血清瘦素及可溶性瘦素受体在诊断非酒精性脂肪肝合并肝纤维化中的价值
龚尚红 曹雨石 郑小蝶 秦芳怡 杜晓晨 徐巧本
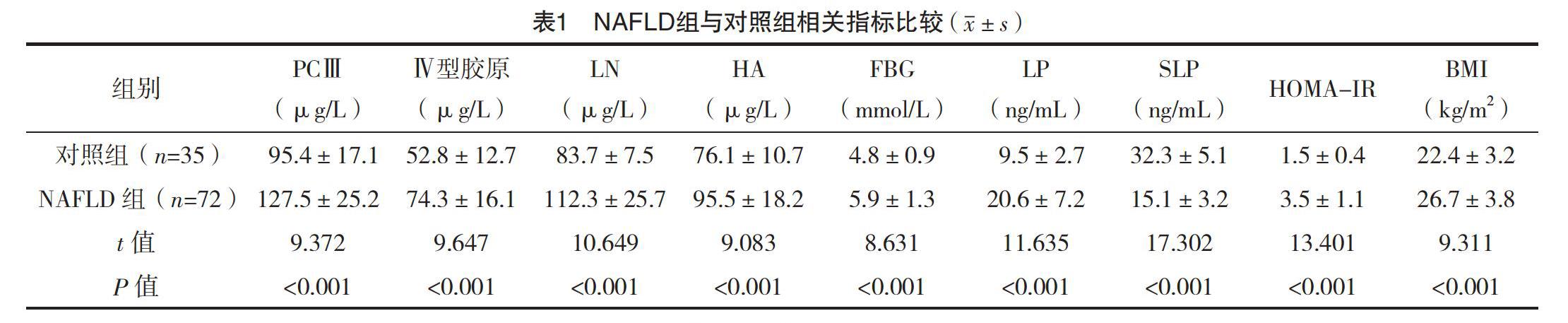

【摘要】 目的:观察血清瘦素(LP)及可溶性瘦素受体(SLP)在诊断非酒精性脂肪肝(NAFLD)合并肝纤维化中的价值。方法:选取2018年5月-2019年5月本院收治的72例NAFLD患者作为NAFLD组。同期选择35例本院门诊健康体检者作为对照组。根据非酒精性脂肪性肝纤维化评分(nonalcoholic fatty liver disease fibrosis score,NAFLDFS)将NAFLD组分为NAFLD无肝纤维化组(A组,NAFLDFS<-1.455,45例)与NAFLD伴肝纤维化组(B组,NAFLDFS≥-1.455,27例)。检测并比较各组血清LP、SLP、Ⅲ型前胶原(PCⅢ)、Ⅳ型胶原、层黏蛋白(LN)、透明质酸(HA)及血清空腹血糖(FBG);计算并比较各组胰岛素抵抗指数(HOMA-IR)、NAFLDFS及BMI。分析上述血清学指标诊断NAFLD患者合并肝纤维化的价值。结果:NAFLD组血清PCⅢ、Ⅳ型胶原、LN、HA、FBG、LP水平及HOMA-IR、BMI均明显高于对照组,而血清SLP水平明顯低于对照组(P<0.05);B组血清PCⅢ、Ⅳ型胶原、LN、HA、FBG、LP水平均明显高于A组,而血清SLP表达水平明显低于A组(P<0.05),两组HOMA-IR、BMI比较,差异均无统计学意义(P>0.05);LP、SLP诊断NAFLD患者合并肝纤维化的AUC、敏感度及特异度均优于PCⅢ、Ⅳ型胶原、LN、HA、FBG。结论:血清LP及SLP在诊断NAFLD合并肝纤维化方面具有较好的临床价值。
【关键词】 瘦素 可溶性瘦素受体 非酒精性脂肪肝 肝纤维化
The Value of Serum LP and SLP in the Diagnosis of Non-alcoholic Fatty Liver Disease with Liver Fibrosis/GONG Shanghong, CAO Yushi, ZHENG Xiaodie, QIN Fangyi, DU Xiaochen, XU Qiaoben. //Medical Innovation of China, 2021, 18(13): 0-064
[Abstract] Objective: To observe the value of serum LP and SLP in the diagnosis of non-alcoholic fatty liver disease (NAFLD) with liver fibrosis. Method: A total of 72 patients with NAFLD admitted to our hospital from May 2018 to May 2019 were selected as the NAFLD group. During the same period, 35 healthy subjects were selected as the control group. According to the nonalcoholic fatty liver disease fibrosis score (NAFLDFS), the NAFLD group was divided into the NAFLD group without liver fibrosis (group A, NAFLDFS<-1.455, 45 cases) and NAFLD with liver fibrosis group (group B, NAFLDFS≥-1.455, 27 cases). The levels of serum LP, SLP, PCⅢ, collagen type Ⅳ, LN, HA, FBG of all groups were detected and compared. The HOMA-IR, NAFLDFS, BMI of all groups were calculated and compared. The value of the above serological indexes in the diagnosis of liver fibrosis in NAFLD patients was analyzed. Result: The levels of serum PCⅢ, collagen type Ⅳ, LN, HA, FBG, LP and the HOMA-IR, BMI of the NAFLD group were significantly higher than those of the control group, while the level of serum SLP was significantly lower than that of control group (P<0.05). The levels of serum PCⅢ, collagen type Ⅳ, LN, HA, FBG, LP of group B were significantly higher than those of group A, while the level of serum SLP was lower than that of group A (P<0.05), and there were no significant differences in HOMA-IR and BMI between the two groups (P>0.05). The AUC, sensitivity and specificity of LP, SLP in diagnosis of NAFLD with hepatic fibrosis were superior to PCⅢ, collagen type Ⅳ, LN, HA, FBG. Conclusion: Serum LP and SLP have good clinical value in the diagnosis of NAFLD with liver fibrosis.
[Key words] LP SLP Non-alcoholic fatty liver disease Liver fibrosis
First-authors address: Traditional Chinese Medicine Hospital of Songzi, Songzi 434200, China
doi:10.3969/j.issn.1674-4985.2021.13.015
近些年随着肥胖、糖尿病及代谢综合征在世界各国的广泛流行,非酒精性脂肪肝(non-alcoholic fatty liver disease,NAFLD)发病率及患病总人数明显升高,已成为导致慢性肝病发生的重要病因[1]。虽然多数NAFLD患者病情处于稳定状态,但流行病学调查显示仍有10%~20%患者可逐渐发展成为肝纤维化[2]。早期准确诊断NAFLD患者是否合并肝纤维化对于采取及时的治疗措施极为重要,但传统肝纤维化血清学指标检查结果易受某些因素影响而出现误差,故迫切需要寻找新的血清学检测指标[3]。有研究发现,瘦素(LP)及可溶性瘦素受体(SLP)在NAFLD发病过程中发挥着十分重要的作用[4]。故本研究拟观察血清LP及SLP在诊断NAFLD患者合并肝纤维化中的临床价值,现报道如下。
1 资料与方法
1.1 一般资料 选取2018年5月-2019年5月本院收治的72例NAFLD患者作为NAFLD组。同期选择35例本院门诊健康体检者作为对照组。纳入标准:NAFLD患者根据临床症状、肝脏超声影像学及实验室检查均符合相关诊断标准[5];所有患者及体检者年龄均大于18岁。排除标准:合并有病毒性肝炎、自身免疫性肝炎;合并有内分泌、遗传代谢疾病者;近期使用激素、护肝降酶、降血脂等药物治疗。根据非酒精性脂肪性肝纤维化评分(nonalcoholic fatty liver disease fibrosis score,NAFLDFS)将NAFLD组分为NAFLD无肝纤维化组(A组,NAFLDFS<-1.455,45例)与NAFLD伴肝纤维化组(B组,NAFLDFS≥-1.455,27例)。所有患者及体检者均知晓本项研究方案并签订知情同意书,且研究已通过医院伦理委员会批准同意。
1.2 方法 采用酶联免疫吸附试验检测各组血清LP、SLP表达水平;采用放射免疫法检测各组血清Ⅲ型前胶原(procollagen typeⅢ,PCⅢ)、Ⅳ型胶原、层黏蛋白(laminin,LN)、透明质酸(hyaluronicacid,HA)表达水平;采用全自动生化仪检测各组血清空腹血糖(fasting blood glucose,FBG)、同時计算各组胰岛素抵抗指数(homeostasismodel assessment insulin resistance,HOMA-IR)、NAFLDFS及体重指数(body mass index,BMI)等指标。HOMA-IR=FBG×空腹胰岛素/22.5,NAFLDFS=-1.675+0.037×年龄+0.094×BMI+1.13×空腹血糖调节受损或者糖尿病(是=1,不是=0)+0.99×AST/ALT-0.013×血小板-0.66×白蛋白。
1.3 统计学处理 采用SPSS 20.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组间比较采用独立样本t检验;计数资料以率(%)表示,比较采用字2检验;采用ROC法分析诊断价值。以P<0.05为差异有统计学意义。
2 结果
2.1 三组一般资料比较 A组男27例,女18例,平均年龄(41.2±10.8)岁;B组男16例,女11例,平均年龄(40.1±11.5)岁。对照组男21例,女14例,平均年龄(42.3±11.2)岁。三组一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
2.2 NAFLD组与对照组相关指标比较 NAFLD组血清PCⅢ、Ⅳ型胶原、LN、HA、FBG、LP水平及HOMA-IR、BMI均明显高于对照组,而血清SLP水平明显低于对照组(P<0.05),见表1。
2.3 A组与B组相关指标比较 B组血清PCⅢ、Ⅳ型胶原、LN、HA、FBG、LP水平均明显高于A组,而血清SLP水平明显低于A组,差异均有统计学意义(P<0.05);两组HOMA-IR、BMI比较,差异均无统计学意义(P>0.05)。见表2。
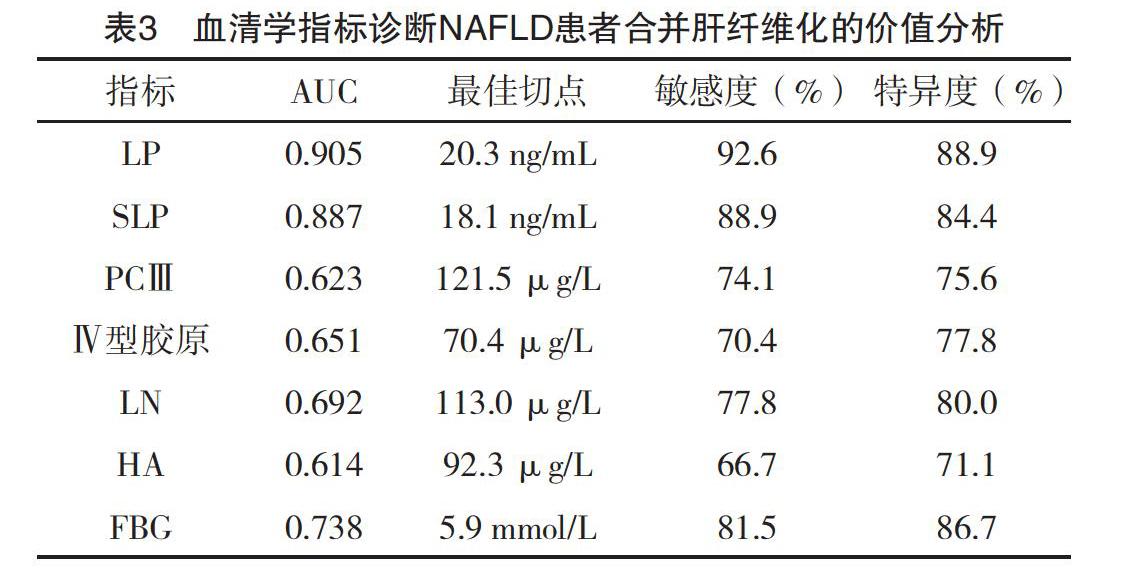
2.4 血清学指标诊断NAFLD患者合并肝纤维化的价值分析 LP、SLP诊断NAFLD患者合并肝纤维化的AUC、敏感度及特异度均优于PCⅢ、Ⅳ型胶原、LN、HA、FBG,见表3及图1。
3 讨论
NAFLD患者在逐渐进展成终末期肝衰竭的过程中常合并有肝纤维化现象,早期准确诊断肝纤维化并采取积极有效的治疗措施对有效阻断肝硬化及终末期肝衰竭的发生具有重要意义[6]。肝脏组织穿刺病理学检查因存在创伤性、医疗费用昂贵等缺点,难以在临床广泛开展。PCⅢ、Ⅳ型胶原、LN、HA等肝纤维化血清学指标虽然在脂肪肝诊断及肝纤维化分级方面具有较好的价值,但其检测结果易受到肝脏炎症反应的影响[7]。传统肝脏超声影像学检查则无法鉴别诊断NAFLD与早期肝纤维化表现[8]。故寻找无创性血清学指标诊断NAFLD患者合并肝纤维化仍是目前临床急需解决的问题。
LP是由机体内脂肪细胞合成及释放出来的脂肪细胞因子,其不但可调控食物摄取及能量消耗总量,还在生殖、血管形成、免疫系统防御反应等发挥着十分重要的功能作用[9-11]。此外,LP可有效促进胰岛素的合成及释放,从而加快肝脏组织及脂肪酸的氧化反应过程,同时还可明显刺激促炎症介质因子的合成及释放[12-15]。正常情况下人体肝脏组织检测不到瘦素的表达,而当肝星状细胞被激活活化和出现肝纤维化现象时,LP表达水平明显升高,提示LP在肝纤维化发生发展中占有重要的地位。目前较多研究认为,LP在激活活化的肝星状细胞呈特异性表达,进而作用于LP受体,通过多种信号转导途径而对肝脏生理功能及生理代谢过程产生影响[16-17]。SLP是LP受体在外周血循环系统中的可溶形式,其与LP呈1︰1结合且具有可逆性、剂量依赖性及特异性结合等多种特点。两者可形成双向闭合反馈调节环路,一方面LP合成和释放入血液循环系统后通过肝脏组织内的SLP发挥调节作用;另一方面LP又受到SLP的负性反馈调节[18]。SLP是决定外周血液循环系统中LP总量的关键因素,而SLP低水平表达是LP抵抗现象的重要标志。
NAFLDFS是一种评估肝脏纤维化严重程度的无创性评分系统,其有效性已得到较多研究的证实,也得到美国胃肠协会的推荐使用[19-20]。因此本研究采用NAFLDFS将NAFLD患者分為无纤维化组和纤维化组进行比较研究,结果显示NAFLD组血清LP表达水平明显高于对照组(P<0.05),血清SLP表达水平明显低于对照组(P<0.05);NAFLD伴肝纤维化组血清LP表达水平明显高于NAFLD无肝纤维化组(P<0.05),血清SLP表达水平明显低于NAFLD无肝纤维化组(P<0.05),提示血清LP和SLP可能成为诊断NAFLD患者是否合并肝纤维化的实验室指标。进一步采用ROC法分析LP、SLP及血清学指标诊断NAFLD患者合并肝纤维化的价值,结果显示血清LP、SLP诊断NAFLD患者合并肝纤维化的AUC、敏感度及特异度均优于PCⅢ、Ⅳ型胶原、LN、HA、FBG等血清学指标,提示血清LP、SLP诊断NAFLD患者合并肝纤维化的临床价值优于传统肝纤维化血清学指标。
综上所述,血清LP及SLP在诊断NAFLD患者合并肝纤维化方面具有较好的临床价值,值得临床广泛应用。
参考文献
[1] Haas J T,Francque S,Staels B.Pathophysiology and mechanisms of nonalcoholic fatty liver disease[J].Annual Review of Physiology,2016,78:181-205.
[2]万艳,常剑波,白艳霞,等.血清学指标在非酒精性脂肪性肝病诊断中的意义[J].临床肝胆病杂志,2017,33(5):963-968.
[3] Siddiqui M S,Charlton M.Liver Transplantation for alcoholic and nonalcoholic fatty liver disease:Pre-transplant selection and post-transplant management[J].Gastroenterology,2016,150(8):1849-1862.
[4] Cernea S,Roiban A L,Both E,et al.Serum leptin and leptin resistance correlations with NAFLD in patients with type 2 diabetes[J].Diabetes Metab Res Rev,2018,34(8):e3050.
[5]中华医学会肝病学分会脂肪肝和酒精性肝病学组.非酒精性脂肪性肝病诊疗指南(2018年更新版)[J].实用肝脏病杂志,2018,21(2):177-186.
[6] Yaghoubi M,Jafari S,Sajedi B,et al.Comparison of fenofibrate and pioglitazone effects on patients with nonalcoholic fatty liver disease[J].Eur J Gastroenterol Hepatol,2017,29(12):1385-1394.
[7]赵培,霍丽静,谭鹤,等.酒精性脂肪肝和非酒精性脂肪肝血液生化学指标的临床研究[J].中国卫生检验杂志,2017,26(23):3436-3438.
[8]贺鹏,任波,李玲,等.剪切波弹性成像技术在非酒精性脂肪性肝病诊断及肝纤维化分级中应用的初步研究[J].中国临床医学影像杂志,2017,28(9):637-641.
[9] Kucerova J,Babinska Z,Horska K,et al.The common pathophysiology underlying the metabolic syndrome,schizophrenia and depression.A Review[J].Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub,2015,159(2):208-214.
[10]魏新亮,史晓盟,苏振华.抗病毒治疗在丙型肝炎失代偿期肝硬化患者的临床应用及其对瘦素和脂连蛋白的影响[J].山西医药杂志,2017,46(17):2041-2044.
[11]赵智明,刘春丽,张群燕,等.针刺对糖尿病前期患者瘦素及可溶性瘦素受体的影响[J].针刺研究,2018,43(8):506-511.
[12] Widerska M,Jaroszewicz J,Stawicka A,et al.The interplay between Th17 and T-regulatory responses as well as adipokines in the progression of non-alcoholic fatty liver disease[J].Clin Exp Hepatol,2017,3(3):127-134.
[13] Parker R,Kim S J,Gao B.Alcohol,adipose tissue and liver disease:mechanistic links and clinical considerations[J].Nat Rev Gastroenterol Hepatol,2018,15(1):50-59.
[14] Behrouz V,Jazayeri S,Aryaeian N,et al.Effects of probiotic and prebiotic supplementation on leptin,adiponectin,and glycemic parameters in non-alcoholic fatty liver disease:a randomized clinical trial[J].Middle East J Dig Dis,2017,9(3):150-157.
[15] Mera K,Uto H,Mawatari S,et al.Serum levels of apoptosis inhibitor of macrophage are associated with hepatic fibrosis in patients with chronic hepatitis C[J].BMC Gastroenterol,2014,14(2):27-33.
[16] Meng Z,Zhang Y,Wei Z,et al.High serum resistin associates with intrahepatic inflammation and necrosis:an index of disease severity for patients with chronic HBV infection[J].BMC Gastroenterol,2017,17(1):6-12.
[17] Saad Y,Ahmed A,Saleh D A,et al.Adipokines and insulin resistance,predictors of response to therapy in Egyptian patients with chronic hepatitis C virus genotype 4[J].Eur J Gastroenterol Hepatol,2013,25(8):920-925.
[18]徐寶华.血清脂联素和瘦素与慢性乙型肝炎肝硬化分级的关系研究[J].河南医学研究,2018,27(11):1967-1969.
[19] Yang H R,Kim H R,Kim M J,et al.Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease[J].World J Gastroenterol,2012,18(13):1525-1530.
[20] Gisondi P,Barba E,Girolomoni G.Non-Alcoholic fatty liver disease fibrosis score in patients with psoriasis[J].J Eur Acad Dermatol Venereol,2016,30(3):282-287.
(收稿日期:2020-03-29) (本文编辑:田婧)