SG, Lorsomradee S, Cromheecke S, et al. The effects of levosimendan in cardiac surgery patients with poor left ventricular function. Anesth Analg , 2007, 104: 766-773.
[35] De Hert SG, Lorsomradee S, vanden Eede H, et al. A randomized trial evaluating different modalities of levosimendan administration in cardiac surgery patients with myocardial dysfunction. J Cardiothorac Vasc Anesth, 2008, 22: 699-705.
[36] Berger R, Moertl D, Huelsmann M, et al. Levosimendan and prostaglandin E1 for uptitration of beta-blockade in patients with refractory, advanced chronic heart failure. Eur J Heart Fail , 2007, 9: 202-208.
[37] Samimi-Fard S, Garcia-Gonzalez MJ, Dominguez-Rodriguez A, et al. Effects of levosimendan versus dobutamine on long-term survival of patients with cardiogenic shock after primary coronary angioplasty. Int J Cardiol, 2008, 127: 284-287.
[38] Mavrogeni S, Giamouzis G, Papadopoulou E, et al. A 6-month followup of intermittent levosimendan administration effect on systolic function, specific activity questionnaire, and arrhythmia in advanced heart failure. J Card Fail , 2007, 13: 556-559.
[39] Zemljic G, Bunc M, Yazdanbakhsh AP, et al. Levosimendan improves renal function in patients with advanced chronic heart failure awaiting cardiac transplantation. J Card Fail, 2007, 13: 417- 421.
[40] Silvetti S, Greco T, Prima AL, et al. Intermittent levosimendan improves mid-term survival in chronic heart failure patients: metaanalysis of randomised trials. Clin Res Cardiol, 2014, 103: 505-513.
[41] Huang X, Lei S, Zhu MF, et al. Levosimendan versus dobutamine in critically ill patients: a meta-analysis of randomized controlled trials. J Zhejiang Univ-Sci B (Biomed & Biotechnol), 2013, 14: 400-415.
[42] Landoni G, Mizzi A, Biondi-Zoccai G, et al. Reducing mortality in cardiacsurgery with levosimendan: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth, 2010, 24: 51-57.
[43] Maharaj R, Metaxa V. Levosimendan and mortality after coronary revascularisation: a meta-analysis of randomized controlled trials. Crit Care, 2011, 15: R140.
[44] 杜贺, 史承勇, 陈少萍. 左西孟旦的研究新进展. 中国循环杂志, 2014, 29: 555-557.
[45] Delaney A, Bradford C, McCaffrey J, et al. Levosimendan for the treatment of acute severe heart failure: a meta-analysis of randomized controlled trials. Int J Cardiol, 2010, 138: 281-289.
The Impact of Levosimendan on Mortality in Patients With Severe Heart Failure by Meta-analysis
HE Fang, YANG Guo-jie.
Department of Geriatric Cardiology, First Affiliated Hospital of Zhengzhou University, Zhengzhou (450000), Henan, China
Objective: To investigate the impact of levosimendan on mortality in patients with severe heart failure (HF) by Meta-analysis.Methods: We search the PubMed, EMBASE and Cochrane Central Registry of cardiovascular disease to identify all randomized impact of levosimendan vs other medications. The document retrieval was from the establishment of each database until 2014-07. The literatures were taken based on Jadad scale standard and the qualified control study was used without dose and time restrictions by Rev Man 5.2 soft ware, and a total of 37 articles with 4470 patients were finally enrolled for Meta-analysis.Results: Compared with controlling medications, levosimendan could decrease the mortality in patients with cardiac disease caused severe HF (RR: 0.85; 95% CI 0.75-0.97; P=0.02), and cardiac surgery caused severe HF (RR: 0.49; 95% CI 0.28-0.85; P=0.01). Compared with dobutamine, levosimendan could reduce the mortality in patients with severe HF (RR: 0.84; 95% CI 0.73-0.99; P=0.02) and severe ischemic HF (RR: 0.85; 95% CI 0.73-0.99; P=0.04).Conclusion: Levosimendan may reduce the mortality in patients with severe HF caused by cardiac disease, cardiac surgery and ischemic cardiac injury.
Levosimendan; Heart failure; Mortality
2014-10-11)
(编辑:常文静)
450000 河南省郑州市,郑州大学第一附属医院 老年医学心血管科
何芳 硕士研究生 主要从事心力衰竭研究 Email:971493419@qq.com 通讯作者:杨国杰 Email:yang63315@126.com
R54
A
1000-3614(2015)05-0422-06
10.3969/j.issn.1000-3614.2015.05.004

