Identification of lymph node metastasis by computed tomography in early gastric cancer
Jingtao Wei ,Yinan Zhang ,Zhilong Wang ,Xiaojiang Wu ,Ji Zhang ,Zhaode Bu ,Jiafu Ji
1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing),Gastrointestinal Cancer Center,Peking University Cancer Hospital &Institute,Beijing 100142,China;2 Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing),Department of Radiology,Peking University Cancer Hospital &Institute,Beijing 100142,China
Abstract Objective:Lymph node status is critical when selecting treatment methods for patients with early gastric cancer(EGC).The aim of this study was to assess the diagnostic value of computed tomography (CT) for detection of lymph node metastasis (LNM) in patients with EGC.Methods:We retrospectively analyzed patients who had pathologically confirmed EGC between November 2010 and January 2019.After 1:1 propensity score matching,65 patients with LNM and 65 patients without LNM were retained for comparison.The long diameter (LD) and short diameter (SD) of all visualized lymph nodes in all stations were recorded.The diagnostic value of LNM was assessed with receiver operating characteristic analysis.Results:Among 130 patients,we found a total of 558 lymph nodes on the CT images.Among the diagnostic indicators,the number,sum of LD and sum of SD of lymph nodes greater than 3 mm had better discrimination.The areas under the curve were all greater than 0.75.As for different regions,the optimal cutoff values of number,the sum of LD and sum of SD were determined as follows:overall,≥4,19.9 mm and 13.5 mm;left gastric artery basin,≥3,15.7 mm and 8.6 mm;right gastroepiploic artery basin,≥2,8.6 mm and 7.0 mm.Conclusions:CT is valuable for diagnosing LNM in EGC patients.The number,sum of LD and sum of SD of lymph nodes greater than 3 mm are preferable indicators.Different regional lymph nodes have different optimal criteria for predicting LNM in ECG patients.
Keywords:Computed tomography;lymphatic metastasis;early gastric cancer;lymphatic basin
Introduction
Although gastric cancer incidence and mortality rates continue to decrease,gastric cancer remains the fourth most common cancer and the second leading cause of cancer-related deaths in China (1,2).Early gastric cancer(EGC) is defined as a lesion of the stomach confined to the mucosa and/or submucosa,regardless of its area or lymph node metastatic status (3).In recent years,the proportion of EGC has been increasing in East Asia (2,4).Some studies have reported that the proportion of ECG in China is approximately 20% (5).Regional lymph node metastasis(LNM) is one of the most significant prognostic factors in EGC,and preoperative determination of lymph node status is critical when selecting treatment methods.The LNM rate of ECG is reportedly 2%-20% (6).For EGC patients with a low possibility of LNM,endoscopic resection is approved as a curative treatment method,according to the guidelines for the diagnosis and treatment of gastric cancer in China and the Japanese Gastric Cancer Association treatment guidelines (7,8). In recent years,organpreserving gastrectomy and sentinel node navigation surgery have become a hot area of research in ECG,and sentinel LNM is the key factor (9).
In addition,the location of lymph nodes is also very important,and the characteristics of metastatic lymph nodes in different regions may be different.In 2003,Miwaet al.first proposed the concept of sentinel basin dissection(SBD).According to the direction of lymphatic drainage,the gastric lymphatic compartments were divided into five regions:left gastric artery basin,right gastric artery basin,left gastroepiploic artery basin,right gastroepiploic artery basin and posterior gastric artery basin (10,11).SBD is mainly applied in sentinel node navigation surgery for ECG (12).
However,the accuracy of detecting LNM with conventional diagnostic tools is only approximately 60%and is even lower in ECG (13).At present,the most commonly used diagnostic method for lymph node staging of gastric cancer patients is 64-slice or more multidetectorrow computed tomography (MDCT),which provides more useful information on the possibility of malignancy.Some studies have reported that the accuracy of MDCT for determining LNM ranges between 68% and 80% (14,15).Currently,the main MDCT criterion for characterizing a lymph node as malignant is size (16).However,there is no universal standard for the size criterion.Moreover,most of the related studies were based on advanced gastric cancer and there were few studies on ECG.Thus,this retrospective study was conducted to assess the diagnostic value of computed tomography (CT) for LNM in patients with EGC.
Materials and methods
Study population
We retrospectively analyzed patients with EGC who received radical gastrectomy at Peking University Cancer Hospital between November 2010 and January 2019.In total,out of 1,146 EGC patients undergoing radical gastrectomy,543 patients met the following criteria(Figure 1).We selected patients who were pathologically diagnosed with gastric adenocarcinoma after gastrectomy and standard D1+/D2 lymph node dissection with pathological stage T1,according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system.The exclusion criteria were as follows:1) patients with neoadjuvant therapy;2) two or more sites of primary gastric cancer;3) previous history of cancer or remnant gastric cancer; 4) distant metastasis; 5) incomplete preoperative examinations,including gastroscopy,endoscopic ultrasonography (EUS),abdominal enhanced CT and biopsy during gastroscopy;or 6) absence of abdominal enhanced CT images.
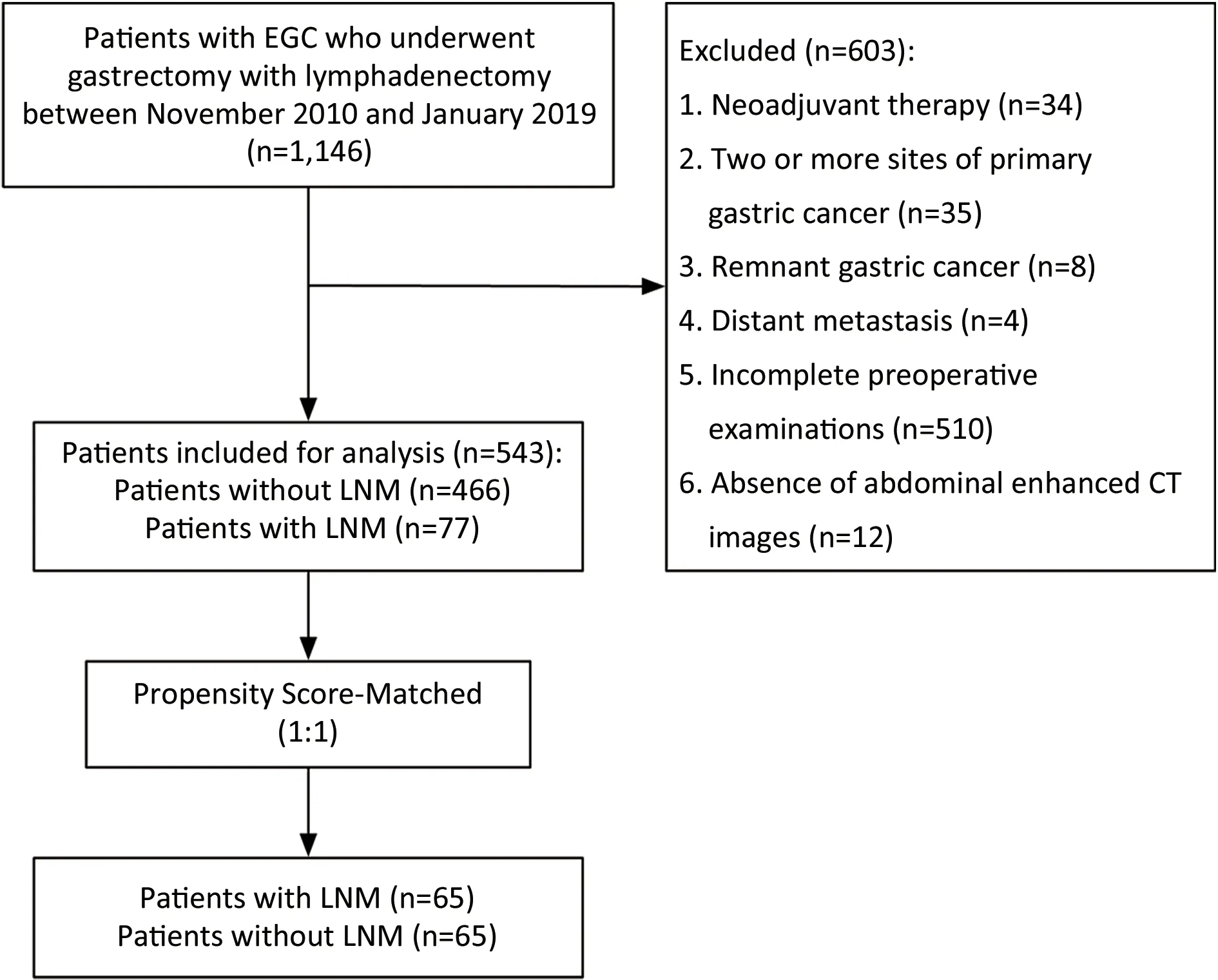
Figure 1 Flow chart of patient selection.EGC,early gastric cancer;LNM,lymph node metastasis.
Clinicopathological features of all patients were retrospectively collected.For pathological results,the differentiated type included papillary adenocarcinoma and well and moderately differentiated tubular adenocarcinoma,and the undifferentiated type included poorly differentiated adenocarcinoma and signet-ring cell carcinoma,and mucinous adenocarcinoma.Pathological reports recorded the stations and number of metastatic and non-metastatic lymph nodes.
This study was approved by the Medical Ethics Committee of the Peking University Cancer Hospital.Informed consent to be included in the study was obtained from all patients.
CT protocol
CT was performed using a CT scanner that had 64 rows of detectors (LightSpeed 64;GE Healthcare,Milwaukee,WI,USA).Patients fasted for at least 8 h prior to the examination.To increase gastric distention and reduce gastric motility,patients were given 8 g of oral gasproducing crystals and an intramuscular injection of 10 mg anisodamine (raceanisodamine hydrochloride,Hangzhou Minsheng Pharmaceutical CO.LTD,Hangzhou,China).Ten to 15 min later,an upper abdominal unenhanced CT scan from the diaphragmatic dome to 2 cm below the lower margin of the air-distended gastric body was acquired(collimation:0.625 mm,peak tube voltage:120 kVp,tube current-time product:automatic).Then,100 mL of nonionic contrast medium (Ultravist,300 mg/mL;Bayer,Germany) was given by intravenous injection using an 18-gauge angiographic catheter that was inserted into an antecubital vein at a rate of 3.5 mL/s using an automatic injector.Contrast-enhanced CT scans were performed in the arterial phase (30 s) and in the portal venous phase (70 s).
Analysis of CT images
All patients underwent abdominal enhanced CT examination before surgery.After the propensity score matching (PSM) process,CT images were read in 65 patients with LNM and 65 patients without LNM,for a total of 130 patients.CT images of each patient were independently reviewed by 2 oncological surgeons and 1 radiologist without knowing the status of lymph nodes.And 2 oncological surgeons well trained in the identification of perigastric lymph nodes.The station number (No.1,No.2,No.3,No.4sa,No.4sb,No.4d,No.5,No.6,No.7,No.8,No.9,No.11p,No.11d,No.12a),CT slice,long diameter (LD) and short diameter(SD) of each lymph node with a SD greater than 3 mm in the venous phase of enhanced CT were recorded.All measurements of the lymph nodes were performed on axial portal venous phase CT images with thickness of 0.625 mm.Lymph nodes of similar size observed by more than 2 physicians at the same station and at the same slice were taken as actually visible lymph nodes.The mean value measured by 2 or 3 physicians was used as the final value of the LD and SD of lymph nodes.
Statistical analysis
The statistical analyses were performed by using IBM SPSS Statistics (Version 26.0;IBM Corp.,New York,USA).The intraclass correlation coefficient (ICC) was used to assess interobserver agreement (17).ICC estimates and their 95%confident intervals (95% CIs) were calculated based on a mean-rating (k=3),absolute-agreement,two-way randomeffects model.For continuous variables,a test of normality was first performed.For normally distributed variables,differences between groups were analyzed usingt-test,and for nonnormally distributed variables,the Mann-Whitney U test was used.The Chi-squared test and Fisher’s exact test (when appropriate) were used for comparisons of categorical variables.Significant factors noted on univariate analysis were subsequently entered into a binary logistic regression model for multivariate analysis.Two-sided P<0.05 was considered statistically significant.
To accurately analyze the diagnostic value of CT,we used PSM to balance out the selection biases and confounding biases/factors between ECG patients with LNM and without LNM (non-LNM).For PSM,we chose variables as covariates that are known to potentially affect LNM in EGC based on the results of the univariate and multivariate analyses.After univariate and multivariate analyses,the presence of ulceration and tumor size on gastroscopy,postoperative histological type and pathological T stage were independent risk factors for LNM.Therefore,individual propensity scores were calculated by the logistic regression method based on the above 4 clinicopathological factors.A 1:1 ratio PSM study group was created with a 0.03 caliper width by the nearest neighbor method.
The area under the receiver operating characteristic(ROC) curve (AUC) was calculated to assess the diagnostic value of CT.The cutoff value of the diagnostic indicator was determined by the Youden index.In addition,the sensitivity,specificity,accuracy,positive predictive value(PPV) and negative predictive value (NPV) were also calculated.The Z test was applied to evaluate the diagnostic value by comparing the AUCs.
Results
Clinicopathological characteristics and PSM
From November 2010 to January 2019,543 patients were enrolled in our research,of which 77 (14.2%) patients had LNM,as detailed inTable 1.Among 543 gastric cancer patients with or without LNM,the two groups were consistent in terms of sex,age and tumor location.Significant differences regarding other clinicopathological factors were demonstrated between the two groups (Table 1).To reduce confounding bias,1:1 PSM was performed,65 EGC patients with LNM and 65 ECG patients withoutLNM were retained for comparison.No significant differences in previously associated covariates were noted between the two groups (Table 1).Among the 130 ECG patients,a total of 3,760 lymph nodes were resected at surgery,of which 167 were metastatic lymph nodes confirmed by pathology.Among 65 patients with LNM,there were 42 (64.6%) patients with stage N1,18 (27.7%)with stage N2 and 5 (7.7%) with stage N3a according to the 8th edition of AJCC staging system.
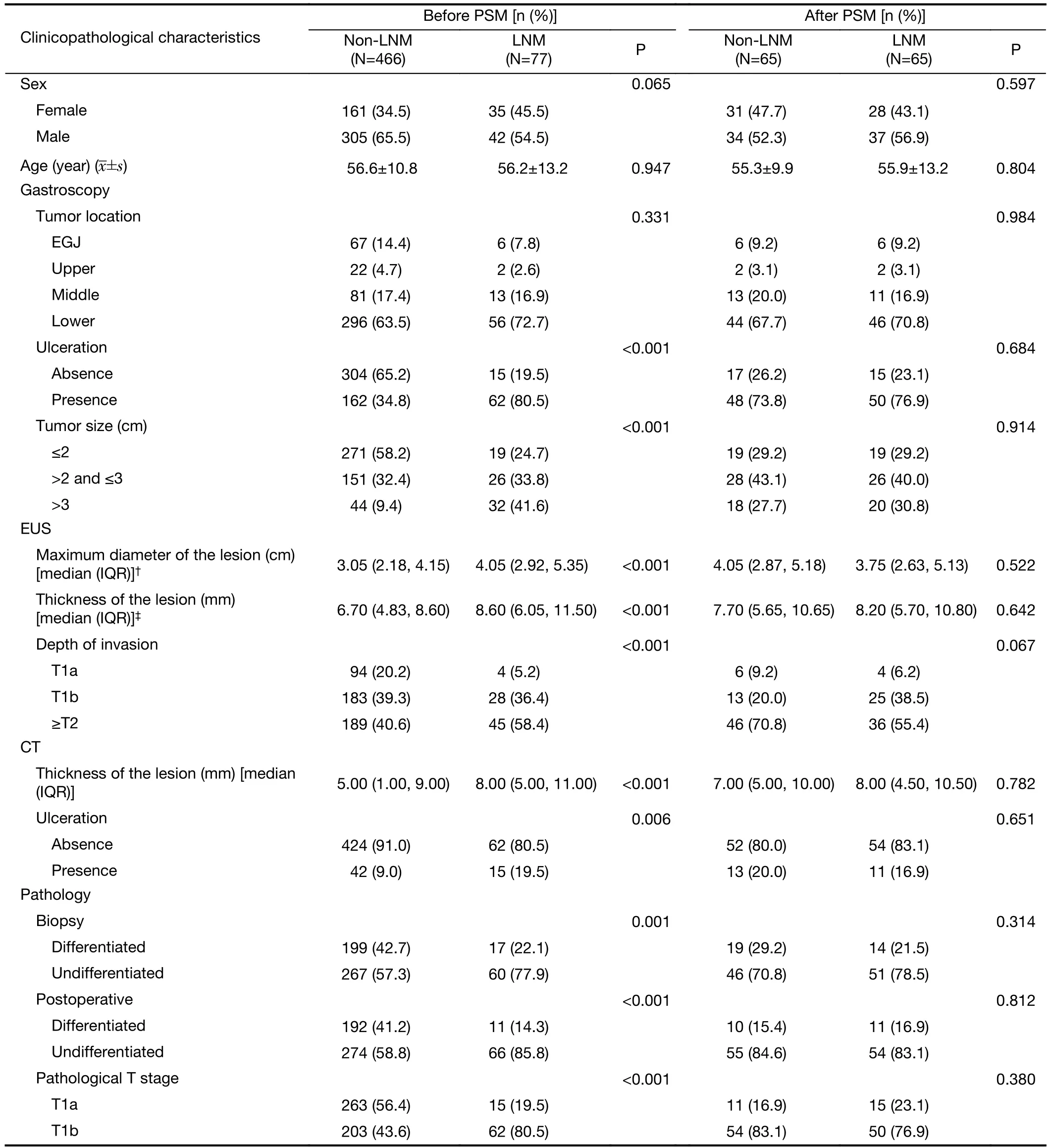
Table 1 Clinicopathological characteristics of EGC patients with LNM and non-LNM
Diagnostic value of CT images
Among 130 patients,we found a total of 558 lymph nodes greater than 3 mm on venous phase CT images (Table 2),and 371 (66.5%) of which were less than 5 mm.The 3 physicians showed a good level of agreement on the number,sum of LD and sum of SD of lymph nodes,with the intraclass correlation coefficient of 0.798 (95% CI,0.664-0.872),0.797 (0.623-0.879) and 0.814 (0.664-0.888),respectively. For 65 patients with LNM,a minimum of 1 lymph node and a maximum of 18 lymph nodes could be found.However,among the 65 patients without LNM,3 patients had no lymph nodes visible on CT,and 13 lymph nodes were found at most.Univariate analysis revealed that the number,sum of LD and sum of SD of lymph nodes,whose short diameter was greater than 3 mm or 5 mm,were related to LNM (Table 2).

Table 2 Analysis of LNs on CT images
Furthermore,to assess the value of these diagnostic indicators,ROC curves were graphed,demonstrating that the number,the sum of LD and the sum of SD of lymph nodes with SD greater than 3 mm were superior to those with SD greater than 5 mm (all P<0.05) (Figure 2).The AUCs of the ROC of the number,sum of LD and sum of SD of lymph nodes with SD greater than 3 mm were 0.787(95% CI,0.708-0.867),0.766 (95% CI,0.682-0.849) and 0.778 (95% CI,0.697-0.859),respectively.The results showed that the maximum Youden’s index of the number of lymph nodes with SD greater than 3 mm was 0.492,and the corresponding cutoff value was 3.5.Thus,the optimal threshold of the number of lymph nodes was ≥4.Meanwhile,the sensitivity,specificity,accuracy,PPV and NPV were 80.0% (95% CI,0.679-0.885),69.2% (95% CI,0.564-0.798),74.6% (95% CI,0.661-0.817),72.2% (95%CI,0.602-0.818) and 77.6% (95% CI,0.644-0.871),respectively.For the sum of LD and SD,the maximum Youden’s indexes were 0.462 and 0.507,respectively,and the corresponding cutoff values were 19.9 mm and 13.5 mm,respectively.The sensitivity,specificity,accuracy,PPV and NPV of the sum of LD were 90.8% (95% CI,0.803-0.962),55.4% (95% CI,0.426-0.675),73.1% (95%CI,0.645-0.803),67.0% (95% CI,0.561-0.765) and 85.7% (95% CI,0.708-0.941),respectively.The sensitivity,specificity,accuracy,PPV and NPV of the sum of SD were 89.2% (95% CI,0.785-0.952),61.5% (95%CI,0.486-0.731),75.4% (95% CI,0.669-0.823),69.9%(95% CI,0.587-0.792) and 85.1% (95% CI,0.711-0.933),respectively.

Figure 2 Assessment of diagnostic value of CT images.(A) ROC plot of the number of lymph nodes.The AUC of ROC of the number of lymph nodes with SD greater than 3 mm is better than those with SD greater than 5 mm [0.787 (95% CI,0.708-0.867) vs.0.650 (95% CI,0.554-0.745),P=0.001];(B) ROC plot of the sum of LD of lymph nodes.The AUC of ROC of the sum of LD of lymph nodes with SD greater than 3 mm is better than those with SD greater than 5 mm [0.766 (95% CI,0.682-0.849) vs. 0.634 (95% CI,0.538-0.730),P<0.001];(C) ROC plot of the sum of SD of lymph nodes.The AUC of ROC of the sum of SD of lymph nodes with SD greater than 3 mm is better than those with SD greater than 5 mm [0.778 (95% CI,0.697-0.859) vs.0.655 (95% CI,0.560-0.750),P=0.001].CT,computed tomography;ROC,receiver operating characteristic;AUC,area under the curve;95% CI,95% confidence interval;LD,long diameter;SD,short diameter.
Different regional lymph nodes
When considering the location of lymph nodes,surgical methods are one of the important factors,because some lymph node stations are not included in the D1+/D2 lymph node dissection area (7,18,19).Among 130 patients with gastric cancer,17 patients (13.1%) underwent total gastrectomy,103 (79.2%) patients underwent distal gastrectomy,and 10 (7.7%) patients underwent proximal gastrectomy. Therefore,we excluded lymph nodes according to the surgical methods to analyze lymph node stations within the range of D2 lymph node dissection area of distal or total gastrectomy and D1+lymph node dissection area of proximal gastrectomy (7,18,19).However,the results showed that the AUCs of the number,sum of LD and sum of SD of lymph nodes with SD greater than 3 mm were 0.784 (95% CI,0.704-0.864),0.760 (95%CI,0.676-0.845) and 0.776 (95% CI,0.695-0.857),respectively.There was no significant change in the diagnostic ability of the number,sum of LD or sum of SD of lymph nodes with SD greater than 3 mm (Z=0.682,P=0.495; Z=0.940,P=0.347; and Z=0.751,P=0.453,respectively).
In clinical practice,lymph nodes often appear near the common hepatic artery,and most of them are benign,which may affect the CT diagnosis of LNM.Therefore,No.8 lymph nodes were analyzed separately(Supplementary Table S1).Among the 130 EGC patients,63 No.8 lymph nodes were shown on CT images,and 7 patients had LNM at station No.8.The analysis found that the number,sum of LD and sum of SD of lymph nodes and ratio of LD to SD were not correlated with LNM.
The lymphatic basin is a good concept when analyzing the location of lymph nodes and is important for SBD.Therefore,in this study,among 65 patients with LNM,there were 37 (56.9%) cases of left gastric artery basin (No.1/No.3/No.7) metastasis,12 (18.5%) cases of right gastric artery basin (No.5/No.8) metastasis,1 (1.5%) case of left gastroepiploic artery basin (No.4sa/No.4sb) metastasis,27(41.5%) cases of right gastroepiploic artery basin (No.4d/No.6) metastasis,4 (6.2%) cases of posterior gastric artery basin (No.11) metastasis,and 5 (7.7%) cases of other lymphatic basin (No.2/No.9/No.12a) metastasis.Due to the small number of metastatic cases of the right gastric artery basin,left gastroepiploic artery basin,posterior gastric artery basin and other lymphatic basins,it is difficult to analyze the correlation between CT images and metastatic lymph nodes,so the left gastric artery basin and the right gastroepiploic artery basin were mainly analyzed.
The results revealed that the number,sum of LD and sum of SD of lymph nodes were related to LNM in both lymphatic basins (Table 3).Further study showed that the number,sum of LD and sum of SD of lymph nodes had good discrimination (Figure 3).In the left gastric artery basin,the AUCs of the ROCs of the number,sum of LD and sum of SD of lymph nodes were 0.803 (95% CI,0.726-0.879),0.799 (95% CI,0.721-0.876) and 0.809(95% CI,0.733-0.884),respectively.The cutoff values of the number,sum of LD and sum of SD were 2.5,15.7 mm and 8.6 mm,respectively.Thus,the optimal threshold of the number of lymph nodes was ≥3.Meanwhile,the sensitivity,specificity,accuracy,PPV and NPV of the number were 67.6% (95% CI,0.501-0.814),80.6% (95%CI,0.709-0.878),76.9% (95% CI,0.686-0.837),58.1%(95% CI,0.422-0.726) and 86.2% (95% CI,0.768-0.892),respectively.The sensitivity,specificity,accuracy,PPV and NPV of the sum of LD were 78.4% (95% CI,0.613-0.896),76.3% (95% CI,0.662-0.896),76.9% (95%CI,0.686-0.837),56.9% (95% CI,0.423-0.704) and89.9% (95% CI,0.805-0.952),respectively.The sensitivity,specificity,accuracy,PPV and NPV of the sum of SD were 86.5% (95% CI,0.704-0.949),67.7% (95%CI,0.571-0.769),73.1% (95% CI,0.645-0.803),51.6%(95% CI,0.387-0.643) and 92.6% (95% CI,0.830-0.973),respectively.

Table S1 Analysis of No.8 LNs on CT images

Table 3 Analysis of LNs within lymphatic basins

Figure 3 Assessment of diagnostic value of CT images in lymphatic basins.(A) Diagnostic value of CT images in left gastric artery basin.The AUCs of the number (black),sum of LD (red) and sum of SD (blue) of lymph nodes were 0.803 (95% CI,0.726-0.879),0.799 (95%CI,0.721-0.876) and 0.809 (95% CI,0.733-0.884),respectively;(B) Diagnostic value of CT images in right gastroepiploic artery basin.The AUCs of the number (black),sum of LD (red) and sum of SD (blue) of lymph nodes were 0.876 (95% CI,0.815-0.938),0.882 (95%CI,0.821-0.943) and 0.878 (95% CI,0.816-0.940),respectively.CT,computed tomography;AUC,area under the curve;95% CI,95%confidence interval;LD,long diameter;SD,short diameter.
In addition,in the right gastroepiploic artery basin,the AUCs of the number,sum of LD and sum of SD of lymph nodes were 0.876 (95% CI,0.815-0.938),0.882 (95% CI,0.821-0.943) and 0.878 (95% CI,0.816-0.940),respectively (Figure 3).The cutoff values of the number,sum of LD and sum of SD were 1.5,8.6 mm and 7.0 mm,respectively.Thus,the optimal threshold of the number of lymph nodes was ≥2.Meanwhile,the sensitivity,specificity,accuracy,PPV and NPV of the number were 85.2% (95%CI,0.654-0.951),77.7% (95% CI,0.682-0.850),79.2%(95% CI,0.711-0.856),50.0% (95% CI,0.351-0.649) and 95.2% (95% CI,0.876-0.985),respectively.The sensitivity,specificity,accuracy,PPV and NPV of the sum of LD were 88.9% (95% CI,0.697-0.971),77.7% (95%CI,0.682-0.850),80.0% (95% CI,0.719-0.863),51.1%(95% CI,0.363-0.657) and 96.4% (95% CI,0.891-0.991),respectively.The sensitivity,specificity,accuracy,PPV and NPV of the sum of SD were 85.2% (95% CI,0.654-0.951),78.6% (95% CI,0.692-0.859),80.0% (95%CI,0.719-0.863),51.1% (95% CI,0.360-0.661) and 95.3% (95% CI,0.877-0.985),respectively.
Discussion
Previous studies have shown that regional LNM is one of the most significant prognostic factors in EGC (20).Determining whether lymph nodes have metastasized is critical to the choice of treatment for ECG.MDCT is the cornerstone of gastric cancer staging,but the benefit of N staging for gastric cancer,especially ECG,remains unclear.To reduce selection bias,we used PSM to analyze the diagnostic value of CT more accurately.Several risk factors for LNM in EGC,such as tumor size,invasion depth,presence of ulceration,histological type,and lymphovascular invasion,have been reported in previous studies(6,21),which were consistent with this study and balanced between the two groups.
In this study,the total lymph node detection rate and the proportion of small lymph nodes less than 5 mm were 14.8% (558/3,760) and 66.5% (371/558),respectively.The total detection rate was lower than that of the related studies,while the proportion of small lymph node examinations was higher (22).The reason may be that relevant studies included not only patients with ECG but also patients with advanced gastric cancer,while this study only included patients with ECG.The study by Parket al.also showed that benign regional lymph nodes were more frequently detected in advanced gastric cancer than in early gastric cancer (23).The lymph nodes of patients with ECG are smaller,which is difficult to find on CT images,but CT image analysis is still valuable for the determination of LNM in EGC.
Currently,there are no generally accepted CT criteria for characterizing a lymph node as malignant,including size,round shape,central necrosis,enhancement,and clustering of 3 or more lymph nodes (16).Most investigations have found that specificity for CT ranges widely from 62.5% to 91.9%,while sensitivity varies between 50% and 89.9% across various studies (24).In addition,most studies use size as a diagnostic criterion,and a threshold of 8 mm is often used (24).A study by Kubotaet al.showed that when choosing a smaller threshold (1-12 mm),the sensitivity was higher and the specificity was lower (25).The accuracy of the size criterion varies greatly from study to study because LNM will not necessarily result in lymph node enlargement.A relevant study has shown that most metastatic lymph nodes are less than 10 mm,and only a small proportion of patients with LNM exhibit the largest metastatic lymph node (26).Alternatively,lymph nodes might be enlarged due to causes other than metastasis,such as inflammatory reactions to primary tumors.Different from advanced gastric cancer,in this study,3 mm was finally determined as the optimal threshold value due to its high degree of discrimination.At the same time,the measurement of lymph nodes on axial portal venous phase CT images with 0.625 mm thickness could ensure high consistency.
The diagnostic accuracy of traditional CT for cN staging was not satisfactory,so researchers have attempted to develop other methods with high sensitivity and specificity.Some studies suggested that MDCT combined with serum tumor biomarkers could improve preoperative sensitivity and accuracy of LNM (27).Liet al.found that dual-energy CT showed acceptable accuracy in predicting LNM of gastric cancer (28).In addition,researchers have also applied radiomic analysis and deep learning to predict the LNM of gastric cancer,which presented good predictive value for LNM (29,30).However,its practicability,accessibility and application in ECG still need further study.For advanced gastric cancer,some researchers found that the sum of the diameters of metastatic lymph nodes may be sufficiently useful in assessing N stage,which was superior to the conventional CT stage (31).However,there are few studies on ECG.This study showed that CT image analysis was still of great value in predicting LNM in EGC.
Takuro’s study found that diagnostic accuracy was improved by using individual cutoff values for each lymph node region,indicating that the characteristics of metastatic lymph nodes in different perigastric regions were different (13).Meanwhile,it is difficult to determine whether the enlarged lymph nodes seen on the CT images are pathologically confirmed metastatic lymph nodes,and during the grouping of lymph nodes,metastatic lymph nodes may be classified into adjacent stations due to mistakes or unclear anatomic landmarks of the isolated specimens.Therefore,in this study,we introduced the concept of the lymphatic basin to analyze the features of metastatic lymph nodes in different regions.The results showed that the criteria for predicting LNM were different in different lymphatic basins.Sentinel basin metastasis is also important for sentinel node navigation surgery,this study can promote the application of CT in this area.
Our study provides effective CT diagnostic criteria for LNM in ECG patients,especially for true lymph nodenegative patients because of its high NPV.Combining our criteria with other criteria,such as endoscopy and pathology,may further improve the diagnostic accuracy of LNM in ECG patients.Due to the use of PSM,there is a bias of LNM rate between the enrolled population and the general population,so the instructional clinical value of PPV and NPV in this study is fairly modest.However,this study still provides a basis for the selection of personalized treatment for patients with ECG and will also create conditions for sentinel lymph node study and functional preservation surgery for ECG.
It is undeniable that this study also has many limitations.One of the limitations of our study was the small number of patients.Moreover,some lymphatic basins have a low rate of metastasis and are thus difficult to analyze.Furthermore,it was a retrospective study.Therefore,a larger-scale study is required to verify the clinical usefulness of our findings in ECG.In addition,LNM was not evaluated for each lymph node individually because it is impossible to match the lymph nodes dissected during surgery with those evaluated on CT.Finally,this study lacks external validation.More efforts should be made before clinical application.
Conclusions
CT is valuable for diagnosing LNM in ECG.The number,sum of LDs and sum of SDs of LNs greater than 3 mm are preferable indicators.Different lymphatic basins have different optimal criteria for predicting LNM in patients with EGC.
Acknowledgements
This study was supported by Beijing Hospitals Authority Clinical Medicine Development of special funding (No.XMLX202119) and Digestive Medical Coordinated Development Center of Beijing Municipal Administration of Hospitals (No.XXT20).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2021年6期
Chinese Journal of Cancer Research2021年6期
- Chinese Journal of Cancer Research的其它文章
- Prudent application of single-cell RNA sequencing in understanding cellular features and functional phenotypes in cancer studies
- ZNF292 suppresses proliferation of ESCC cells through ZNF292/SKP2/P27 signaling axis
- Development and validation of a questionnaire-based risk scoring system to identify individuals at high risk for gastric cancer inChinese populations
- Associations of centralization with health care quality for gastric cancer patients receiving gastrectomy in China
- Deep learning model improves radiologists’ performance in detection and classification of breast lesions
- All-trans retinoic acid (ATRA) inhibits insufficient radiofrequency ablation (IRFA)-induced enrichment of tumor-initiating cells in hepatocellular carcinoma
