Determination of vitamin D and analysis of risk factors for osteoporosis in patients with chronic pain
Bao-Lin Duan, Yuan-Rong Mao, Li-Qi Xue, Qing-Yuan Yu, Mei-Yi Liu
Bao-Lin Duan, Yuan-Rong Mao, Li-Qi Xue, Qing-Yuan Yu, Mei-Yi Liu, Department of Pain,Qinghai Provincial People’s Hospital, Xining 810000, Qinghai Province, China
Abstract
Key words: Chronic pain; Vitamin D deficiency; Bone mass reduction; Osteoporosis;Bone mineral density
INTRODUCTION
Chronic pain is one of the most challenging clinical problems for clinicians. Patients with chronic pain not only have to endure somatic pain but also bear a huge psychological burden due to behavioral responses. Some studies have demonstrated that vitamin D deficiency is associated with non-specific musculoskeletal pain[1], knee osteoarthritis[2], migraine[3], chronic cervical pain[4], and other multiple chronic pains. It is also a risk factor for various chronic diseases such as osteoporosis, hypertension and cardiovascular disease[5].
Vitamin D deficiency is not only present in patients with chronic pain but also a common phenomenon in healthy populations. It is estimated that more than 50% of the world’s population have vitamin D deficiency[6]. A recent multi-center survey in China showed that the prevalence of vitamin D deficiency in Chinese urban residents is approximately 55.9%[7]. Vitamin D is a pro-hormone that regulates the calcium (Ca)and phosphorus (P) balance and skeletal structures. Vitamin D deficiency increases the risk of osteoporosis[8]. The occurrence of osteoporosis is a silent and imperceptible process, and is often ignored until fragile fracture occurs. For osteoporotic patients,early detection, diagnosis and treatment are of primary importance. Currently, the diagnosis of osteoporosis mainly depends on bone mineral density (BMD) measured by dual-energy X-ray absorptiometry. Many studies have reported the relationship between vitamin D and BMD, but the conclusions are controversial.
The aim of the present study was to determine the changes in vitamin D level in patients with chronic pain, clarify the relationship between vitamin D and BMD, and explore the risk factors for bone mass reduction and osteoporosis in patients with chronic pain, in an attempt to provide experimental clues for the prevention and treatment of osteoporosis.
MATERIALS AND METHODS
General data
In this study, 184 patients with chronic pain who were admitted to the Pain Department of Qinghai People’s Hospital (Xining, China) between May and September 2017 were enrolled. These patients consisted of 49 males and 135 females with a mean age of 57.62 ± 13.79 years. An additional 104 healthy individuals who underwent routine health checkups in the same hospital during the same period were enrolled as controls, including 25 males and 79 females with a mean age of 56.52 ±13.66 years. According to the BMD test results, the patients in the study group were further classified into three subgroups: Normal BMD group (n= 55), reduced BMD group (n= 74) and osteoporosis group (n= 55). The exclusion criteria were as follows:Patients with endocrine and autoimmune diseases; malignant tumors; chronic liver disease, chronic obstructive pulmonary disease and chronic kidney disease; sequelae of cardio-cerebrovascular disease affecting extremity function; skin diseases who could not be exposed to sunlight; those using active vitamin D, steroids, sex hormones, parathyroid hormone (PTH), calcitonin, diphosphate and other drugs that may affect bone metabolism within 6 mo before initiation of the study.
The research protocol was approved by Qinghai People’s Hospital, and informed consent was obtained from all participants in the study on the principle of voluntary participation. Of the initially recruited 346 patients with chronic pain, 103 patients with complicated autoimmune, cardiovascular, endocrine and chronic kidney diseases, malignant tumors, and those who had a history of using anti-osteoporosis drugs or Ca supplements, and 59 patients who lacked BMD, PTH and other key data were excluded from the study. In total, 184 patients were included in this study for analysis.
Methods
Criteria for test index evaluation:Venous blood samples were collected at 7:00-8:00 AM from all participants under fasting conditions and sent to our laboratory for analysis. 25 hydroxy vitamin D (25OHD) and PTH were measured by a Cobas 8000 electrochemiluminescence immunoassay kit. Ca and P levels were detected using an automatic biochemical analyzer and the required kit (Hitachi. Japan). BMD of the L-1-4 and femoral neck, Ward’s triangle and trochanter was measured by dual-energy Xray absorptiometry (Hologic Q DR 2000, United States). Other general data of the participants including age, height, weight, body mass index (BMI), living altitude,past medical history and drug administration were also recorded for analysis.
The vitamin D status was assessed by measuring the serum level of 25OHD, and was classified as severe vitamin D deficiency (< 10 ng/mL), vitamin D deficiency (≥ 10< 20 ng/mL), vitamin D insufficiency (≥ 20 < 30 ng/mL), and vitamin D sufficiency (≥30 ng/mL).
The criteria for BMD assessment were as follows: Patients with a BMD T value > 1 in any of the L1-4, total hip and femoral neck were included in the normal BMD group, -1 to 2.5 were included in the reduced BMD group, and ≤ -2.5 were included in the osteoporosis group.
The criteria for PTH assessment were as follows: Serum PTH < 15 pg/mL was considered reduced, ≥ 15 pg/mL ≤ 65 pg/mL was considered normal, and > 65 pg/mL was considered increased.
The criteria for P assessment were as follows: Serum P < 0.85 mmol/L was considered reduced, ≥ 0.85 mmol/L ≤ 1.51 mmol/L was considered normal, and >1.51 mol/L was considered increased.
The criteria for Ca assessment were as follows: Serum Ca < 2.2 mmol/L was considered reduced, ≥ 2.2 mmol/L ≤ 2.7 mmol/L was considered normal, and > 2.7 mol/L was considered increased.
Statistical analysis
All statistical analyses were performed using SPSS 17.0. Quantitative data are expressed as x± s. Comparisons between two groups were performed using the independent sample t test; comparisons between three groups were performed by one way ANOVA; and comparisons between multiple groups were performed by LSD.Counting data are expressed asc2. Two sets of ordered counting data were analyzed by Mantel-Haenszel test for linear trend. Risk factors were analyzed by binary logistic regression. Values ofP< 0.05 were considered statistically significant.
RESULTS
Comparison of the general data and vitamin D concentrations between the study and control groups
Comparisons of the general data indicated no significant difference in age and sex between the two groups. The vitamin D concentration in the study group was significantly lower than that in the control group (P <0.05) (Table 1).
Comparison of the percentage of vitamin D concentration between the study and control groups
Vitamin D deficiency was predominant in both groups, accounting for 53.8% and 57.7%, respectively, with no significant difference between the two groups. The proportion of patients with severe vitamin D deficiency in the study group was significantly higher than that in the control group (P< 0.05) (Table 2).
Comparison of vitamin D concentrations between the normal BMD group, reduced BMD group and osteoporosis group, and the diagnostic value of vitamin D concentration on osteoporosis
Two-group comparisons showed a significant difference in age between the normal BMD, reduced BMD and osteoporosis groups, with the oldest patients in the osteoporosis group and the youngest in the normal BMD group. There was no significant difference in sex between the three groups. The vitamin D level in the osteoporosis group was lower than that in the other two groups (Table 3).
The area under the receiver operating characteristic curve of vitamin D concentration in the reduced BMD and osteoporosis groups was 0.487 and 0.417,respectively, suggesting that it was significant for the diagnosis of bone mass reduction and osteoporosis (Table 4, Figure 1).
Relationship between BMD and vitamin D concentrations in terms of age in the study group
The relationship between age and BMD was analyzed by the Mantel-Haenszel chisquare test, and the results showed a linear correlation between age and BMD in patients with chronic pain (c2= 58.933,P< 0.001). Pearson correlation analysis showed that R = 0.567 andP< 0.001, indicating that BMD decreased gradually with increased age in chronic pain patients (Table 5).
There was no significant difference in vitamin D change between the different age groups in the study group (P> 0.05) (Table 6).
Analysis of risk factors for bone mass reduction in the study group
Ten factors including age, sex, ethnicity and BMI in the normal and reduced BMD groups were analyzed by univariate analysis and the results showed that age, sex,ethnicity, PTH and Ca showed statistical significance (P <0.05) (Table 7).
Of the above results, age, sex, ethnicity, PTH, and Ca were entered into binary logistic analysis, and the results showed that age, PTH and Ca were risk factors for bone mass reduction (Table 8).
Analysis of risk factors for osteoporosis in patients with chronic pain
Univariate analysis of 10 factors including age, sex, ethnicity and BMI in the osteoporosis and normal BMD subgroups showed significant differences in age, sex,ethnicity and altitude between these two subgroups (P <0.05) (Table 9).
Of the above results, age, sex, ethnicity and altitude were entered into binary logistic analysis, and the results showed that age, ethnicity and altitude were risk factors for osteoporosis (Table 10).
DISCUSSION
Vitamin D is a hormone synthesized in the skin during sunlight exposure. It not only participates in bone and cellular metabolism but plays a role in the regulation of autoimmune disease, inflammation, neuromuscular and other immune functions.During the process of vitamin D metabolism, serum 25OHD concentration is the optimal marker for evaluating vitamin D status[9]. A number of studies have demonstrated the deficiency or insufficiency of vitamin D in multiple chronic pain disorders including non-specific musculoskeletal pain, chronic generalized pain,fibromuscular pain, lower back pain, headache and lumbar canal stenosis. In addition,the results of vitamin D surveys in healthy populations worldwide are not optimistic,with the prevalence of vitamin insufficiency reaching 30%-50%[10]. In the presentstudy, it was found that vitamin deficiency was generally present in both chronic pain patients and healthy individuals, although the overall vitamin D level in chronic pain patients was lower than that in healthy individuals, especially in those with vitamin D deficiency or severe vitamin D insufficiency. Some studies showed that vitamin D supplements could alleviate pain[11-14]. However, three meta-analyses found no significant correlation between vitamin D supplementation and pain relief in their randomized study and placebo control groups[15-17]. Serum 25OHD concentration is affected by multiple host and environmental factors, including age, sex, diet, sunlight exposure, physical activity, body weight, skin pigmentation, and genetic factors.Whether there is a relationship between vitamin D deficiency/severe insufficiency and chronic pain requires further studies.
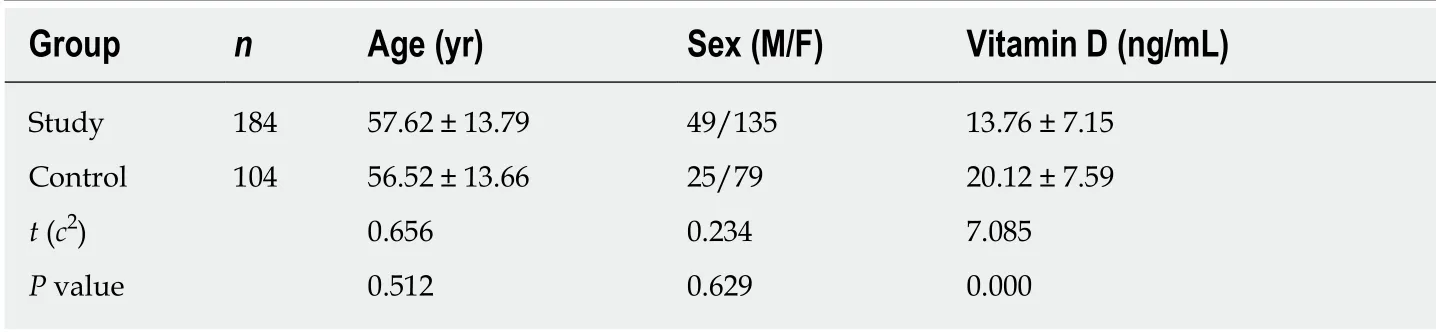
Table 1 Comparison of the general data and vitamin D concentrations between the study and control groups
Vitamin D is a pro-hormone that regulates Ca and P balance and skeletal structures, and has an adverse impact on skeletal health and neuromuscular function.Vitamin D deficiency increases the risk of osteoporosis. Serum 25OHD level lower than 20 ng/mL was reported to be associated with defective bone mineralization[8,18].In our study, it was found that vitamin D concentration was lowest in osteoporotic patients but was not a risk factor for bone mass reduction and osteoporosis,suggesting that they are not correlated. This finding is consistent with the results of a large-scale cross-sectional study conducted in Northwest China[19]. However, the role of vitamin D in the basic treatment of osteoporosis should not be questioned. A large number of studies have confirmed that vitamin D alone cannot reduce the risk of bone fracture, but combined use of vitamin D and Ca supplements can reduce the risk of hip and non-vertebral fractures[20-22]. The anti-osteoporosis treatment guidelines from multiple different countries and regions maintain that sufficient Ca uptake plus the vitamin D status is a precondition of any regimen for the prevention and treatment of osteoporosis regardless of which drug is used[23-25]. Thus, questions arise as to what amount of vitamin D supplementation can maximally increase the serum 25OHD concentration and at the same time ensure that the concentration will not be excessive? In other words, what is the optimal vitamin D supplement concentration required for the 25OGD target for general populations? One study set up the general practical criteria and the latest suggestions for preventive administration of vitamin D for newborns, infants, children, adolescents and adults (including pregnant women,lactating mothers and older people) in central European areas, in which the vitamin D concentration < 20 ng/mL is defined as deficiency, 20-30 ng/mL as the sub-healthy state, and 30-50 ng/mL as the optimal target concentration of vitamin D action and the range of serum 25OHD concentration. It also suggests that all individuals with serum 25OHD lower than 20 ng/mL should be supplemented or corrected for vitamin D, and 30 ng/mL is the target most suitable for infirm, osteoporotic and senile patients[26].
Osteoporosis is one of the main health concerns worldwide. With increasing age,bone mass decreases gradually, leading to bone mass reduction and osteoporosis. The differential diagnosis of bone mass reduction and osteoporosis is based on the BMD level. The main goal of osteoporosis screening and treatment is to prevent fracture by reducing bone mass loss. It is therefore extremely important to recognize risk factors associated with bone mass change in order to identify high risk populations and take early preventive strategies to reduce the occurrence of osteoporosis. With increasing age, the risk of bone mass reduction and fracture is generally increased, especially in menopausal women whose estrogen level and liver/kidney function in synthesizing active vitamin D are both reduced, leading to reduced absorption of Ca in the gut. In addition, a reduction in estrogen level activates PTH, thus increasing the activity of osteoclasts, increasing bone absorption, and quickening bone turnover and bone mass loss. As a result, the bone trabecula becomes thinner, the bone cortex is structurally damaged and becomes progressively thinner, and the bone density is decreased.Undoubtedly, age is an important risk factor for bone mass change, which isconsistent with related reports[23]. What is different is that we failed to find a significant correlation between bone mass loss and BMI. Lifestyle factors associated with the risk of osteoporosis include alcohol consumption, diet, hormones, sports and smoking. In addition, Ca and vitamin D are extremely important in age-related BMD and skeletal muscle mass reduction[27]. It was observed in our study that PTH and Ca were risk factors contributing to bone mass reduction, while ethnicity and altitude were risk factors contributing to osteoporosis. Whether this phenomenon is due to the relatively small sample size or reflects intrinsic differences remains to be confirmed in future studies.
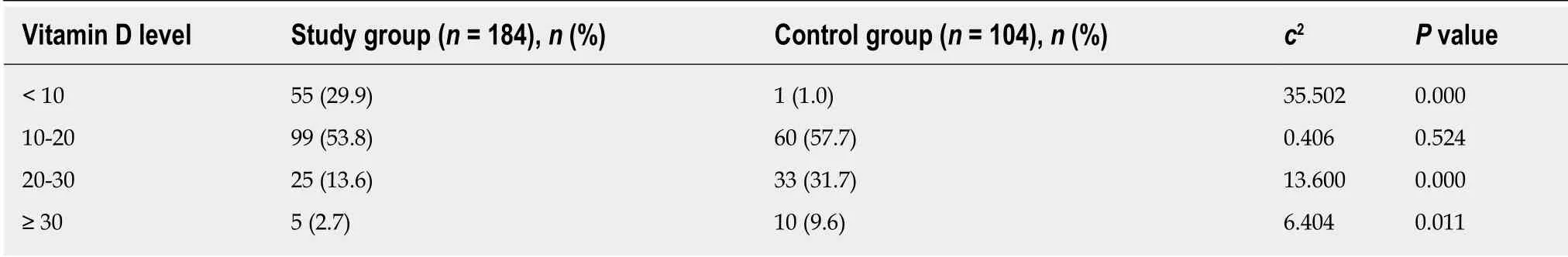
Table 2 Comparison of the percentage of vitamin D concentration between the study and control groups
Multiple individual factors should be considered in the treatment of osteoporosis.Personalized treatment strategies should be built on disease severity, patient sex,complications and adverse effects that the drug(s) may produce[28]. Differences in related risk factors should also be included in the selection of therapies.
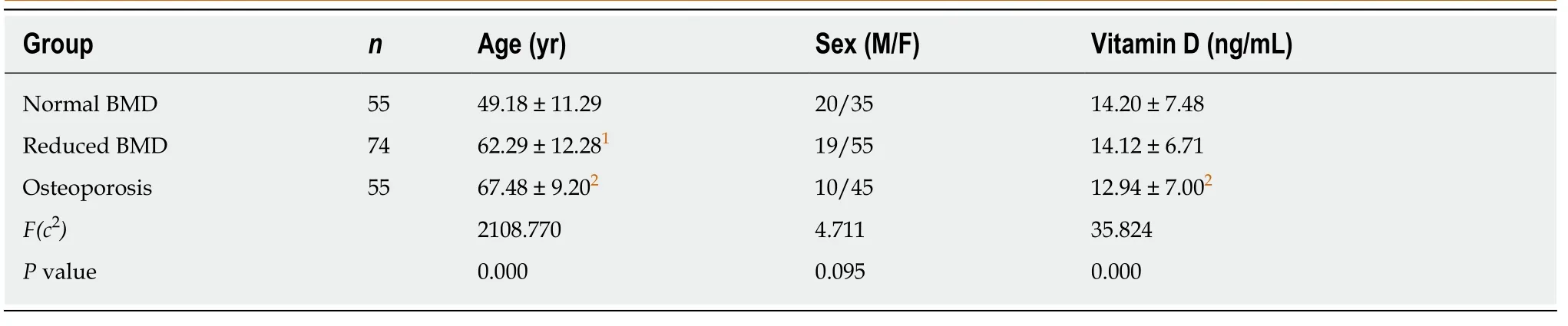
Table 3 Comparison of vitamin D concentrations between the normal bone mineral density group, reduced bone mineral density group,and osteoporosis group
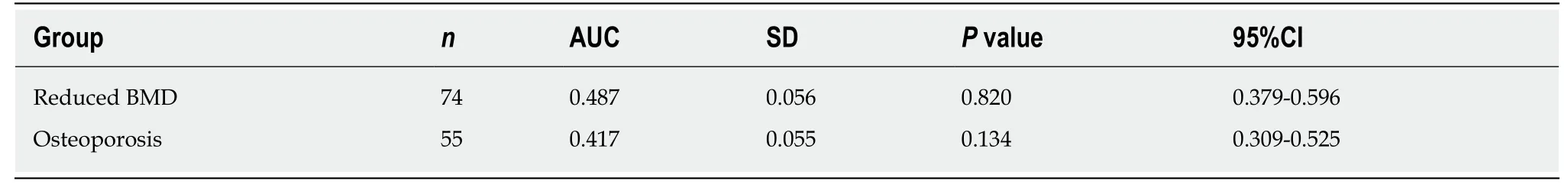
Table 4 The diagnostic value of vitamin D concentration on bone mass reduction and osteoporosis

Table 5 Relationship between age groups and bone mineral density in patients with chronic pain

Table 6 Comparison of vitamin D concentrations between different age groups in the study group
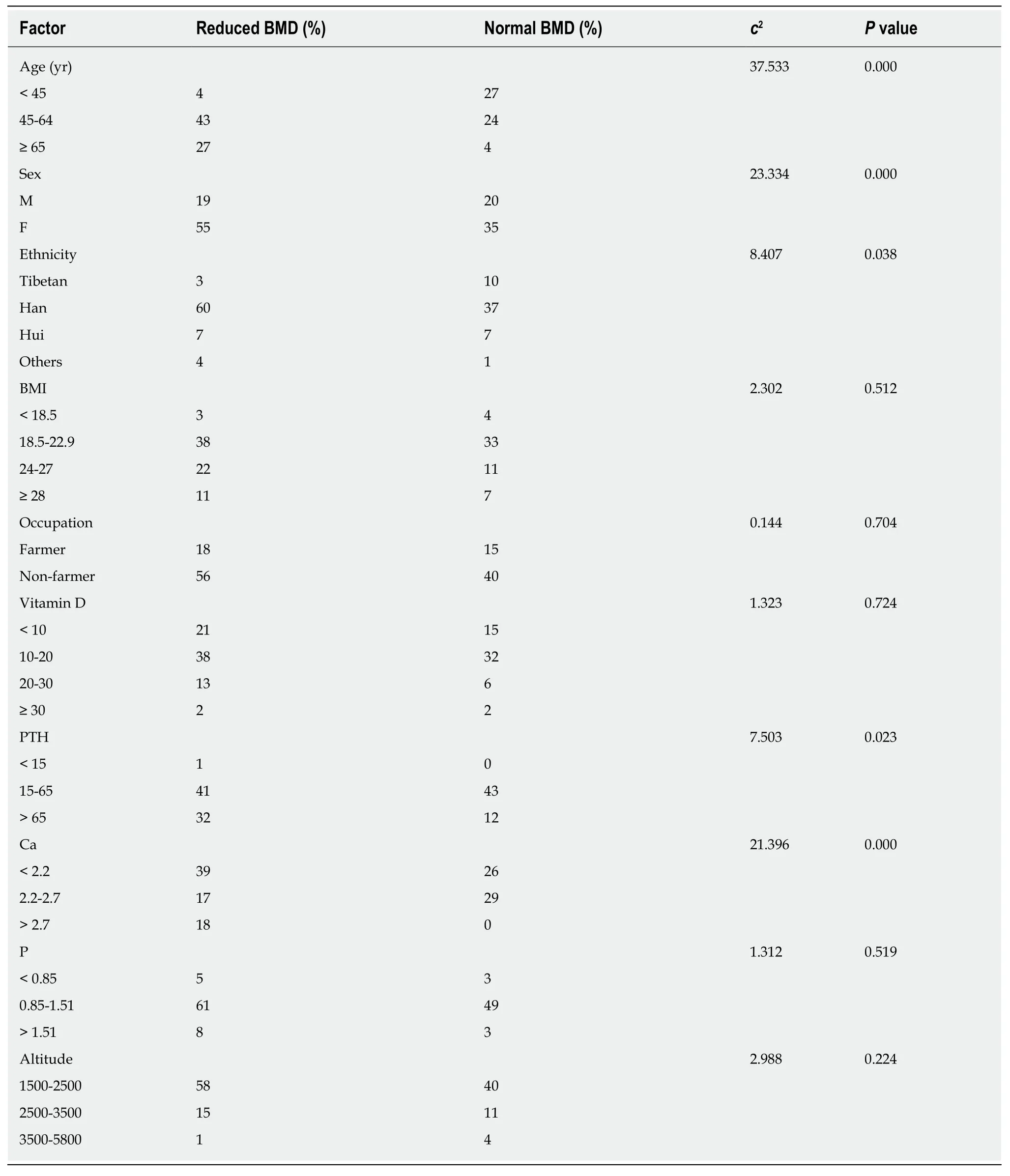
Table 7 Univariate analysis of various factors in the normal and reduced bone mineral density groups of the study group
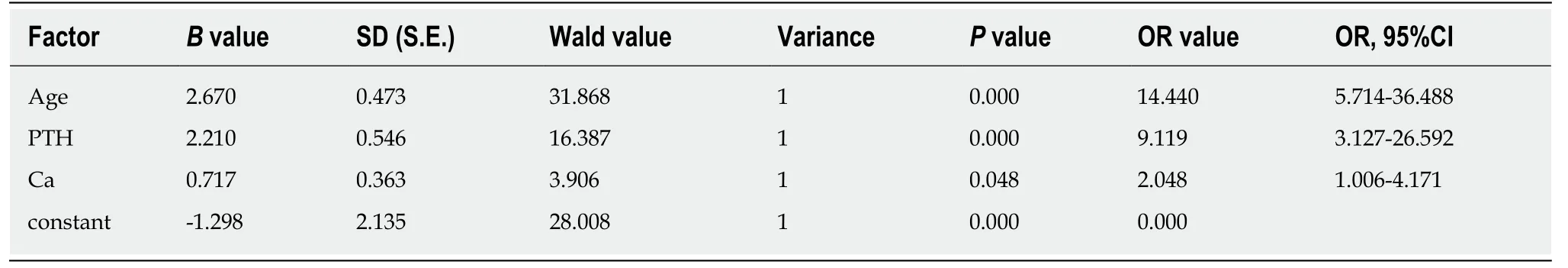
Table 8 Binary logistic analysis of multiple factors for bone mass reduction

Table 9 Univariate analysis of multiple factors in the osteoporosis and normal bone mineral density subgroups of the study group
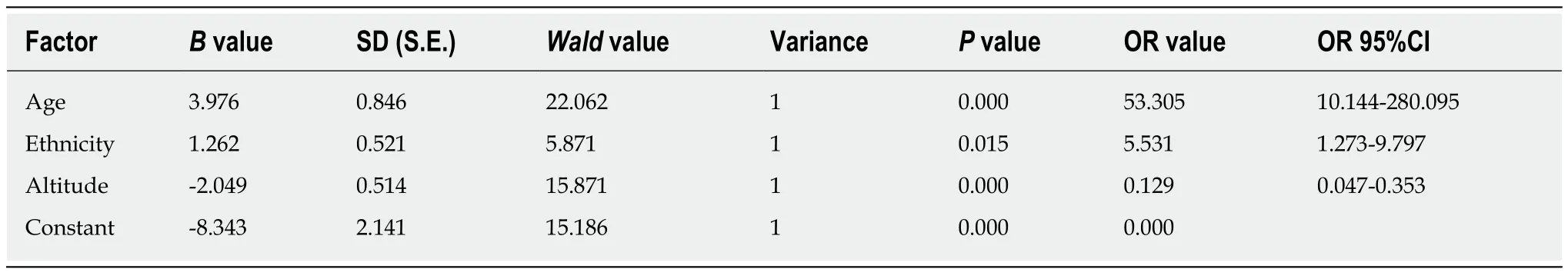
Table 10 Binary logistic regression analysis of multiple factors for osteoporosis
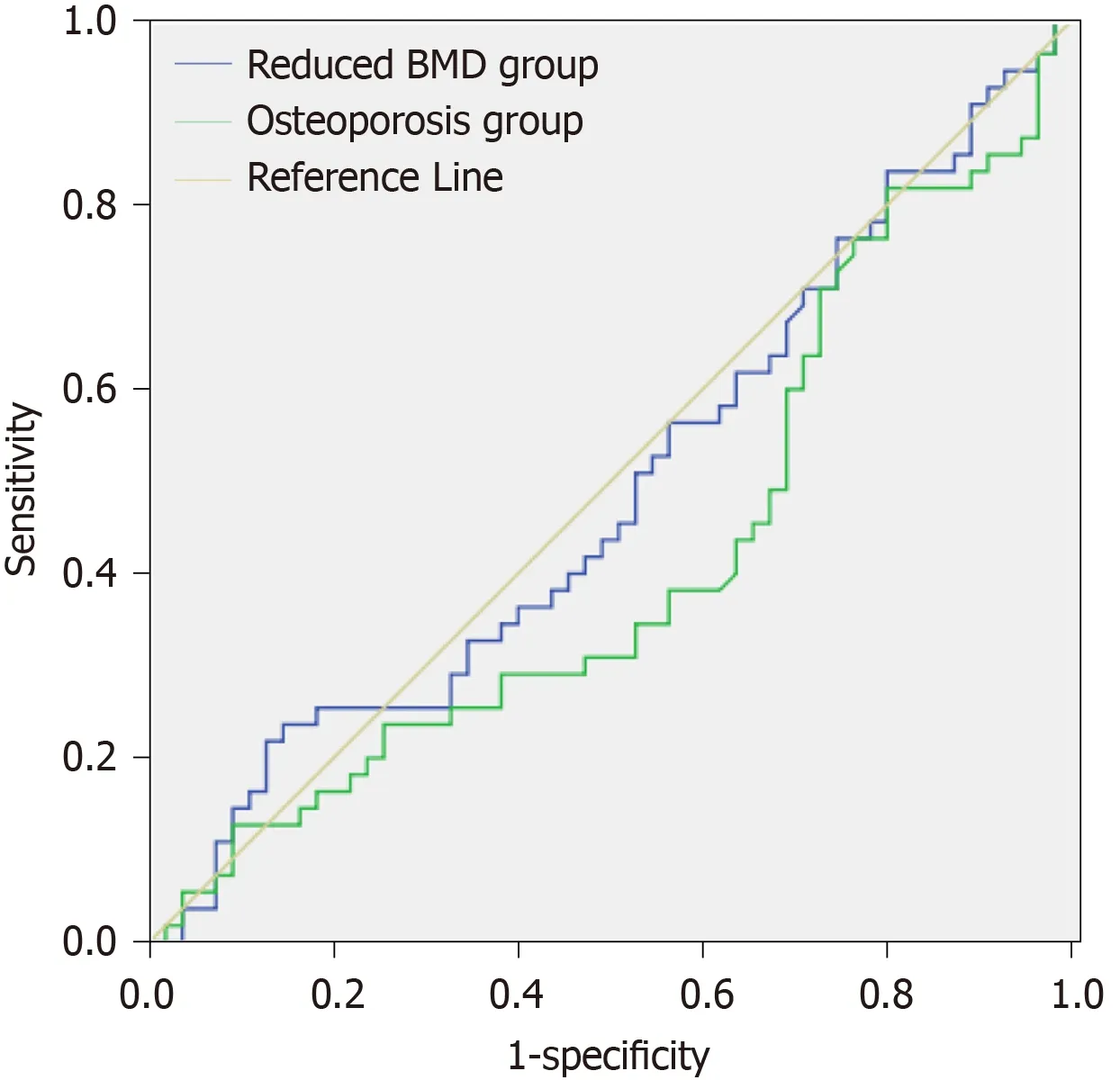
Figure 1 The diagnostic value of vitamin D concentration on bone mass. BMD: Bone mineral density.
ARTICLE HIGHLIGHTS
Research background
Vitamin D deficiency is common in chronic pain patients and healthy people, but the difference between the two has not been reported. The relationship between vitamin D, chronic pain and bone mineral density (BMD) is controversial. The aim of the present study was to observe changes in vitamin D levels in patients with chronic pain, clarify the relationship between vitamin D and BMD, and explore risk factors for bone mass reduction and osteoporosis.
Research motivation
To understand the relationship between vitamin D and chronic pain, clarify the relationship between vitamin D and bone density, analyze the risk factors of bone mass reduction and osteoporosis, and provide a basis for early treatment of osteoporosis.
Research objectives
Vitamin D deficiency is very common in patients with chronic pain and healthy people, but severe vitamin D deficiency is more likely to occur in patients with chronic pain. Vitamin D is not a risk factor for bone mass changes. Age, parathyroid hormone (PTH) and calcium (Ca) were risk factors for bone mass reduction, while age, ethnicity and altitude were risk factors for osteoporosis.
Research methods
25 hydroxy vitamin D and PTH were determined by a Cobas 8000 electrochemical luminescence immunoassay kit. Ca and P levels were detected using a fully automated biochemical analyzer and the relevant kit (Hitachi). BMD of l-1-4, femoral neck, Ward's triangle, and femoral trochanter was measured by dual-energy X-ray absorptiometry. General patient information was collected including age, height, weight, body mass index, altitude of residence, previous medical history and medication use. All statistical analyses were performed using SPSS 17.0. Quantitative data are expressed as x ± s. Comparisons between two groups were performed using the independent samplettest; comparisons between three groups were performed by one way ANOVA; and comparisons between multiple groups were performed by LSD. Counting data are expressed asc2. Two sets of ordered counting data were analyzed by the Mantel-Haenszel test for linear trend. Risk factors were analyzed by binary logistic regression. Values ofP< 0.05 were considered statistically significant.
Research results
Both chronic pain patients and healthy people were mainly deficient in vitamin D, but the proportion of severe vitamin D deficiency in chronic pain patients was significantly higher than that in the healthy group. Patients with chronic pain were more likely to suffer from vitamin D deficiency or severe deficiency, the causes of which require further study. The levels of vitamin D in the osteoporosis group were lower than those in the groups with normal bone mass and reduced bone mass, but vitamin D levels were not a risk factor for changes in bone mass. Age,PTH and Ca were risk factors for bone mass loss. Age, sex, ethnicity, and altitude were risk factors for osteoporosis.
Research conclusions
Vitamin D deficiency is common a mong patients with chronic pain, and severe vitamin D deficiency is more likely to occur. Although vitamin D levels are lowest during osteoporosis,they are not a risk factor for changes in bone mass. According to the different risk factors of bone mass change, independent treatment methods can be adopted clinically.
Research perspectives
Chronic pain patients are more likely to have severe vitamin D deficiency, and the reason for this is not clear. Vitamin D is not a risk factor for osteoporosis. Whether vitamin D supplementation is beneficial requires further study. Whether early monitoring of PTH and Ca levels has an effect on the prevention of bone mass change, and which age group can effectively prevent osteoporosis requires further investigation.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
