特应性皮炎患者皮肤表面真菌定植分析
张秀钦 程波 纪明开 方芳 苏惠春
361026厦门市海沧医院皮肤科(张秀钦);福建医科大学附属第一医院皮肤科(程波、纪明开、方芳、苏惠春)
特应性皮炎患者皮肤表面真菌定植分析
张秀钦 程波 纪明开 方芳 苏惠春
361026厦门市海沧医院皮肤科(张秀钦);福建医科大学附属第一医院皮肤科(程波、纪明开、方芳、苏惠春)
目的观察念珠菌、红酵母、青霉、曲霉在特应性皮炎患者皮肤表面定植情况,分析这4种常见致敏真菌与特应性皮炎症状严重程度的相关性。方法特应性皮炎患者50例,健康对照组20例。刮取特应性皮炎患者皮损部位及非皮损部位的鳞屑(以四肢屈侧为主)、健康对照组肘关节屈侧皮屑行真菌镜检,无1例发现菌丝或假菌丝;将皮屑标本接种于沙氏葡萄糖培养基,置25℃恒温箱内培养,发现真菌及酵母样可疑菌落,转种沙氏葡萄糖培养基斜面,获得纯培养后,根据菌落形态特征及颜色、菌落生长的快慢、镜下孢子及菌丝的特征进行菌种鉴定。结果特应性皮炎组50例,皮损表面检出念珠菌29例(58%)、红酵母17例(34%);健康对照组20例,检出念珠菌5例(25%)、红酵母2例(10%),特应性皮炎组念珠菌、红酵母检出率明显高于健康对照组(χ2值分别为6.23、4.10,均P< 0.05)。重度患者25例,检出念珠菌19例(76%)、红酵母12例(48%);中度患者25例,检出念珠菌10例(40%)、红酵母5例(20%),重度患者皮损表面念珠菌、红酵母检出率明显高于中度患者(χ2值分别为6.65、4.37,均P<0.05)。患者组与对照组青霉、曲霉检出率差异无统计学意义。结论特应性皮炎患者皮肤表面念珠菌、红酵母定植明显高于健康对照组,且重度患者定植率高于中度患者,表明真菌定植的种类与皮肤的健康状况相关,与特应性皮炎患者症状的严重程度相关。
皮炎,特应性;白色念珠菌;红酵母属;产黄青霉;曲霉菌属
特应性皮炎(AD)是一种遗传过敏性疾病,除了对食物和吸入物过敏外,其血清对微生物的sIgE抗体升高,包括金黄色葡萄球菌、马拉色菌、白念珠菌[1]。最近的研究表明,真菌致敏原在遗传过敏性疾病中也发挥重要作用。我们采用常规真菌培养方法,观察白念珠菌、红酵母、青霉、曲霉在AD患者皮损和非皮损部位,以及中度及重度患者皮肤表面的定植情况。
一、对象与方法
1.对象:2012年6-12月,福建医科大学附属第一医院皮肤科门诊AD患者50例,均符合Williams提出的AD诊断标准[2],所有受试者2周内均未使用抗真菌药、糖皮质激素或免疫抑制剂治疗,无其他免疫及炎症性疾病等病史。其中男28例,女22例;年龄2~45岁,平均15岁;病程2个月至18年,平均7年。伴过敏性鼻炎或哮喘20例。AD病情严重程度评分(SCORAD)为26~84.5分,平均(57±16)分;中、重度患者各25例。对照组20例,女8例,男12例,年龄2~40岁,平均12岁,均为健康体检者,无过敏性疾病及家族过敏史,无免疫及炎症性疾病等病史,两组在年龄及性别方面差异无统计学意义,具有可比性。SCORAD评分标准为,①皮肤病变范围:以占1%体表面积为1分;成人头颈部、臂部各占9%,躯干前后各占13.5%,下肢各占22.5%;<14岁儿童头颈部、臂部各9%,躯干前后及下肢各18%;②皮损严重度:包括6项体征:a红斑,b丘疹/水肿,c糜烂、渗出(或)结痂,d角化脱屑,e浸润与苔藓化,f皮肤干燥(评价未受累皮肤);用3分4级法:0分为无,1分为轻度,2分为中度,3分为重度;③瘙痒及影响睡眠程度:应用视觉模拟评分法(VAS),VAS标尺由0分(无瘙痒)至10分(患者所能想象最严重的瘙痒),患者在标尺上标出最能代表其瘙痒强度的点;评价睡眠的方法同瘙痒一样。SCORAD=①/5+②×7/2+③,总分范围0~103分。SCORAD评分分级为:轻度<15分;中度15~40分;重度>40分。
2.试验材料:沙氏葡萄糖培养基根据《全国临床检验操作规程》配制,法国柯玛嘉显色培养基(广州益满生物科技有限公司)。
3.方法:取患者皮损部位的鳞屑及非皮损部位的皮屑(均以四肢屈侧为主),健康对照组刮取肘关节屈侧的皮屑。所有标本均先行镜检,无1例发现菌丝或假菌丝。将标本接种于沙氏葡萄糖培养基,置25℃恒温箱内连续培养5 d,逐日观察,2周内不生长,判断为阴性;发现真菌及酵母样可疑菌落,转种沙氏葡萄糖培养基斜面,获得纯培养后鉴定。根据菌落形态特征及颜色、菌落生长的快慢、镜下孢子及菌丝的特征鉴定。念珠菌加用法国柯玛嘉显色培养基,30~37℃培养48 h,根据念珠菌显色培养说明书判断结果,绿色、翠绿色菌落判断为白念珠菌;蓝灰色、铁灰色为热带念珠菌;紫红色边缘模糊,有微毛,判断为克柔念珠菌;整个菌落紫红色判断为光滑念珠菌;白色菌落判断为其他念珠菌。AD患者皮损及非皮损部位共培养出念珠菌48株,其中白念珠菌16株,热带念珠菌11株,克柔念珠菌9株,光滑念珠菌5株,其他念珠菌7株。
4.统计方法:用SPSS13.0统计软件,χ2检验分析阳性率差异,P<0.05为差异有统计学意义。
二、结果
见表1。AD患者皮损部位念珠菌、红酵母定植阳性率明显高于健康对照组,χ2值分别为6.23、4.10,均P< 0.05;两组间曲霉、青霉阳性率差异无统计学意义,χ2值分别为1.17、0.17,均P>0.05。AD患者非皮损部位念珠菌、红酵母、曲霉、青霉定植阳性率与健康对照组比较,差异均无统计学意义,χ2值分别为1.07、1.70、0.58、0.30,P> 0.05。AD患者皮损部位念珠菌阳性率明显高于非皮损部位(χ2=4.00,P<0.05);而红酵母、曲霉、青霉两组间差异无统计学意义,χ2值分别为0.42、0.17、1.56,均P> 0.05。
重度AD患者皮损部位念珠菌、红酵母定植阳性率明显高于中度患者,χ2值分别为6.65、4.37,均P< 0.05;青霉、曲霉两组间差异无统计学意义,χ2值分别为0.35、0.86,均P>0.05。重度AD患者非皮损部位念珠菌阳性率明显高于中度患者,χ2=4.16,P<0.05;红酵母、曲霉、青霉两组间差异无统计学意义,χ2值分别为1.59、0.33、2.05,P> 0.05。见表1。
三、讨论
皮肤屏障功能障碍可能是引起AD等干燥性皮肤病的主要原因,皮肤屏障功能破坏,增加了对外界不同刺激的敏感性,使环境的过敏原,如花粉、屋尘螨和微生物等容易穿透皮肤,产生sIgE抗体,使AD患者的病情加重。真菌在皮肤表面的定植情况与皮肤的生理条件及健康状况相关[3],真菌致敏原在遗传过敏性疾病中发挥重要作用[4],AD患者的汗液中有一种主要变应原,是由球形马拉色菌产生的真菌蛋白mgl⁃1304,可引起Ⅰ型变态反应[5];超过三分之二以头颈部为主要表现的成人特应性皮炎患者对伊曲康唑和其他唑类抗真菌药物有明显的疗效[6]。AD患者皮肤表面定植的真菌包括念珠菌、马拉色菌、青霉、曲霉[7],SCORAD评分与曲霉、马拉色菌、青霉、念珠菌的sIgE水平有显著相关性[8]。本研究中,AD患者皮损部位念珠菌定植阳性率为58%。一项关于AD患者念珠菌的皮肤点刺试验中,70%发生速发型过敏反应[9];而Chang等[10]报道,81.2%的AD患者血清中检测到念珠菌特异性IgE。真菌孢子在环境中普遍存在,室外最常见的真菌致敏原是枝孢菌和链格孢,室内最常见的是曲霉和青霉,它们的存在不受季节影响。本试验中曲霉、青霉皮肤表面定植阳性率与健康对照没有显著差别。
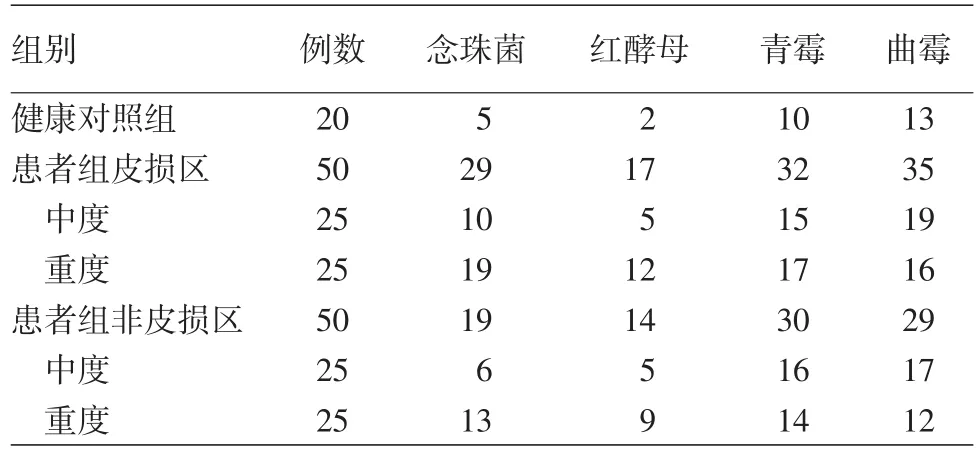
表1 特应性皮炎患者皮损及非皮损部位4种真菌培养结果(例)
[1]Sonesson A,Bartosik J,Christiansen J,et al.Sensitization to skin⁃associated microorganisms in adult patients with atopic dermatitis is of importance for disease severity[J].Acta Derm Venereol,2013,93(3):340⁃345.DOI:10.2340/00015555⁃1465.
[2] Williams HC.Diagnostic criteria for atopic dermatitis[J].Lancet,1996,348(9038):1391 ⁃1392.DOI:10.1016/S0140 ⁃6736(05)65466⁃9.
[3] Zhang E,Tanaka T,Tajima M,et al.Characterization of the skin fungal microbiota in patients with atopic dermatitis and in healthy subjects[J].Microbiol Immunol,2011,55(9):625 ⁃632.DOI:10.1111/j.1348⁃0421.2011.00364.x.
[4]刘芳,桑红,胡文星,等.浅部真菌感染和变态反应性皮肤病相关性研究[J].中国真菌学杂志,2011,6(6):344⁃349.DOI:10.3969/j.issn.1673⁃3827.2011.06.007.Liu F,Sang H,Hu WX,et al.Correlation of superficial fungal infections and allergic skin diseases[J].Chin J Mycol,2011,6(6):344⁃349.DOI:10.3969/j.issn.1673⁃3827.2011.06.007.
[5]Hiragun T,Ishii K,Hiragun M,et al.Fungal protein MGL_1304 in sweat is an allergen for atopic dermatitis patients[J].J Allergy Clin Immunol,2013,132(3):608 ⁃615e4.DOI:10.1016/j.jaci.2013.03.047.
[6]Kaffenberger BH,Mathis J,Zirwas MJ.A retrospective descriptive study of oral azole antifungal agents in patients with patch test⁃negative head and neck predominant atopic dermatitis[J].J Am Acad Dermatol,2014,71(3):480⁃483.DOI:10.1016/j.jaad.2014.04.045.
[7]Zhang E,Tanaka T,Tajima M,et al.Characterization of the skin fungal microbiota in patients with atopic dermatitis and healthy subjects[J].Microbiol Immunol,2011,55(9):625⁃632.DOI:10.1111/j.1348⁃0421.2011.00364.x.
[8]Ong PY,Ferdman RM,Church JA.Association of microbial IgE sensitizations with asthma in young children with atopic dermatitis[J].Ann Allergy Asthma Immunol,2012,108(3):212⁃213.DOI:10.1016/j.anai.2011.12.016.
[9]Kobayashi T,Yamada M,Aihara M,et al.Immedeate and delayed⁃type reactivity to fungi and effects of antifungal drugs on atopic dermatitis[J].Arerugi,2006,55(2):126⁃133.PMID:16719000.
[10]Chang FY,Lee JH,Yang YH,et al.Analysis of the serum levels of fungi⁃specific immunoglobulin E in patients with allergic diseases[J].Int Arch Allergy Immunol,2011,154(1):49⁃56.DOI:10.1159/000319208.
Analysis of fungal colonization in skin surfaces of patients with atopic dermatitis
Zhang Xiuqin,Cheng Bo,Ji Mingkai,Fang Fang,Su Huichun
Department of Dermatology,Xiamen Haicang Hospital,Xiamen 361026,Fujian,China(Zhang XQ);Department of Dermatology,First Affiliated Hospital of Fujian Medical University,Fuzhou 350005,China(Cheng B,Ji MK,Fang F,Su HC)
ObjectiveTo analyze the colonization ofCandida,Rhodotorula,PenicilliumandAspergillusin skin surfaces of patients with atopic dermatitis,and to assess the relationship between the four common fungal allergens and severity of atopic dermatitis.MethodsFifty patients with atopic dermatitis and 20 healthy controls were enrolled.Scales were scraped from lesional and non⁃lesional skin of flexural extremities of the patients,as well as from normal skin of the flexural elbow of healthy controls,then were subjected to microscopic examination and culture.Scale specimens were inoculated onto Sabouraud dextrose agar medium and cultured at 25℃in a constant temperature incubator.Subsequently,suspected fungal or yeast⁃like colonies were collected for pure culture.Finally,fungal strains were identified according to colony morphology,color,growth speed,as well as microscopic features of spores and hyphae.ResultsNo hyphae or pseudohyphae were found in any case by microscopic examination.Candida albicansandRhodotorulawere detected in 29(58%)and 17(34%)out of the 50 patients,respectively,and in 5(25%)and 2(10%)out of the 20 healthy controls,respectively.The detection rates ofCandida albicansandRhodotorulawere significantly higher in the patients than in the controls(χ2=6.23,4.10,respectively,bothP< 0.05).Of 25 patients with severe lesions,19(76%)and 12(48%)were colonized byCandida albicansandRhodotorularespectively;among 25 patients with moderate lesions,10(40%)and 5(20%)were colonized byCandida albicansandRhodotorularespectively.An increase was observed in the detection rates ofCandida albicansandRhodotorulain the patients with severe lesions compared with those with moderate lesions(χ2=6.65,4.37,respectively,bothP< 0.05).There was no significant difference in the detection rate ofPenicilliumorAspergillusbetween the patients and health controls.ConclusionThe colonization rates ofCandida albicansandRhodotorulaon skin surfaces were higher in patients with atopic dermatitis than in healthy controls,and higher in patients with severe lesions than in patients with moderate lesions,indicating that the types of colonizing fungi are associated with the health status of skin and severity of symptoms in patients with atopic dermatitis.
Dermatitis,atopic;Candida albicans;Rhodotorula;Penicillium chrysogenum;Aspergillus
Cheng Bo,Email:chengbo630415@126.com
程波,Email:chengbo630415@126.com
10.3760/cma.j.issn.0412⁃4030.2016.07.015
2015⁃07⁃28)
(本文编辑:吴晓初)