Establishment of trauma registry at Queen Elizabeth Central Hospital (QECH), Blantyre, Malawi and mapping of high risk geographic areas for trauma
Linda C. Chokotho, Wakisa Mulwafu, Mulinda Nyirenda, Foster J. Mbomuwa, Hemant G. Pandit, Grace Le,Christopher Lavy
1 Beit Cure International Hospital, Blantyre, Malawi
2 Department of Surgery, College of Medicine, University of Malawi, Blantyre, Malawi
3 Adult Emergency and Trauma Center, Queen Elizabeth Central Hospital, Ministry of Health, Blantyre, Malawi
4 Chapel Allerton Hospital, Uinversity of Leeds, Leeds, UK
5 Nuf field Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Oxford, UK
KEY WORDS: Trauma Registry; Adult injuries; Hot spot analysis; Low and middle income countries
INTRODUCTION
Injuries were responsible for approximately 4.7 million deaths worldwide in 2015, accounting for about 8.5% of all mortality.[1]The death toll worldwide from injuries is equivalent to the total mortality caused by HIV, Malaria and Tuberculosis combined.[2]The burden of injuries disproportionately affects low- and - middle income countries (LMICs) with almost 90% of deaths due to injuries occurring in LMICs.[3]
Prevention of trauma and improved care of the injured patients when trauma occurs help to reduce morbidity and mortality associated with injuries.[4,5]Trauma registry surveillance systems provide pertinent information that can be used to prevent trauma and also improve efficiency and quality of trauma care.[5,6]An understanding of the epidemiology of trauma gives insights into the nature and extent of the problem,identifies risk factors for injury, and highlights trauma care areas that require quality improvement. This information can then be used to set priorities for intervention and facilitate evidence based decision making, policy planning and development of good trauma care systems.
Trauma registries in many developed countries are recognized as one of the vital tools in providing useful information that helps enhance trauma care.[7-9]Most LMICs do not have injury surveillance systems that can generate reliable information on the nature and extent of injuries to assist in designing appropriate interventions that achieve the greatest impact in preventing and improving quality of care for injuries. While tremendous resources are consumed caring for injured patients at hospitals in LMICs, less attention is directed toward gaining a better understanding of the burden of injuries,quality of trauma care and the impact of prevention strategies through establishment of trauma registries.[10]Routine data collection may exist but tends to be inadequate in content and quality to improve trauma care.[8,11]Trauma registries would complement routine data collection to provide quality and content rich injury information.[8]
The establishment of a trauma registry where none previously existed is a challenging task, especially in LMICs.[12]Trauma registries established in Uganda,Ethiopia, Nigeria and Haiti have shown the practical feasibility in LMICs.[13-15]
Malawi is among LMICs with fragmented injury data and no injury surveillance system at a national level, as such the true burden of injuries in the country is not known. There have been some efforts by some institutions to improve injury surveillance in the country with an aim of improving injury prevention and trauma care. Kamuzu Central Hospital (KCH), a referral facility in the central region of the country has an established injury surveillance system of all trauma patients seen at the hospital.[16,17]However there was no well-established trauma registry at Queen Elizabeth Central Hospital(QECH), the largest tertiary and teaching hospital in the country which manages severe trauma cases from Southern and Eastern regions of the country and less severe cases from areas located near to the hospital.
This paper describes the implementation process of a trauma registry at QECH and reports the findings from the registry which was established with an aim of capturing data to help understand the epidemiology of trauma in Malawi and assist in informing injury prevention and improve trauma care. It also highlights mapping of the data to identify high risk locations for trauma and suggests ways in which trauma care can be improved at QECH and surrounding health centres.
METHODS
Setting
A modern Adult Emergency Trauma Centre (AETC)was opened in October 2011 at Queen Elizabeth Central Hospital. The trauma unit provides adult trauma, medical emergency and gynecological emergency care. Paediatric patients are managed at a separate unit within the hospital. AETC trauma care services include evaluation of new trauma cases, review of old trauma cases requiring secondary or tertiary care, and medical report compilation for all trauma cases occurring in Blantyre district requiring police investigation or undergoing insurance claims. This registry limited its implementation to collection of information for only new trauma cases seen by clinicians in the unit.
The trauma care is offered in three designated areas:(1) trauma assessment room and procedure room for mild to moderate injuries, as well as reviews; (2) resuscitation room for major injuries; (3) short stay ward is used for major incidence when there are more than 10 injured patients coming into the unit at the same time.
Most of the trauma care is provided by medical assistants, clinical officers, nurses and intern medical doctors. Medical assistants are a cadre of clinicians who undergo a two-year training post-secondary school and are awarded a certificate in clinical medicine;while clinical officers earn a three-year post-secondary diploma in clinical medicine. During the time of the implementation of trauma registry project there was only one full time medically qualified emergency medicine specialist who was in charge of the unit.
Data capture form
A two-page data capture form was developed from a trauma care sheet that had been used in AETC since December 2011. The form was piloted and necessary changes made. The form captured demographic information, mechanism of injury information, relevant medical history and examination (primary and secondary survey) findings, injury type and location, treatment offered and disposition of patient. The form was printed on self-carbonated papers and was completed in duplicate. One paper was collected by the data clerks at the end of every day to be used for electronic data capture, whereas the other paper either remained in the patient’s file for admitted cases or remained in the AETC for patients treated as outpatients.
Personnel and training
Consultative meetings were held with AETC clinicians to discuss how trauma data collection could be organized in the department. They recommended the addition of clerks to capture patient demographic information and mechanism of injury data while the clinicians would continue to enter clinical, injury diagnosis, management and disposition information.
Ten clerks working in AETC underwent training on how to complete the trauma data form and also capture data electronically from filled forms. Each one of them received a supplemental remuneration of $15 USD per month during the registry project period. All clinicians working in AETC also underwent training to ensure competency in completing the form. Clinicians did not receive any financial incentives.
Equipment
Four digital sphygmomanometers and 4 pulse oximeters were purchased and used in the unit for blood pressure and oxygen saturation measurements respectively. Two desktop computers were also purchased and used for electronic data capturing. An external drive was purchased and used for back up of data.
Data collection and entry
The first section, which had demographic data,arrival information, and injury information (such as time of injury and mechanism of injury) was completed by data clerks. The second section, which had findings on primary and secondary survey, past medical history,clinical diagnosis, procedures performed and disposition,was completed by clinicians. In cases of multiple injury,clinicians were asked to record the type and location of three most severe injuries identified and document the total number of severe injuries the patient had sustained.At the end of each day, the data clerks collected all completed forms and 2 data clerks were assigned to enter the data daily onto a Microsoft Excel[18]spreadsheet.
The data was then analysed using Microsoft Excel and Stata Version 15.0.[19]Descriptive statistics was done to determine frequencies of the variables. Chi square test was used to determine statistical significance of associations between the 2 categorical variables.Multivariate logistic regression was used to determine characteristics associated with being admitted. Variables included were age, gender, season, mechanism of injury,injury type and transport used by victims of trauma to come to hospital. These variables were identified from the literature.[20,21]Crude and adjusted odds ratios with 95% confidence intervals were reported. Results were considered to be statistically significant if thePvalue was less than 0.05.
Hot spot analysis of the geographical locations where there were high numbers of incidents of injury(injury hotspots) was done using the hot spot analysis tool in ArcGIS[22]software where spatial relationships of our location grouped injury cases were conceptualised using the inverse distance method. In the inverse distance method, cases or features close to each other have a greater in fluence on each other than those that are away from them. The cut-off value for distance used in this study was 6520.29 meters which was calculated using the incremental spatial autocorrection tool. At this distance all participating cases had at least one neighbour and spatial clustering was more pronounced. Ethical approval was obtained from the University of Malawi, College of Medicine Research Ethics Committee.
Funding
The trauma registry project was supported financially by the Health Partnership Scheme funded by the Tropical Health and Education Trust (THET) funded by the UK Department for International Development (DFID).
RESULTS
The AETC provided trauma care to 5,282 newly injured patients from May 2013 to May 2015. This trauma registry had 3,747 trauma cases recorded during this period, representing a 70.9% rate of data collection for the targeted population. In the resuscitation room,976 (18.5%) injured patients were not captured whereas in the trauma assessment room, 559 (10.6%) were not captured.
Demographic and injury characteristics
The majority of the patients (79.1%) were males. The average age was 32 years (SD 12) and age range of 13 to 89. More than a third of the cases (39.8%) occurred in age group of 21 to 30 years (Table 1). The average time taken from injury to arrival at hospital was 3.5 hours(SD 4.1 hours) and the average time taken from arrival at hospital to being seen by a clinician was 3.9 hours (SD 1.3 hours). The majority of patients (75.9%) were treated as outpatients. Only 14.3% were admitted to the wards.
The most common mechanism of injury was assaults(38.2%), followed by RTIs (31.6%). In the road traffic injuries, the majority were pedestrians (36.2 %). Gun shot wounds (0.3%) and burns (0.4%) were not common in the 2-year period that the data was collected. The most common diagnosis of injury was soft tissue injury(53.1%), however about 23.8 % had no diagnosis (Table 1).
The commonest mode of transport for the injured person to get to the hospital was by minibus (51.6%)and private vehicle (24.7%). Only 3.4% arrived by ambulance. The majority of the cases occurred on the road/street (41.7%) followed by home (26.1%) and workplace (18.1%) (Table 1). A third (33.4%) of the cases were were intentional. Of note, 10.9% of all injuries were in flicted upon by either an intimate or domestic partner.

Table 1. Demographic and injury characteristics details
Bivariate analysis (Table 2), showed that female trauma patients were more likely to be admitted than males (OR1.26, 95%CI[1.01-1.7]). Falls had higher odds of being admitted compared to road traf fic accidents(OR1.38, 95%CI[1.06-1.8]). Assault cases were less likely to be admitted as compared to road traffic accidents (OR0.55; 95%CI[0.44-0.69]). Both fractures(OR19.98, 95%CI[15.66-25.48]) and head and internal organ injuries (OR30.49, 95%CI[17.11-54.35]) had much higher odds of being admitted as compared to soft tissue injuries. Furthermore, those that were brought by an ambulance had higher odds of being admitted compared to those who were brought in by public transport (OR2.1, 95%CI[1.55-2.84]).
Multivariate analysis found that fractures, head injury and internal organ injury, and use of ambulance were found to be predictive of increased odds of being admitted to hospital while assault was found to be associated with less odds of being admitted to hospital(Table 2).
Variable completion rates
We achieved excellent completion rates for demographic and injury details with more than 90%completion rate for almost all variables.
Diagnosis details were not completed in 23.8% of cases. Procedure performed or treatment received was not completed in 27.2% of the cases. Disposition was not completed in 9.9% of cases.
Whereas completion of secondary survey details was high for most variables, primary survey details had poor completion rates. More than a third of the patients (30.6%) had no documentation of cervical spine examination and immobilization details. Vital signs recording was poor with more than 40 % having no recording of temperature, pulse rate, blood pressure;worst being respiratory rate (79.5%) and oxygen saturations (89.0%). Table 3 summarises the challenges identified during the implementation of the trauma registry.
Source of cases and hot spot analysis
The majority of patients (88.7%) were self referrals to Queen Elizabeth Central Hospital. Blantyre is split into several geographic locations or neigbourhoods. Hot spot analysis showed that at 99% confidence interval,Ndirande, Mbayani and Limbe locations were the top three most hot spots for injury occurrence (Figure 1).At 95% confidence interval, Chirimba and Blantyre city central were additional hot spots. These are all high density poor urban townships within Blantyre.
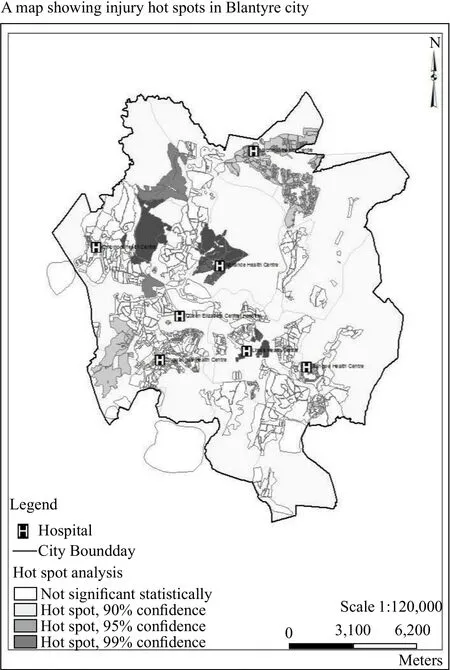
Figure 1. Injury hotspots in Blantyre city.
DISCUSSION
In the two years that this trauma registry has run,we have demonstrated that with minimal resources, we can run a trauma registry at our hospital. Our aim was to establish a trauma registry that is integrated in the routine clinical care of our trauma patients. Therefore our data set was quite comprehensive to ensure data capturing of injury information while providing standardised clinical review and management of the trauma patient. We also ensured that the trauma registry was incorporated into the unit’s routine data collection system by utilising unit staff members.

Table 3. Challenges identified in establishing trauma registry at QECH and recommendations for improving data capturing

Table 2. Disposition in 3,379 adult trauma patients according to age, gender, mechanism of injury, seasonal variation, transport mode and injury type
The completion rates for the demographic and injury details completed by data clerks were very high. This reduced the amount of data that needed to be completed by few clinicians in a busy emergency department especially with the rising burden of trauma on health workers.[25]
Even with the high completion rates of demographic and injury details by data clerks, the biggest challenge,however, was incomplete clinical data collection by clinicians working in the AETC; prominently seen in the primary survey and diagnosis. Such variability of completion rates were also shown in a trauma registry in Cape Town, South Africa.[26]Low completion rates are unacceptable for prospectively collected data. Possible reasons could be that our form was too long compared to other trauma registry forms and so, while we achieved our aim of integrating routine clinical care, the quality of the collected data was compromised. Coded/ tick box options are preferred to write out diagnosis of injures and facilitate the reduction of transcription errors that occur from illegible handwritings. Frequent clinician training on the trauma form was done, but the effect was compromised by a high turnover rate for clinicians and heavy dependence on not readily available locum clinicians. The trauma care services offered in the unit are very diverse resulting in heavy patient loads that could compromise clinician capacity to fill in trauma information adequately. There is need for a focus group discussion with the clinicians to establish reasons for the poor completion rates, and a review of the amount of data needed. Other registry experiences report the benefit of having a minimum trauma data set in high patient burden settings[27]and it is worth considering this in future to improve the quality of data collected. Furthermore, efforts should be made to ensure data capturing happens in all areas where trauma care is offered in the unit. Of particular note was the low completion rates for the vital signs.The reasons for these are not clear but lack of enough measuring equipment for those vital signs that require special equipment, time constraints and lack of appreciation of the importance of documenting vital signs could have contributed. There is need for further research to find out reasons for poor completion rates of vital signs and solutions provided to improve this.
Despite the low completion rates for some variables,we were able to analyse variables that were relatively well completed, such as the address of injury and time taken from injury to arrival. The majority of the patients came straight to QECH bypassing their “nearest” health centres (primary care facilities) with soft tissue injuries which can be easily managed at the health centre level.Furthermore the majority of patients were treated as outpatients suggesting that they had minor injuries which could be managed at the health centre level. The hot spot analysis showed that the identified hot spots have a health centre nearby where patients can receive care.It is possible that in practice these health centres do not operate 24 hours and are therefore inaccessible for cases that occur after working hours. Another explanation for the by-pass phenomenon is that there is inadequate capacity to manage trauma cases and therefore patients who have received inadequate care previously prefer to go to the central hospital. Furthermore, the centralization of legal medical report compilation for Blantyre district promoted the by-pass phenomenon. There is therefore need to strengthen the referral system or improve trauma care capacity in the health centres located in the hotspots.Such an initiative could ease the workload on the referral hospital and other referral hospitals in the region with similar constraints and free up resources to concentrate on the more serious injuries. A study to establish reasons why people bypass the health centres will help in strengthening the referral system.
As seen from this study, the average waiting time for a patient to be seen by a clinician was 3.9 hours;this waiting time could be significantly reduced if there is less workload. This timeframe is within the 4 hour established waiting period for clinical review for nonurgent cases in the unit and could have influenced the response to the patients presenting with minor nonlife threatening injuries categorized as “non- urgent” at triage in the unit. This study notes that urgent/emergency cases seen in the resuscitation area were not adequately captured to identify the pattern of responsiveness to major injuries. There is need for a study to look into factors that in fluence waiting times at AETC.
The average time taken from injury to arrival at hospital was 3.5 hours. Patients have the best chance of survival if they reach a trauma center within one hour of injury.[28]Reducing the travel distance from the spot of injury to a health facility is pertinent. Strengthening identified three health centers near hotspots to injury locations would help to compel patients to utilize them and shorten travel times, resulting in better trauma care outcome.
The long time taken to reach hospital, also reflects deficient pre-hospital trauma care. The majority of patients arrived by private transport either by a minibus or private vehicle. This is an opportunity to offer first aid training to minibus drivers so that they are able to provide care to injured persons either on the scene or enroute to hospital, thereby improving trauma care. In addition making it compulsory for all drivers to have mandatory first aid training before getting a driving license will also help, as they are among the first responders when an injury happens, whether it is road traffic related or otherwise. Future studies should also look at what proportion of injured patients, especially assault cases, report to police first before going to seek medical treatment. If most assault cases present to police first, then there could be benefit in training police in first aid.
One of the important decisions in the ED is the disposition of the patient. Our study looked at disposition of injuries from all causes of trauma. We found that fractures, internal injury and patient transported on ambulance were significantly associated with a greater likelihood of admission. These patients are likely to be severely injured. However, a study in Cameroon found no significant factors predictive of admission to ward, but Injury Severity Score of >9 was found to be predictive of death, transfer to intensive care unit and transfer to the operating room.[20]Once predictors of admission have been identified, the next step would be to identify prognostic factors in admitted patients in our setting that would help to come up with interventions to improve outcomes.
An alternative to paper based trauma registry is an electronic trauma registry. The experience from Karachi, Pakistan,[29]where they implemented an electronic trauma registry was that it was expensive and that it requires an environment where there is already electronic health information system with a backup of IT experts. It is also time-consuming. It took 23 months for the development of the Karachi trauma registry from the concept to the operational software.Entering data directly on an iPad or tablet has a steep learning curve and may be challenging for a clinician working in a busy clinic or with limited computer skills.However direct electronic databases have the advantage of saving stationery and printing costs and obviating the problem of a backlog of paper forms not captured into the electronic database because of other reasons. In our study, the two clerks who were assigned to capture the data electronically were the only ones among the other clerks who felt confident to do the job. We had a problem of a backlog of completed paper forms waiting to be captured electronically, especially at the beginning of the study as their entry rate was slow. This improved with time, however there were still some instances when either one or both were not on duty, which caused buildup of completed forms. This problem could have been averted if we had used direct electronic capturing using either an iPad or a tablet. In addition direct electronic capturing can be designed in such a way that one can only proceed to the next questions after completing the index question. This will ensure high completion rates thereby improving the quality of the data which were also sub optimal in our study.
Limitations
Our study had several limitations. The calculation of Injury Severity Score was hampered by the incomplete information entered in the medical records. In a study by Samuel et al[30]done at Kamuzu Central Hospital, only 11 of 63 charts had enough data in order to calculate an RTS or TRISS. We advocate the use of the Kampala trauma score in our setting which is easier to use. One technique that has been suggested to circumvent the underreporting from primary data sources is the capture-recapture data through utilization of more than two data sources.[31]
The registry did not include paediatric cases as these have their own accident and emergency department in a separate building of the hospital. Future initiatives should include an all-inclusive trauma registry so that we will have data for all age groups. A total of 29.1% of trauma patients were not recorded in the registry, the majority of which were from the resuscitation area. Resuscitation area patients are usually serious injured patients sometimes with life threatening injuries who need urgent resuscitation as a life saving measure. These patients are usually entered into the registry after resuscitation and stabilisation. It is possible that the data clerks and clinicians forgot to capture these patients after the initial resuscitation or before the patients were transferred to other units such as intensive care or theatre for further emergency management. This limitation resulted in underreporting of admitted and severely injured cases in the registry.
CONCLUSION
This study has described the process of establishing an integrated and potentially sustainable hospital based trauma registry in an urban adult emergency department located in a low income country. Despite the limitations and challenges, significant trauma data were captured to provide details on the epidemiology of trauma cases seen at the hospital and high risk geographic locations thereby giving some insight to the type of trauma care offered and how care could be improved at AETC and surrounding health facilities. The approach followed in Malawi may be relevant in similar poor resource settings.
Funding:The trauma registry project was supported financially by the Health Partnership Scheme funded by the Tropical Health and Education Trust (THET) funded by the UK Department for International Development (DFID).
Ethical approval:Ethical approval was obtained from the University of Malawi, College of Medicine Research Ethics Committee.
Conflicts of interest:Authors have no financial or other conflicts of interest related to this submission.
Contributors:LC and WM proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
 World journal of emergency medicine2019年1期
World journal of emergency medicine2019年1期
- World journal of emergency medicine的其它文章
- Information for Readers
- World Journal of Emergency Medicine
- Venous thromboembolism in the emergency department: A survey of current best practice awareness in physicians and nurses in China
- The use of outcome feedback by emergency medicine physicians: Results of a physician survey
- Rapid sequence induction (RSI) in trauma patients:Insights from healthcare providers
- Comparison between intravenous morphine versus fentanyl in acute pain relief in drug abusers with acute limb traumatic injury
