CerebrospinaI fluid biomarkers in idiopathic normaI pressure hydrocephaIus
Xin-Jie Zhang, Jian Guo, Jun Yang
Department of Neurosurgery, Xiang'an Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen 361102,Fujian, China.#Authors contributed equally.
Abstract Idiopathic normal pressure hydrocephalus (iNPH) is characterized by abnormal cerebrospinal fluid (CSF) flow and consequent cerebral ventricular enlargement due to imbalance of CSF production and absorption.The typical triad symptoms, namely cognitive decline, gait disturbance, and urinary incontinence, are thought to be caused by disruption of CSF circulation.However, some patients may still experience symptomatic progression after functional shunting, suggesting that iNPH is far more complicated than a simple disorder of CSF circulation.Moreover, the diagnostic workup of iNPH can be challenging due to symptomatic and neuroimaging overlaps with other neurological disorders, such as Alzheimer's disease.Furthermore, accumulating studies indicate that the pathogenesis of iNPH might relate to multiple mechanisms, including abnormalities of brain development, brain extracellular matrix, synaptic function, blood flow, and cerebral metabolism.Therefore, iNPH is not an isolated entity in occurrence and development.Nevertheless, different pathogeneses may result in protein content changes in CSF, and the biomarkers in CSF may reflect the possible mechanisms involving the etiology of iNPH and are potentially useful in assisting the diagnosis and treatment selection.In this review, we summarize the main findings of CSF biomarkers and aim to outline a possible synthetic profile in assisting iNPH diagnosis and therapeutic options.
Keywords: Idiopathic normal pressure hydrocephalus, cerebrospinal fluid, biomarkers, neurodegenerative diseases
INTRODUCTION
Idiopathic normal pressure hydrocephalus (iNPH) is one of the disabling neurological disorders whose potential treatability is significantly impacted by the timeliness of unequivocal diagnosis.iNPH is characterized by ventriculomegaly that is caused by an imbalance between cerebrospinal fluid (CSF)production and absorption.The characteristic triad symptoms of dementia, gait disturbance, and urinary incontinence are thought to be caused by a disruption of CSF dynamics[1,2].Therefore, the triad symptoms of iNPH could be surgically treatable with a diversion of CSF into peritoneal cavity or heart[3].However,the diagnostic workup of iNPH can be a challenge due to neuroimaging and symptomatic overlaps with other neurological disorders, such as Alzheimer's disease (AD) and subcortical ischemic vascular disease,especially at early stage.Moreover, although the cognitive decline could be proceeded by these diseases,they are not equally responsive to the treatment of CSF shunting.Therefore, further effort to improve the diagnosis of iNPH would benefit the current imaging and symptomatic diagnostic criteria.Increasing studies indicate that the pathogenesis of iNPH involves multiple mechanisms, including abnormalities of brain development, brain extracellular matrix, synaptic function, blood flow, and cerebral metabolism,which could result in protein content changes in CSF.On the other hand, impaired CSF absorption could lead to a pathological flow of CSF into the periventricular tissues to initiate a cascade of pathological processes such as edema and consequent neuronal degenerative changes[4].Therefore, measurements of different biomarkers in CSF may reflect the underlying neuropathological changes of the brain and could play an important role in revealing the possible etiological mechanisms.Furthermore, its detection may facilitate the timeliness and accuracy of iNPH diagnosis, and thus becomes potentially useful for therapeutic selection and treatment response monitoring.In addition, the biomarkers could help to differentiate iNPH from other neurological disorders, which might mimic iNPH symptomatology but show unsatisfactory outcomes after shunting[5,6].Despite a growing interest, the CSF biomarker profile in iNPH has not yet been identified definitively.In this review, we summarize the main findings of CSF biomarkers regarding iNPH and outline a rough CSF profile in order to assist iNPH diagnosis and provide adequate treatment.It is notable that, due to the etiological complexity of iNPH, most biomarkers might lack specificity for iNPH diagnosis and are possibly coincidental, confounding with other overlapping neurological diseases.In addition, in comparison with a cortical brain biopsy or neuropsychological testing, biomarkers may also have limitations in distinguishing iNPH from comorbid iNPH plus AD[7], as well as in predicting clinical cognitive outcome post shunting[6,8,9].However, a combination of more than one biomarker may enhance the predictive value and provide more viable and accurate solutions.Ideally,the dynamic changes of biomarker measured before and after surgical diversion of CSF would supply useful clinical information for the diagnosis and assistance in monitoring disease progression.The biomarkers could be categorized as AD discrimination, neurodegeneration and demyelination, neuroinflammation,neuropeptides and cerebral metabolites, and as biomarkers in response to cerebral and vascular insulting,among others[1,2,10,11].
BIOMARKERS FOR AD DISCRIMINATION
Dementia in iNPH is potentially reversible if adequately treated.However, it often resembles the clinical appearance of patients with AD, such as memory decline, as well as attention and executive impairment[12].Urinary incontinence and gait disturbance may also occur in both diseases due to disturbed subcortical network caused by vascular pathology.Moreover, ventricular enlargement may have been observed in AD patients as a result of cerebral atrophy rather than CSF circulation impairment[13].Furthermore, the pathological examination of cortical brain biopsies performed during placement of CSF shunts revealed AD neurodegenerative changes in 24% of iNPH patients, suggesting a high comorbidity of both diseases.Thus,cortical brain biopsy may provide a valuable predictive way for outcome evaluation[6,8].However, cortical brain biopsy is not always available or appropriate in some cases.Moreover, both iNPH and AD diseases may manifest sleep disturbances, which correlate with dysfunction of the glia-lymphatic (glymphatic)system, consequently building-up of brain metabolic wasters, favoring dementia development[14,15].Therefore, it is always a challenge to discriminate iNPH and AD diseases in clinical practice.
The glymphatic system facilitates cerebral metabolite and brain fluid clearance during sleep via gliasupported perivascular channels.This system facilitates efflux of cerebrospinal and interstitial fluid via the perivascular spaces to the meningeal and cervical lymphatic vessels, assisting the draining/clearing of metabolic wastes from the central nervous.The glymphatic flux is proposed to be driven by cardiacinduced arterial pulsation[16], and may be possibly manipulated through change of intracranial pressure pulsatility with our cardiac-gated device[17].Most interestingly, the action of glymphatic flux is predominant during sleep[18], and up to 90% of iNPH patients are associated with obstructive sleep apnea, a common sleep disorder[19].Blockage of the airway in obstructive sleep apnea causes increased awakenings and decreased quality of sleep, resulting in glymphatic dysfunction and increased cerebral Ab aggregation[20].Patients with obstructive sleep apnea encounter reduced oxygen intake due to intermittent airway obstruction.Excessive breathing against a closed airway induces negative intrathoracic pressure, sufficient to cause atrial distortion and reduced venous return to the heart[19]and ultimately affect arterial pulsation,resulting in dysfunction of glymphatic flux.
Many studies have shown impaired glymphatic function in both iNPH and AD.Furthermore, iNPH and AD patients share multiple clinical and pathologic features such as Ab deposition, cerebrovascular inflammation, impaired localization of perivascular astrocyte aquaporin-4 (AQP4), and sleep disturbances[15].Therefore, it is a diagnostic challenge in daily practice for iNPH and AD.Although many biomarkers have been investigated for their discrimination, amyloid-b 42 (Ab42), total-tau (t-tau),and phosphorylated tau (p-tau) are the most robust candidate markers to discriminate iNPH from AD patients[1,2].Ab42is lower in both iNPH and AD patients compared with healthy control, and Ab42does not separate iNPH and AD.Tau protein is a microtubule-associated protein and is a marker for neuronal degeneration[21].The levels of t-tau and p-tau are higher in AD patients compared with iNPH patients and controls, whereas the levels of t-tau and p-tau are within normal range in iNPH patients.The combination of these biomarkers, i.e., the reduced Ab42with concomitant normal or reduced t-tau and p-tau levels in iNPH coupled with reduced Ab42with concomitant increased both t-tau and p-tau levels in AD,may significantly improve the accuracy of differential diagnosis between AD and iNPH patients[22].The mechanism of lower Ab42level in iNPH patients is unknown.However, the reduced production of Ab42due to a decline in brain metabolism in the periventricular zone in iNPH patients[23,24]and interstitial Ab deposition due to impaired glymphatic function may be possible reasons[15].Meanwhile, the low concentrations of CSF t-tau and p-tau do not support the major cortical degenerative process in iNPH[24,25],whereas, in AD patients, the core pathological changes are the accumulation of abnormally folded betaamyloid and tau proteins in the plaques and neuronal tangles[26], and the progressive deposition of amyloid plaques lowers Ab42level.Moreover, concurrent axonal degenerations and neurofibrillary tangle formation further increase t-tau and p-tau CSF levels in AD patients[27].The representative information and main biomarkers for assisting differential diagnosis of iNPH and AD are summarized in the attached Table 1.
NEURODEGENERATION AND DEMYELINATION
The disturbance of CSF circulation could lead to a potentially hostile milieu for cerebral structures,especially periventricular areas and subcortical structures, and could result in vascular lesions, destruction of periventricular white matter, and subsequent neurodegeneration and demyelination[28-30].Such pathological changes could be estimated with the examination of CSF contents, such as neurofilament light chains (NFL), myelin basic protein (MBP), and leucine-rich-α2-glycoprotein (LRG)[31-33].NFL is a cytoskeletal element in nerve axons and dendrites, and therefore could be considered as a biomarker for axonal damage in patients with iNPH[31,34].Although some studies did not find difference of CSF NFL levels between iNPH and AD patients[11,32], as well as controls[35], other studies demonstrated increased CSF NFL levels, and the increase paralleled the degeneration of large myelinated axons in iNPH[31,36].In addition, some studies observed that the ventricular NFL level directly correlated with altered signals in periventricular white matter in brain MRI[37].Moreover, one study demonstrated that high preoperative NFL level was associated with favorable surgical outcomes, and suggested that NFL could possibly be used as an indicator for neurodegeneration and a marker of ongoing axonal damage[38].

Table 1.The representative information and biomarkers in iNPH and AD
Demyelination of the periventricular white matter could occur in hydrocephalus due to the result of mechanical stretching.MBP is an oligodendroglial structural protein of myelin and sulfatide is a glycosphingolipid component of myelin, and they are essential for the maintenance of central nervous system myelin and axon structure[32,39].Both MBP and sulfatide are well known indicators for ongoing demyelination and therefore are attractive markers for the pathological process[40].However, the CSF levels of MBP are higher in many different neurologic disorders, including iNPH and cerebrovascular diseases,leading to lack of specification for iNPH diagnosis[32,36], whereas it is demonstrated that changes of MBP levels are correlated with periventricular white matter damage[41].When comparing the levels of MBP preand post-shunting, the results showed that the levels of MBP decreased post-shunting, suggesting that MBP could be used for evaluation of brain damage and shunting effect[42].
LRG is an astrocytic protein and could be induced by inflammation.The LRG level in CSF increases with age in iNPH and other dementia diseases.It was speculated that the accumulation of LRG in the brains is one of the causes of neurodegeneration, therefore its level in CSF could be an anticipated marker for early diagnosis of iNPH and other dementia diseases[33,43].
Taking together, all these markers allow tracking the integrity of periventricular and subcortical structures.Although they are not disease specific, their changes in CSF directly reflect cerebral damage, and they may be useful indicators in comparative analyses between iNPH and other neurodegenerative diseases.
NEUROINFLAMMATION
Cytokines mediate inflammatory response and often correlate with neurodegeneration in neurological diseases.The profile of CSF cytokines provides access to explore the pathogenic mechanisms of different neurological diseases and therapeutic approaches[44].Abundant CSF cytokines have been investigated in iNPH patients, but a more definite profile still needs to be clarified[32,36].
Tumor-necrosis factor (TNF-α) is a cytokine of inflammatory mediator and its level in CSF is significantly high in iNPH patients[45,46].Most interestingly, the CSF level of TNF-α returned to the control level in the patients with shunt improvement.Because of its short half-life, the increased CSF TNF-α may be caused by increased production rather than the accumulation due to CSF stagnation, which suggests that TNF-α in CSF might be used as a candidate marker for the evaluation of demyelination and disease progression in iNPH patients.More studies are needed for validation.
Transforming growth factor b1(TGF-b1), one of the three cytokines in the TGF family, plays a role in cell differentiation and tissue modification during brain development.It could be released from microglia and astrocytes in response to cerebral insult to initiate neuroinflammation and neurodegeneration through the induction of fibrosis, vascular hypertrophy, accumulation of extracellular matrix components, and neuronal apoptosis[47-49].TGF-b level was found to be higher in iNPH patients than controls, and was considered to be a reliable index of cerebral damage in iNPH[49].
Other increased inflammatory biomarkers measured in iNPH patients include IL-1b and IL-6 (proinflammatory cytokines), IL-10 (anti-inflammatory cytokine), tissue factor pathway inhibitor 2 (TFPI-2),chitinase-3-like protein-1 (YKL-40), and monocyte chemoattractant protein (MCP-1)[50-52].However, as similar changes are also observed in AD and Parkinson's disease, these changes only reflect an underlying neuroinflammatory processes of pro-inflammatory reaction (IL-1b and IL-6) and compensatory antiinflammatory reaction (IL-10), rather than disease-specific indicators[44,51,52].TFPI-2 is involved in inflammatory process by recruiting astrocytes and microglia to the injury site[50].YKL-40 is then released from astrocyte and/or microglia in response to neuroinflammation.The increased CSF YKL-40 levels seem to be correlated with cognitive decline and therefore to predict progression of dementia[53].However, more studies are deserved on the clinical use of this novel promising neuroinflammation biomarker[35,48].
NEUROPEPTIDES AND CEREBRAL METABOLITES
Neuropeptides, including somatostatin, vasoactive intestinal peptide, neuropeptide Y, and delta-sleep inducing peptide, have been evaluated by various groups[10,54,55].Decreased CSF somatostatin levels suggest damage to the hypothalamus and the cortical neurons that normally have high concentrations of somatostatin[54].Higher level of somatostatin correlates with better visual memory and mental condition in iNPH patients, proposing that somatostatin may have a modulatory role in cognition[10].Vasoactive intestinal peptide is a potent vasodilator and therefore may play a role in chronic ischemia, and the CSF level is usually higher in iNPH patients with cerebrovascular disease[55-57].Delta-sleep inducing peptide is a nine-amino acid peptide with a role in sleep-wakefulness regulation.iNPH patients with lower delta-sleep inducing peptide level show worse psychomotor performance[56].Several studies also reported reduced levels of neuropeptide Y in iNPH patients[54-56].Cerebral metabolism changes may occur in iNPH patients.iNPH patients were also reported to have altered levels of lactate, an end product of anaerobic glycolysis underlying a presence of chronic ischemia[58,59].Free-radical peroxidation could result in cellular dysfunction and may therefore be implicated in the pathogenesis of iNPH and dementia.A study showed that the levels of free-radical peroxidation products significantly increased in iNPH patients[60].The authors implied that peroxidation of cytoplasmic membranes might be involved in the development of cognitive dysfunction in iNPH.
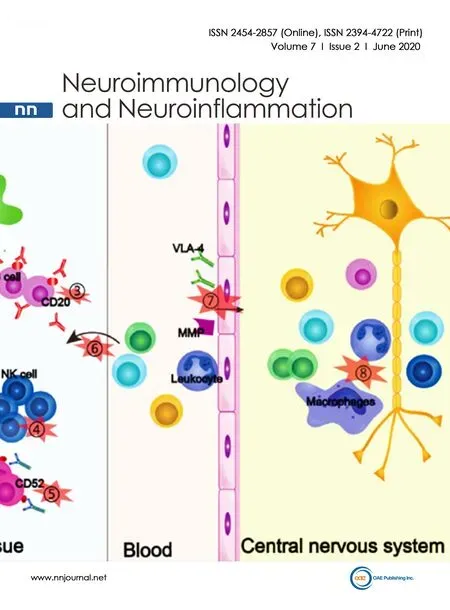
BLOOD-BRAIN BARRIER CHANGE AND BIOMARKERS RESPONDING TO CEREBRAL AND VASCULAR INSULTING IN INPH
Blood-brain barrier is a physically powerful gateway that strictly monitors and controls the interchange of substances between central nervous system and blood flow[61].Its function is strictly dependent on the integrity of microvascular endothelium and thus affected by many pathophysiological risk factors,including vascular/hemodynamic changes, inflammation,etc., and in turn affects the homeostasis of central nervous system[62].The “CSF/blood albumin ratio” represents a reliable index of blood-brain barrier function.Blood-brain barrier impairment was reported in different neurodegenerative diseases, including AD and cerebral vascular disease[63].Nowadays, it has been scarcely evaluated in iNPH patients, but available reports indicate a substantial preservation of the blood-brain barrier[22,36].
Vascular risk factor may be a component of subcortical neuropathology in the development of iNPH[2].As key components, cerebral white matter lesions and hypertension were reported to be related to the pathophysiology of iNPH[64-66].White matter lesions, involved in different cognitive processes and/or clinical outcomes, are associated with small vessel disease and white matter ischemia.The association between iNPH and white matter lesions indicates the involvement of microvascular disturbances in the white matter and in the pathological processes of iNPH.In addition, hypertension increases the risk of iNPH through the mechanisms of involved small vessel diseases, including hypertension induced endothelial damage and resultant extravasation of blood products into white matter, impaired blood flow with reduced metabolism, and direct mechanical effect on ventricular size[66,67].Therefore, identifications of vascular related risk factors may improve diagnostic accuracy and address the underlying pathology regarding the development of iNPH, and ultimately provide suitable intervention for iNPH management.Overall, the dynamic and morphological alterations in subcortical structure of iNPH brain could be resulted from white matter lesions, hypertension related vascular lesions, destruction of periventricular white matter axons and gliosis, and impaired CSF circulation[28].Such pathological alterations could affect CSF protein contents and biomarkers in CSF could mirror the underlying pathologic alterations.As markers of subcortical damage, at least three proteins have been measured in iNPH patients, including NFL, LRG, and MBP[1].The functions and clinical application of these proteins are discussed above.In summary, NFL is a cytoskeletal protein for maintenance of axonal architecture and is considered as a marker for neuronal morphological integrity[31].Although it has also been assessed as a biomarker for inflammatory and neurodegenerative diseases, it has been observed that ventricular NFL levels in iNPH patients directly correlate with more extensive altered signals in periventricular white matter in brain MRI[1].LRG is an astrocytic protein and is increased in CSF of iNPH patients, suggesting a potential biomarker for iNPH, but it also changes with aging and non-specific inflammation[68].MBP is an oligodendroglial structural protein of myelin.Its CSF levels are increased in iNPH patients and other cerebrovascular and neurodegenerative diseases, indicating the damage of periventricular white matter[1,32].
In addition, nerve growth factor (NGF) play an important role in neuro-regeneration in response to brain injury and age-related atrophy.NGF is scarcely detectable in innervated tissues, but denervation of cerebral tissue could lead to the production of NGF and become measurable in the target tissues[69].The CSF level of NGF was found to be significantly higher in hydrocephalus patients compared with the controls[70], which suggests the possibility that the increased NGF levels could represent an increased cerebral regeneration after shunting.
Vascular endothelial growth factor plays roles in many cerebral physiological and pathological modifications, and its level in CSF is respondent to ischemic condition involved in different neurological disorders[59,71-73].Our group demonstrated that the CSF levels of vascular endothelial growth factor in iNPH patients have circadian variations and exercise induced increasing[74].The higher concentration of vascular endothelial growth factor level in CSF is associated with less response to shunting and worse clinical outcome, suggesting a possible concurrent ischemic or vascular injury in iNPH patients[73,75].
Glial fibrillary acidic protein is a marker for gliosis[34,76].In iNPH patients, the CSF level of glial fibrillary acidic protein was increased when compared with controls, and correlated with disease progression[38].The increased glial fibrillary acidic protein level in CSF suggests an irreversible damage to astrocytes, since glial fibrillary acidic protein is not secreted by astrocytes.
All of these markers suggest the involvement of vascular risk factors and consequent subcortical white matter lesions in the development of iNPH; however, further studies are needed to explore their predictive value in clinical application.
OTHER BIOMARKERS AND METHODOLOGICAL IMPACT ON CSF BIOMARKER DETECTION
The level of prostaglandin D synthase was found to be significantly lower in iNPH patients compared with controls and other dementia patients, such as Lewy body dementia, vascular dementia, and AD[77].This enzyme is secreted into CSF by the leptomeninges and the trabecular cells of the arachnoid membrane.The authors speculated that the decreased level of prostaglandin D synthase was probably due to a degenerative change of the arachnoid membrane in iNPH patients.
Finally, the methodology of CSF biomarker detection may also affect the ability to reliably evaluate biological biomarkers for the differentiation and prognosis of cognitive impairment diseases[78].Many factors may affect the reliability and sensitivity of biomarker detection, for example, the systematic difference between different assays, different pre-analytical protocol for sample preparation and storage,analytical variability of measurement procedures,etc.[79,80].When interpreting measurement results, these factors should be considered.In addition, some biomarkers exhibit periodic concentration patterns.Therefore, the most appropriate time for sample collection must also be considered when designing a protocol[79].
CONCLUSION
The overlap of neuroimaging and symptomatic manifestations leads to diagnostic confusion between iNPH and other neurodegeneration diseases, such as AD and subcortical ischemic vascular disease.Despite the absence of definite pathological hallmarks, the biomarkers altered in CSF might serve as targets for diagnosis and therapeutic intervention.Furthermore, the biomarkers in CSF could reflect the adjacent cerebral pathophysiological status, therefore are potentially useful to provide insight into the pathological changes in the brain milieu and underling pathogenesis.Although many CSF biomarkers have been analyzed in iNPH patients, the significant findings include the reduced Ab42with concomitant normal or reduced t-tau and p-tau levels in iNPH coupled with reduced Ab42with concomitant increased both t-tau and p-tau levels in AD.This characteristic alteration may significantly improve the accuracy of differential diagnosis between AD and iNPH patients.Other biomarkers may lack specification in differential diagnosis, but the definite changes may mirror the underlying pathogenesis mechanisms, such as demyelination, neurodegeneration, and neuroinflammation, and provide valuable information to further explore the pathogenesis mechanisms and optical therapeutic manipulations.
DECLARATIONS
Authors' contributions
Conceived of the presented idea: Yang J
Underwent literature review and synthesized a draft: Yang J, Zhang XJ, and Guo J
Contributed ideas throughout the process and approved the final draft: Yang J
Looked over and edited draft: Yang J, Zhang XJ, and Guo J
AvaiIabiIity of data and materiaIs
Not applicable.
FinanciaI support and sponsorship
None.
ConfIicts of interest
All authors declared that there are no conflicts of interest.
EthicaI approvaI and consent to participate
Not applicable.
Consent for pubIication
Not applicable.
Copyright
© The Author(s) 2020.
 Neuroimmunology and Neuroinflammation2020年2期
Neuroimmunology and Neuroinflammation2020年2期
- Neuroimmunology and Neuroinflammation的其它文章
- Favorable and unfavorable roles of microglia and macrophages in the pathologic central nervous system
- BiIirubin and inflammation in neurodegenerative and other neuroIogicaI diseases
- COVID-19 neurotropism and implications for therapy
- An association between mitochondria and microglia effector function: what do we think we know?
- Phf15 - a novel transcriptional repressor regulating inflammation in a mouse microgIiaI ceII Iine
- AUTHOR INSTRUCTIONS
