Practice and knowledge of the dangers of self-medication among pregnant mothers attending antenatal care in Iganga District(Uganda)
Sarah Namususwa,Rebecca Nakaziba
1Department of Pharmacology and Therapeutics,Faculty of Medicine,Lira University,Lira P.O Box 1035,Uganda. 2Department of Nursing and Midwifery,Faculty of Health Sciences,Lira University,Lira P.O Box 1035,Uganda.
Abstract Background: Self‐medication is a common practice among pregnant mothers in many developing countries Uganda inclusive. Despite its adverse effects to the pregnant mother and the developing fetus, limited efforts are in place to reduce the practice. This study was conducted to assess the practices and knowledge of the dangers of self‐medication among pregnant mothers attending antenatal care in Iganga district, Uganda. Methods: A cross sectional approach was employed using convenient sampling technique among 181 pregnant mothers at the antenatal clinic. An interviewer administered questionnaire was used to collect data that was analyzed descriptively using SPSS software.Results:Out of the 181 respondents, 119 (65.75%) self‐medicated during their current pregnancy obtaining drugs from pharmacies 42 (23.20%). Majority of the mothers 129 (71.27%) had good knowledge concerning the dangers of self‐medication with 66.85% reporting that it was a bad practice. Regarding the dangers of self‐medication, 23.76% reported fetal death while 24.86% stated miscarriages. There was a significant association between self‐medication practice and occupation (P‐value = 0.04; OR = 1.21 at 95% CI). Conclusion:Self‐medication remains a common practice among pregnant mothers in Iganga district despite the fact that a large proportion of them have good knowledge regarding the dangers of self‐medication. Therefore, further investigations into the associated factors and strict measures to combat the risks of self‐medication during pregnancy should be embarked on.
Keywords:self‐medication; dangers; pregnant mothers;Iganga
Introduction
Self‐medication denotes the use of drugs for self‐diagnosed ailments or continual use of previously prescribed drugs for chronic or recurrent sicknesses without consulting a doctor [4, 5]. Self‐medication practices comprise obtaining drugs minus prescription from a health personnel; resubmitting an old prescription to acquire drugs; sharing medicines between relatives and friends; as well as failing to comply with a prescription [6]. Self‐medication among pregnant mothers is a widespread challenge that requires attention due its potential threat to the mother and the unborn child [7]. Studies have shown that drug exposure during pregnancy especially in the first trimester can lead to adverse effects to the fetus such as congenital abnormalities like heart and brain defects; low birth weight, premature birth and intrauterine growth retardation [8]. An estimated 94% of women use at least one medication while pregnant with almost 70% in the first trimester of pregnancy during which organogenesis occurs [9]. Studies conducted in Indonesia, Jordan and Brazil revealed that self‐medication among pregnant mothers was at 11.7%, 33% and 36% respectively [10‐12].In Nigeria and Ghana,self‐medication in pregnancy stands at 60%and 88% correspondingly with prescriptions only, over the counter medicines and herbal remedies [ 7, 13, 14]. In Ethiopia,self‐medication among pregnant mothers was at 55.2% in 2013 and 40.8% in 2021 mainly with antibiotics and analgesics [15, 16] while in Brazzaville (Congo), it is estimated at 14%especially for headaches[17]. In a survey conducted in Tanzania, 46.24% of pregnant mothers self‐medicated [18] while in one study conducted in Uganda (Zombo district), self‐medication in pregnancy was at 70.65% with antimalarials and NSAIDs [19]. The common sources of drugs include markets and pharmacies [17] whereas the leading illnesses associated with self‐medication are malaria, morning sickness and headaches[18, 20]. Among pregnant mothers, the awareness of the effects of self‐medication to both the mother and the fetus is generally low[21].In a study conducted in Iran, a total of 52.2% of pregnant mothers reported that their knowledge about self‐medication adverse effects was either low [22]. Studies in American, Asian and European countries revealed misconceptions regarding pregnant mothers’knowledge of the drugs especially antibiotics [23, 24]. In one of the studies, 96% of the pregnant mothers reported incorrect concepts of self‐medicated disease causes including drugs’ administration [25]. In Ethiopia a study conducted in 2015 revealed that 80%of the pregnant mothers perceived the risk of self‐medication associated congenital defects as low [26]. However in 2020, 70% of the mothers perceived drugs as harmful during pregnancy [27]. Despite the wide spread and adverse impact of self‐medication during pregnancy, there remains very few programs for its control[21].
In Uganda, studies related to self‐medication especially among pregnant mothers are scarce. This research therefore was intended to assess the self‐medication practices and the level of awareness regarding the dangers of self‐medication among pregnant mothers attending antenatal clinic in Iganga district.
Methods
Ethical approval
Ethical approval was obtained from the research and ethics committee of Lira University (LUREC‐18‐025) as well as from management of IGH. The study purpose was also clearly explained to the participants who signed a consent form before being recruited into the study. In addition, the study participants were individually interviewed to ensure privacy while their identity was concealed.
Study design and approach
This was quantitative cross sectional study using interviewer administered questionnaire.
Study site and setting
The study was conducted in the antenatal clinic of Iganga General Hospital(IGH).The Antenatal clinic(ANC)which is part of Outpatient Department (OPD) has an average monthly attendance of 1,950 pregnant mothers. The hospital is located in Nakavule, Lubaale zone,central division, Iganga municipality, Iganga district, and 400 m from Iganga town. It is the district general hospital and a referral point for health centers within the district. The hospital also serves other neighboring districts like Mayuge, Luuka and Namutumba.
Study population
Pregnant mothers attending ANC at IGH, Iganga district.
Sampling technique
Convenience sampling technique was used for the study giving every pregnant mother an equal opportunity of being selected, thus bias was avoided and fairness effected [28,29].
Sample size
An adjusted sample size of 181 was determined using a formula by Methodology[28, 30].
Eligibility
The study included all pregnant mothers attending ANC at IGH who were willing to participate in the study by signing a consent form before data collection. Mothers who were mentally unstable or had any pregnancy related complication were excluded.
Data collection method, instruments and procedure
Data was collected using a pretested interviewer administered questionnaire. Participants were interviewed individually or in the presence of their husbands in the triage shade of ANC clinic during their waiting time. Interviewer administered questionnaires were preferred because they gather responses in a standardized way while ensuring confidentiality [31].
Statistical analysis
The quantitative data‐sets were analyzed using Statistical Package for Social Sciences (SPSS) statistical analysis software (IBM SPSS, version 23). Descriptive statistics such as frequencies and percentages were used for this study and data was presented in tables, graphs and figures. The main variables of interest were practices and knowledge regarding dangers of self‐medication among pregnant mothers attending ANC at Iganga general hospital. A pregnant mother who admitted exposure to one form of self‐medication was regarded as having self‐medicated. Participants’ knowledge regarding dangers of self‐medication was measured using a questionnaire and compiled in percentages. A pregnant mother with 80% and above was considered having a high level of knowledge, whereas 50‐79% was regarded as moderate knowledge level while below 50% had low knowledge.
Results
Respondents and their characteristics
Demographic characteristics The study examined 181 pregnant mothers attending ANC at IGH. Most of the respondents (47.51%)were in the age group of 21‐28 and interestingly, 27.07% were teenage mothers. 34.81% had primary level of education with the number of participants decreasing as the education level advanced.Many (50.28%) participants lived in the rural setting with majority(61.33%) being unemployed. Among those who were employed(38.67%), 18.23% were earning less than 100,000. A substantial number of participants (40.33%) walked to the health facility with 66.85% travelling a distance of less than 5 km to the health facility(Table 1).
Gynecological and Obstetrical characteristics Majority(52.49%)of the respondents were multi‐gravida, with 72.37% of the mothers having a parity of less than 3. 77.90% of the respondents reported no history of abortions. However, 7.73% reported 2 or more abortions(Table 2).

Table 1 Showing the demographic characteristics
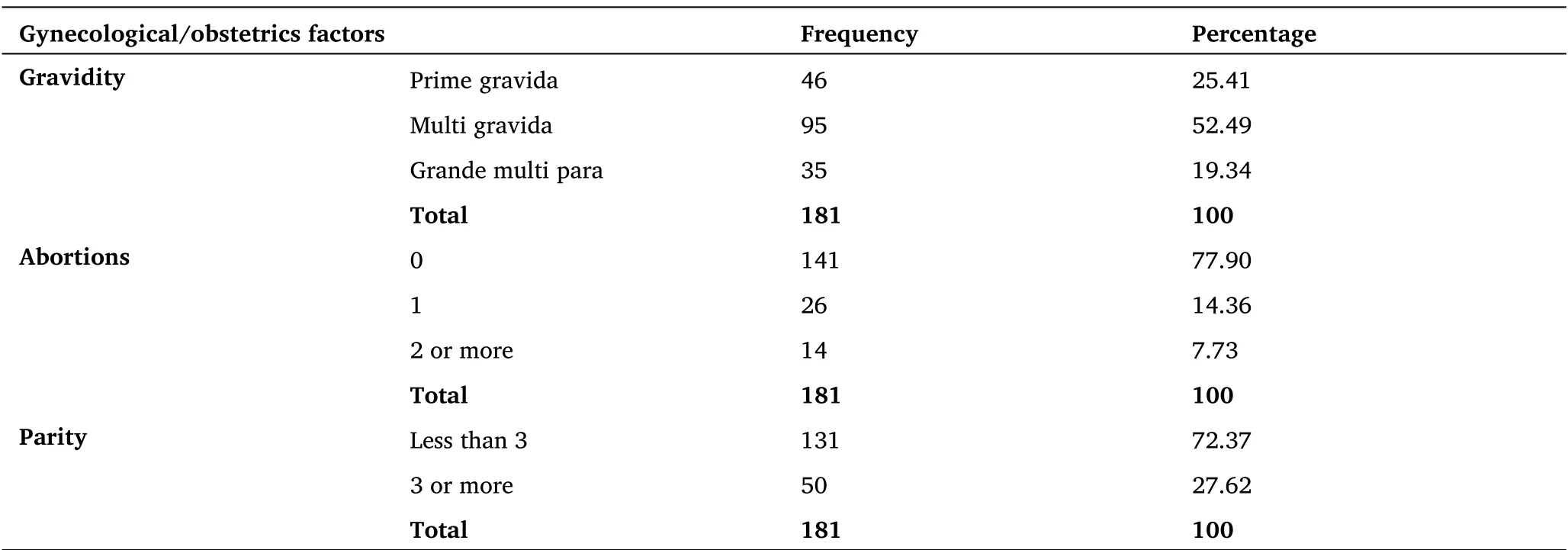
Table 2 Showing the gynecological and obstetrics characteristics
Self medication
Prevalence of self-medication Out of the 181 respondents, 65.75%self‐medicated during their current pregnancy while 34.25% did not self‐medicate (Figure 1).
Practices of self-medication 55 (30.39%) mothers who self‐medicated acquired drugs for self‐medication using the old prescription while only 10 (5.52%) used information from adverts(Table 3).
Sources of drugs for self-medication. 23.20% of the respondents who self‐medicated acquired drugs from Pharmacies while only 5.52%from friends (Table 4).
Health seeking practices
39.78% seek medical advice from professional medical personnel for any sign and symptoms(Figure 2).
Knowledge level regarding dangers of self-medication.
Majority (66.85%) of the respondents reported that it was not a good practice to self‐ medicate (Figure 3).
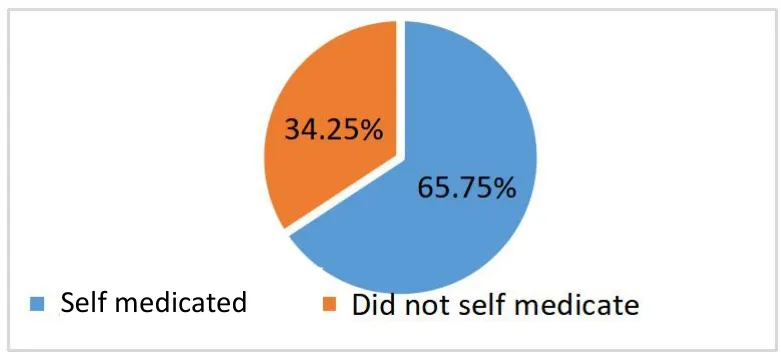
Figure 1 Showing prevalence of self-medication (n = 181)
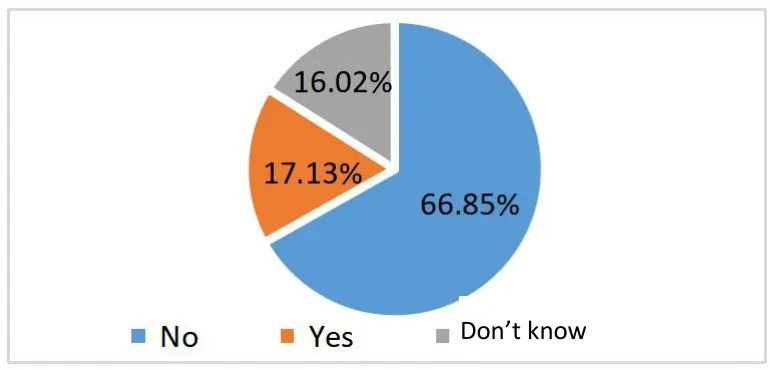
Figure 3 Showing the perception of pregnant mothers’knowledge regarding self-medication

Table 3 Showing some of the practices of self-medication

Table 4 Showing the sources of drugs for self-medication
Knowledge level of mothers regarding use of self-medicated drugs
Majority (71.27%) of the respondents had good knowledge on use of self‐medicated drugs(Table 5)
Dangers of self-medication to the unborn child and the pregnant mother 23.76%mothers reported death of the baby while 24.86% stated miscarriages (Table 6).
Bivariate analysis
Association between the demographic factors and the practice of self-medication There was a significant association between self‐medication practice and occupation (P‐value = 0.04). Age,education level, residence, transport means, salary scale and health facility distance were not significant (Table 7).

Table 5 Showing the knowledge level of mothers regarding use of self-medicated drugs

Table 6 Showing the dangers of self-medication to the unborn child and the pregnant mother
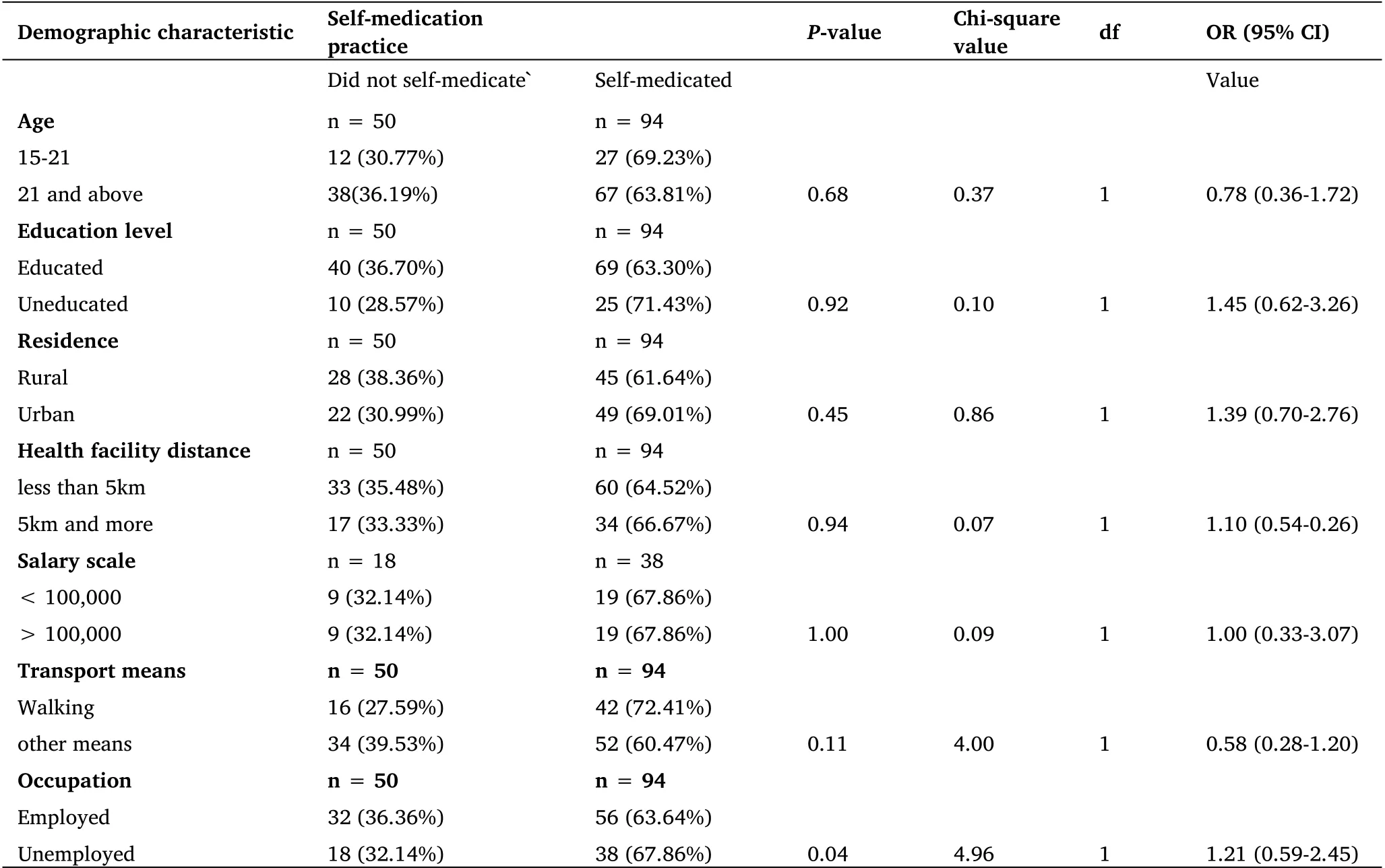
Table 7 Showing the association between the demographic factors and the practice of self-medication
Association of Gynecological and obstetrics factors with self-medication practice There was no statistical significance between the gynecological/obstetrics factors with practice of self‐medication. AllP‐values above 0.05 (Table 8).
Association of demographic factors with knowledge level There was no statistically significant association between knowledge level and the demographic factors. AllP‐values above 0.05 (Table 9).
Associationbetweenknowledgeleveland gynecological/obstetric factors There was a statistically significant association between knowledge level and the number of miscarriages(P‐value=0.04). However, gravidity and parity were not significant[P‐value = 0.16 and 0.50 respectively] (Table 10)
Association between the knowledge level and the practice of self-medication There was no significant association between the knowledge level and the practice of self‐medication (Table 11).

Table 8 Showing the association of gynecological/obstetrics factors with the practice of self-medication
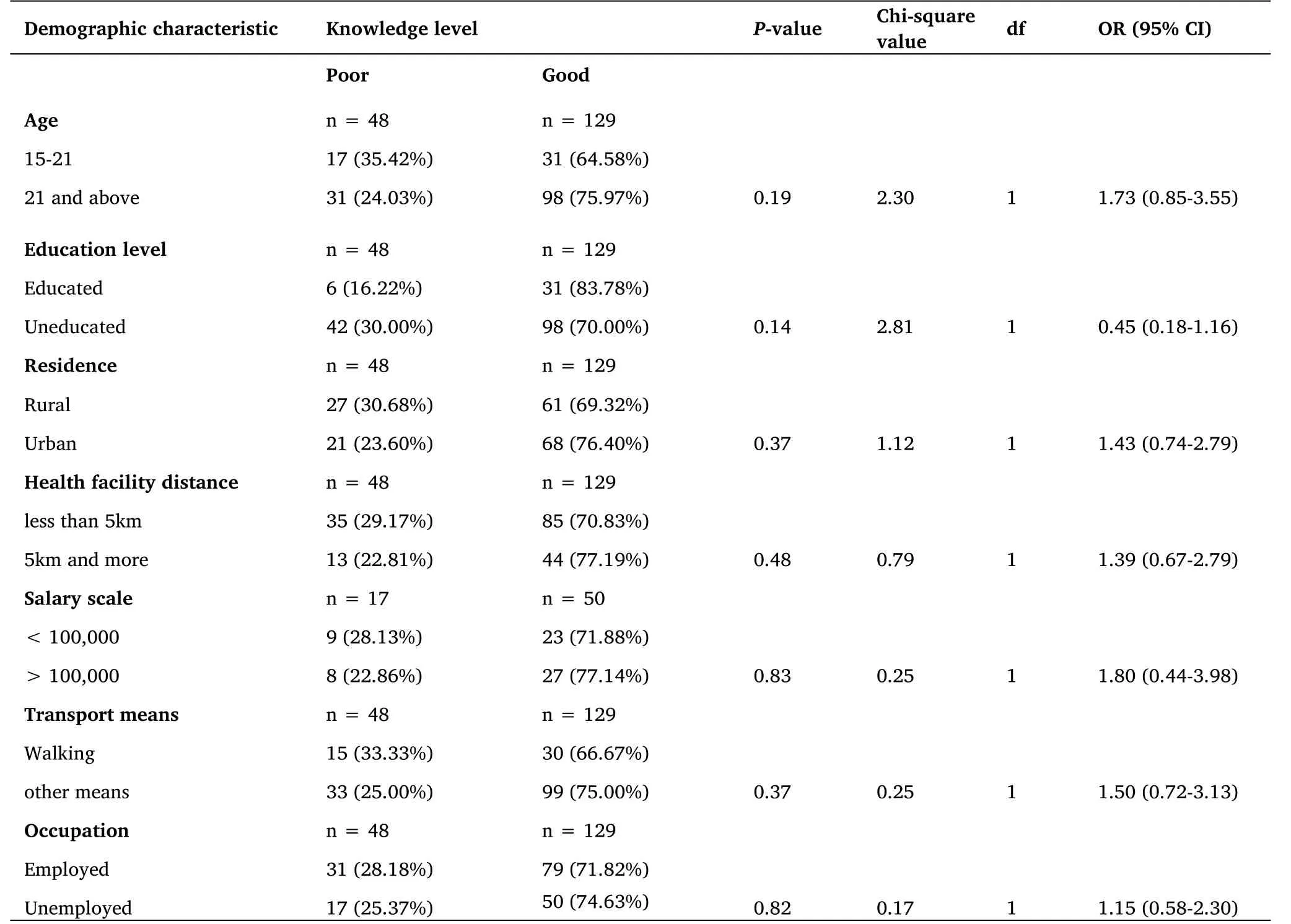
Table 9 Showing the association between demographic factors and knowledge level
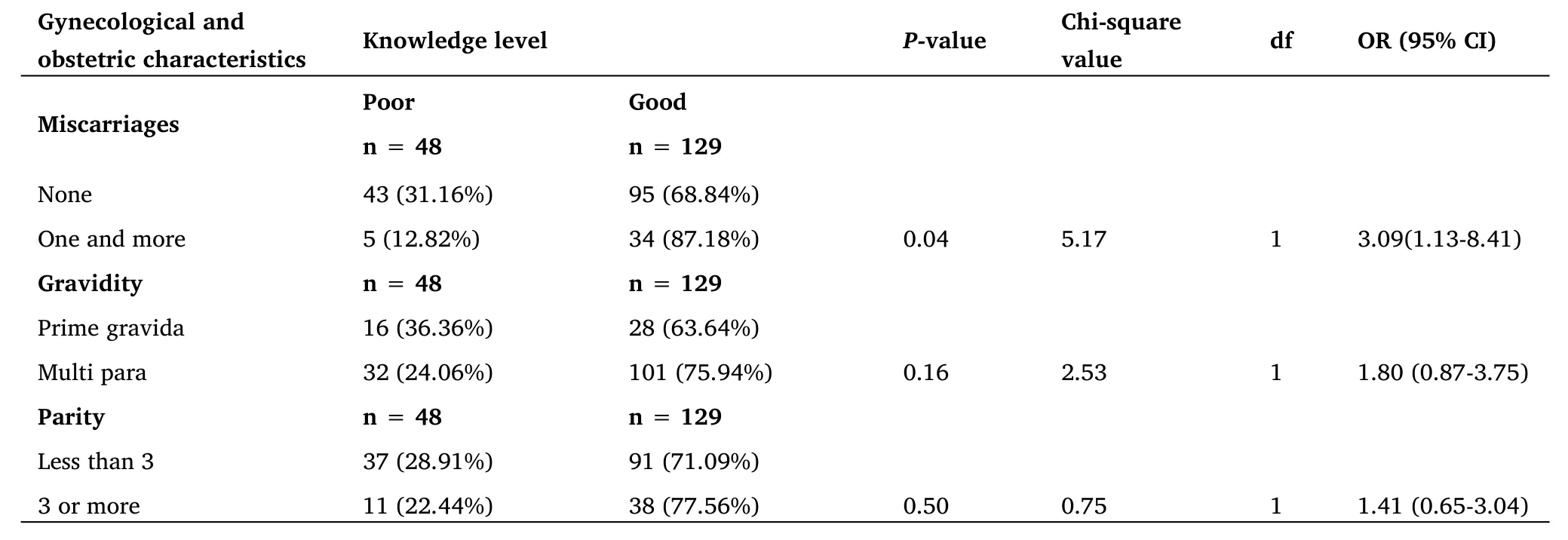
Table 10 Showing the association between gynecological/obstetric factors and the knowledge level

Table 11 Showing the relationship between the knowledge level of mothers and the practice of self-medication
Discussion
65.75%of the participants in the present study self‐medicated (Figure 1). However, in a study conducted in Zombo district in West Nile(Uganda), a slightly higher prevalence of 70.65%of pregnant mothers practiced self‐medication [19]. The findings of this study support the results of a study conducted in Nigeria where 62.9% of the pregnant mothers attending ANC practiced self‐medication [7].On the contrary a study conducted in Brazzaville, Congo showed that only 14% of pregnant mothers self‐medicated [17]. Pregnant mothers practice self‐medication due to higher costs of treatment at health facilities and inconveniences such as long queues. In addition, the present study showed that most mothers get the drugs from pharmacies and drug shops (Table 4). This is because most pharmacies and drug shops in the country do not require prescriptions from doctors to issue medicines to people in the community. The respondents also revealed that it is cheaper to obtain drugs from those preferred drug sources compared to health facilities or hospitals. Other reasons registered included long waiting time for medicines at health facilities and drug stock‐outs in government health facilities. These findings are slightly similar to a study conducted in Mukono,Uganda regarding practice of self‐medication which indicated that 81%of the mothers got drugs for self‐medication from drug shops and related studies in Ethiopia [32,33]. Majority (30.39%) of the pregnant mothers in the present study who practiced self‐medication used old prescriptions to acquire drugs(Table 3). This could be due to reappearance of signs and symptoms that are similar to previous conditions that mothers face. The current findings are consistent with the results from a study conducted in Lango sub‐region, Northern Uganda where majority of the study participants obtained drugs from pharmacies and drug shops [34].Comparable to the current findings, in Nigeria, 72.4% of pregnant mothers were involved in one form of self‐medication [21]. The current results further show that respondents practiced self‐medication due to seriousness of the sickness (Figure 2). In the study area, 34.25% of the respondents seek medical advice from trained medical personnel only when they are severely ill (Figure 2).From the bivariate analysis,self‐medication was more common among higher socio‐economic status pregnant mothers than those with a lower socioeconomic status. The fear of losing earnings and a moderate knowledge level in drug use could account for the higher prevalence of self‐medication among the socio‐economically empowered mothers. This finding is in congruent with the findings in India and Brazil [35, 36]. In the present study, 71.27% of the participants had good knowledge regarding the dangers of self‐medication while 66.85%of the participants noted that it was not a good practice for a pregnant mother to acquire drugs without a prescription from professional medical personnel (Figure 3). Similar studies in Africa revealed that 87.6% of respondents had adequate knowledge about the safety of drugs yet the rates of self‐medication were still high at 69.9%[13].In another related study,the knowledge of pregnant mothers regarding self‐medication was moderate with approximately 50% of the pregnant mothers believing that medications were harmless and preferred to continue [37]. In this study, 18.23% of the pregnant mothers reported intrauterine growth retardation (poor growth of baby), 14.36% low birth weight (small baby), 12.71% preterm birth and 9.94% congenital malformations(missing body parts) while 24.86% reported miscarriages comparable to findings in Nigeria [21]. There was a significant association between occupation and self‐medication among the mothers in the present study (Table 7) probably to save time for working.
Conclusion
The practice of self‐medication among pregnant mothers attending antenatal clinic in Iganga district is quite high yet a good proportion of mothers have adequate knowledge regarding the dangers of self‐medication. However, there are still some shortcomings in this study. The study was conducted at only one health facility and may not apply to other health facilities in the district unless related studies are conducted across the district. Adequate counseling of pregnant mothers by healthcare professionals about the potential risks of self‐medication with non‐prescription medicines during pregnancy is strongly warranted.
 Nursing Communications2022年13期
Nursing Communications2022年13期
- Nursing Communications的其它文章
- Delphi and Analytic hierarchy process for the construction of a risk assessment index system for post-stroke shoulder-hand syndrome
- A review of obstacles and facilitating factors of implementing Clinical Ladder Programs in nursing
- Spiritual health, empathy ability and their relationships with spiritual care perceptions among nursing students in China:A cross-sectional correlational study
- Qualitative study on influencing factors of refusal of gastric tube placement in stroke patients with dysphagia
- The influence of professional identity and ageism on turnover intention in nursing homes: a cross-sectional study from suzhou, China
- The relationship of family separation and nutrition status among under-five children: a cross-sectional study in Panti Public Health Center, Jember Regency of East Java, Indonesia
