Oral higher dose prednisolone to prevent stenosis after endoscopic submucosal dissection for early esophageal cancer
Sheng-Gang Zhan, Ben-Hua Wu, De-Feng Li, Jun Yao, Zheng-Lei Xu, Ding-Guo Zhang, Rui-Yue Shi, Yan-Hui Tian, Li-Sheng Wang
Sheng-Gang Zhan, Ben-Hua Wu, De-Feng Li, Jun Yao, Zheng-Lei Xu, Ding-Guo Zhang, Rui-Yue Shi, Yan-Hui Tian, Li-Sheng Wang, Department of Gastroenterology, Second Clinical Medical College of Jinan University, Shenzhen People’s Hospital, Shenzhen 518020, Guangdong Province, China
Abstract BACKGROUND Esophageal stenosis is one of the main complications of endoscopic submucosal dissection (ESD) for the treatment of large-area superficial esophageal squamous cell carcinoma and precancerous lesions (≥ 3/4 of the lumen). Oral prednisone is useful to prevent esophageal stenosis, but the curative effect remains controversial.AIM To share our experience of the precautions against esophageal stenosis after ESD to remove large superficial esophageal lesions.METHODS Between June 2019 and March 2022, we enrolled patients with large superficial esophageal squamous cell carcinoma and high-grade intraepithelial neoplasia experienced who underwent ESD. Prednisone (50 mg/d) was administered orally on the second morning after ESD for 1 mo, and tapered gradually (5 mg/wk) for 13 wk.RESULTS In total, 14 patients met the inclusion criteria. All patients received ESD without operation-related bleeding or perforation. There were 11 patients with ≥ 3/4 and < 7/8 of lumen mucosal defects and 1 patient with ≥ 7/8 of lumen mucosal defect and 2 patients with the entire circumferential mucosal defects due to ESD. The longitudinal extension of the esophageal mucosal defect was < 50 mm in 3 patients and ≥ 50 mm in 11 patients. The esophageal stenosis rate after ESD was 0% (0/14). One patient developed esophageal candida infection on the 30th d after ESD, and completely recovered after 7 d of administration of oral fluconazole 100 mg/d. No other adverse events of oral steroids were found.CONCLUSION Oral prednisone (50 mg/d) and prolonged prednisone usage time may effectively prevent esophageal stricture after ESD without increasing the incidence of glucocorticoid-related adverse events. However, further investigation of larger samples is required to warrant feasibility and safety.
Key Words: Early esophageal cancer; Stenosis; Prednisone; Endoscopic submucosal dissection
INTRODUCTION
Endoscopic submucosal dissection (ESD) is one of main treatment measures for early esophageal cancer and esophageal high-grade intraepithelial neoplasia[1]. It is minimally invasive and permitsenbloc resection of large esophageal lesions without esophagectomy. However, esophageal stenosis generally occurs after ESD resection of esophageal lesions, especially for lesions ≥ 3/4 of the lumen. Multivariate analysis has shown that esophageal mucosal membrane defects over 3/4 of the lumen is an important predictor of stenosis formation. Without prophylactic treatment, the occurrence rate of esophageal strictures can reach 83.3%-94.1%; especially when the lesion affects the whole circumference of the esophagus, the rate of esophageal strictures is even higher[2,3]. This often requires repeated endoscopic balloon dilatation (EBD) to alleviate symptoms; however, the benefit is limited[4].
Recently, it has been reported that hormones, as a preventive treatment, can reduce the occurrence of stricture after esophageal ESD[5,6]. Yamaguchiet al[5] first reported that oral prednisone 30 mg/d can effectively prevent esophageal stenosis after ESD, and the postoperative stenosis rate can be reduced to 5.3% (1/19). A study also showed that oral prednisone 30 mg /d is not effective in preventing esophageal stenosis in patients with an entire circumference or ≥ 7/8 circumferential mucosal defects[7]. Meanwhile, one case reported that a patient with superficial esophageal squamous cell carcinoma received high-dose dexamethasone therapy (40 mg for 4 d) for multiple myeloma on the 9thd after ESD. After three courses of treatment, no esophageal stenosis was found in the follow-up gastroscopy, the histopathological evaluation showed that the submucosa became thinner, and the fibrosis degree of wound scar after ESD was the lowest[8]. In a prospective study by Nakamura, 11 patients with superficial esophageal squamous cell carcinoma with lesions ≥ 3/4 of the circumference were treated with steroid pulse therapy from the next day after ESD (intravenous infusion of sodium methylprednisolone succinate 500 mg/d for 3 consecutive days from the next day after ESD)[9]. It was found that although steroid pulse therapy was safe, steroid pulse therapy had no preventive effect on esophageal stenosis after ESD. Therefore, oral hormone is an effective method to prevent esophageal stenosis after esophageal ESD, but the dose, use time, effectiveness, and safety of the hormone need to be further studied.
MATERIALS AND METHODS
Patients
Between June 2019 and March 2022, 74 patients with superficial esophageal squamous cell carcinoma or precancerous lesions of esophagus wereen blocresected with ESD at the Digestive Endoscopy Center of Shenzhen People’s Hospital (Guangdong province, China). Of these, 18 patients accepted mucosal resectionviaESD, and the mucosal defects involved a 3/4 or larger circumference of the esophageal lumen. However, 1 patient who had received additional chemoradiotherapy (CRT) and 3 patients who had undergone additional surgery were removed from our study. Ultimately, 14 patients were included in this study. The indication criteria were as follows: (1) Before esophageal ESD, the intrapapillary capillary of the lesion mucosa observed by narrow band imaging magnifying endoscopy was type B1; (2) The preoperative lesions of ESD were histologically confirmed as superficial esophageal squamous cell carcinoma or esophageal high-grade intraepithelial neoplasia; (3) Thoracoabdominal enhanced computed tomography (CT) showed no lymph node or distant metastasis; (4) Provision of written informed consent was given; (5) There was no achalasia; and (6) There was no corrosive injury of esophagus. The exclusion criteria were as follows: (1) Patients who could not be followed up for 6 mo or longer; (2) patients whose stenosis formed before esophageal ESD; (3) patients who had prior esophageal cancer with CRT; and (4) patients with additional CRT or additional esophagectomy after non-curative ESD.
ESD procedure
The ESD was operated in an operating room. The patients were endotracheal intubated and kept in the left lying position. An endoscope (GIF-Q260J; Olympus Co., Tokyo, Japan) was attached with forward water delivery function and was used with carbon dioxide insufflation. The head end of the endoscope was connected with a pellucid cap (diameter 12.4 mm, length 4 mm, D-201-11804; Olympus Co.). Iodine 0.75% staining was used for identifying the range of the lesion, and a dual knife (KD-650Q; Olympus Co.) marking dots 3 mm away from the edge of the lesion. An electronic surgical workstation (VIO 200D; ERBE, Tübingen, Germany) was used with an operating mode (Forced Coagulation model, effect 2, maximum power 20 W). The 0.9% saline solution containing 0.3% indigo carmine was used for adequate submucosal injection along the marked dots. After circumferential mucosal incision, submucosal dissection was operated by the dual knife (KD-650Q) from the oral side to the anal side of the lesion under an operating mode (Endocut I mode, Forced Coagulation model, effect 2, maximum power 50 W, VIO 200D; ERBE). Bleeding during the operation and visible blood vessels were handled with hemostatic forceps (FD-410LR; Olympus Co.) under a soft coagulating mode (Soft Coagulation mode, effect 4, maximum power 80 W, VIO 200D; ERBE).
Postoperative-related bleeding was defined as bleeding requiring blood transfusion or surgical intervention, or bleeding that resulted in a 2 g/dL decline in hemoglobin levels. Postoperative-related perforation was diagnosed by endoscopy or chest CT[7]. All patients treated with proton pump inhibitor, esomeprazole, with a dose of 20 mg, twice a day after ESD for 28 d[5,9]. After ESD, each patient received two pieces of calcium carbonate and vitamin D3 chewable tablets (each tablet contains 300 mg calcium and 60 IU vitamin D3) per day until the prednisone was stopped to prevent glucocorticoid-induced osteoporosis[10].
Management for esophageal stenosis prevention
Prednisolone was taken orally at a dose of 50 mg/d from the next morning after ESD for 1 mo, and then decreased gradually (45, 40, 35, 30, 25, 20, 15, 10, and 5 mg for 7 d each) until 13 wk later.
Follow-up
Regular endoscopy was examined at 1, 3, and 6 mo after ESD operation, and then annually thereafter. In addition, endoscopic examination was performed whenever the patient had dysphagia to determine whether there was esophageal stenosis. EBD was performed subsequently if esophageal stricture was identified. Any abnormal mucosa required biopsy for pathological evaluation of whether there was local tumor recurrence. Meanwhile, regular physical and blood examinations were carried out to evaluate the side effects of the steroid. Bone mineral density testing was performed before ESD treatment and 6 mo after ESD treatment.
Outcomes
The main outcome measure was incidence of esophageal stenosis. Esophageal stenosis was defined as the inability of 9.9 mm diameter gastroscope (GIF-Q260J; Olympus) to pass through the esophageal stenosis. Secondary observation indicators of glucocorticoid-related adverse events were observed at 1, 3, and 6 mo after ESD such as newly diagnosed diabetes or aggravation of diabetes, pepticulcer, adrenocortical insufficiency, aggravation of osteoporosis or fracture, and corticosteroid-related mental disorders.
End point: The follow-up was terminated if tumor recurrence and serious adverse events of glucocorticoid and procedure-related complications (procedure-related bleeding and procedure-related perforation) occurred.
Statistical analyses
Continuous variables are presented as the mean ± standard deviation or median (interquartile range, 25%-75%). Categorical variables are expressed by proportion. Date analyses were conducted using SPSS 23.0 software (version 23.0 for Mac).
RESULTS
Background characteristics of patients
After ESD surgery, there were 18 patients with mucosal defects more than 3/4 of the esophageal circumference. One patient received additional CRT treatment, and 3 patients received additional surgery and were removed from this study. Eventually, a total of 14 patients met the criteria. Patients and characteristics of lesions are shown in Table 1 and Table 2. Male patients accounted for 64%, with a mean age of 62.1 years (ranging from 45 to 75 years). According to the Paris endoscopic classification,13 cases of endoscopic tumor morphology were classified as type 0-IIa and 1 case was type 0-IIc. The lesions were mainly located in the middle and lower esophagus, and 1 case was located in the upper esophagus. Each patient successfully received esophageal ESD treatment, and postoperative pathology confirmed that the lesion was completely removed. All patients had no procedure-related bleeding and procedurerelated perforation after esophageal ESD. The mean resection size was 55.5 mm in diameter (ranging from 47.5 mm to 65.0 mm). According to the range of esophageal mucosal defect, 11 cases involved ≥ 3/4 and < 7/8 circumference, 1 case involved ≥ 7/8 circumference, and 2 cases involved the entire circumference. The longitudinal extension of mucosal defect was < 50 mm in 3 patients and ≥ 50 mm in 11 patients. In 12 cases, the depth of invasion of pathological tissues was limited within the epithelium and lamina propria mucosa, whereas 2 lesions were limited within muscularis mucosa without lymphovascular infiltration.

Table 1 Background characteristics of patients, n (%)
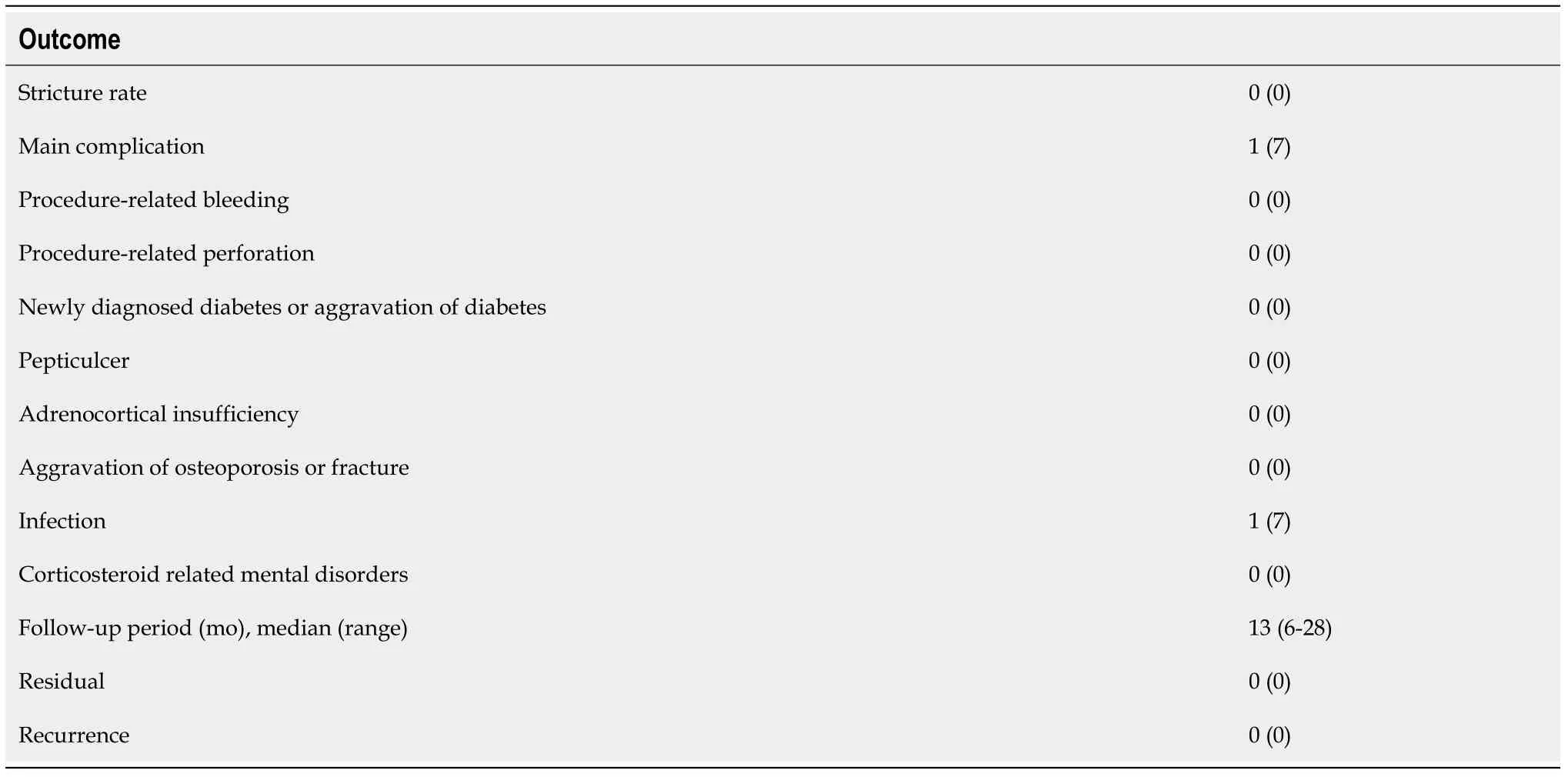
Table 2 The feasibility and safety of prophylactic treatment, n (%)
The shortest follow-up time of all cases was 6 mo, the longest follow-up time was 28 mo, and the median follow-up time was 13 mo. During this period, all patients were followed up by endoscopy regularly without dysphagia. The incidence of esophageal stenosis was 0% (0/14) (Table 3). Representative cases are shown in Figures 1 and 2.

Figure 1 Representative case (case 1). A 67-yr-old female who underwent endoscopic resection for large superficial esophageal squamous cell carcinoma. A:Endoscopic view of the tumor after Lugol’s staining. The tumor spread to more than 3/4 of the circumference of the esophageal lumen; B: Endoscopic view of the ulcer bed immediately after endoscopic submucosal dissection. The width of the mucosal defect was ≥ 3/4 and less than the entire circumference. Then oral steroid was administered as a prophylactic treatment; C: Endoscopic view on the 30th d. The mucosal defect was still undergoing re-epithelialization, and a 9.9 mm diameter gastroscope (Olympus GIF-Q260J) could pass. D: Endoscopic view on the 180th d; Complete epithelialization is shown and a 9.9 mm diameter gastroscope (Olympus GIF-Q260J) could pass without dysphagia.

Figure 2 Representative case (case 3). A 70-yr-old female who underwent endoscopic resection for large superficial esophageal squamous cell carcinoma. A:Endoscopic view of the tumor after Lugol’s staining. The tumor spread to about the entire circumference of the esophageal lumen; B: Endoscopic view of the ulcer bed immediately after endoscopic submucosal dissection. The width of the mucosal defect was the entire lumen circumference. Then oral steroid was administered as a prophylactic treatment; C: Endoscopic view 6 mo later. The mucosal defect underwent complete epithelialization, and an 9.9 mm diameter gastroscope(Olympus GIF-Q260J) could pass; D: Endoscopic view after 1 yr. The endoscope could pass without dysphagia.

Table 3 Clinical outcomes for 14 patients with early esophageal cancer after circumferential endoscopic submucosal dissection
Only 1 patient developed esophageal Candida infection on the 30thd after ESD and recovered completely after 7d of treatment with oral fluconazole 100 mg/d. Glucocorticoid-related adverse events were observed such as newly diagnosed diabetes or aggravation of diabetes, pepticulcer, adrenocortical insufficiency, aggravation of osteoporosis or fracture, and corticosteroid-related mental disorders.
DISCUSSION
In the current study, increasing the dose of oral hormone (prednisone acetate 50 mg/d) and prolonging the treatment time (13 wk) were effective to prevent esophageal stenosis in patients with mucosal defects ≥ 3/4 circumference after ESD. Studies have shown that the occurrence of esophageal stricture after ESD is related to the infiltration of postoperative inflammatory cells and vascular proliferation[11,12]. At the same time, epithelial cells proliferate and migrate from the edge of the wound after ESD, fibroblasts proliferate continuously, and finally fibrous scar is formed. This process is divided into three stages: acute inflammation, proliferation, and remodeling; however, the duration of this process is unknown. Through the dog model study, Honda found that within about 1 mo after esophageal EMR, the mucosal defect healed and was covered by squamous cells. Although the proper muscle layer was not damaged, muscle fiber atrophy still occurred in the 1stwk after operation, and finally fibrosis was formed[13]. Some clinical studies have also shown that esophageal stenosis mostly occurs within 2 to 4 wk after surgery[3,14], but this was confined to endoscopic observation. Glucocorticoid has a strong anti-inflammatory effect, which not only inhibits the synthesis of collagen but also promotes the decomposition of collagen to inhibit the formation of stenosis. In our study, all cases did not have esophageal stenosis after ESD. We believe that increasing the dose of prednisolone can enhance the antiinflammatory effect in the acute inflammatory period, especially in the critical period of the 1stmo after ESD. Meanwhile, we speculate that the process of esophageal stenosis may last longer than expected, and prolonging the usage of prednisolone may inhibit the proliferation of fibroblasts steadily to prevent esophageal remodeling and the formation of esophageal stenosis.
There are several reports on the application of steroids to prevent stenosis after ESD operation for large-area superficial esophageal squamous cell carcinoma and precancerous lesions. Yamaguchiet al[5] reported the therapeutic effect of oral prednisolone after esophageal ESD for the first time. In their report, prednisone was taken on the 3rdd after ESD, with an initial dose of 30 mg/d, and then decreased gradually (30, 30, 25, 25, 20, 15, 10, and 5 mg for 1 wk each). The incidence of stenosis after semi-circumferential ESD resection and entire circumferential ESD resection were 6.3% (1/16) and 0% (0/3), respectively[5]. However, for the cases of circumferential esophageal mucosal defect after ESD, Satoet al[15] found that oral prednisone 30 mg/d could not reduce the incidence of postoperative esophageal stenosis, but could decrease the total number of EBD expansions required. In Kadota’s[7] study, the stenosis rate of patients with less than entire circumferential ESD resection and with oral prednisone 30 mg/d administration was similar to the results by Yamaguchiet al[5], whereas patients with entire circumferential ESD resection showed higher stenosis rate (10/14) even with additional local submucosal steroid injections[7]. Meanwhile, two studies of submucosal injection of triamcinolone acetonide within the mucosal defects combined with oral prednisone in the prevention of esophageal stenosis post-ESD for lesions more than 3/4 circumference have obtained completely opposite results. Chuet al[16] reported that after treated with submucosal injection of triamcinolone acetonide within the mucosal defects combined with oral prednisone 30 mg/d, the incidence of esophageal stenosis was only 18.2% (2/11), including lesions with total circumferential resection. Surprisingly, in the Hanaokaet al[17] study of 12 cases with whole circumferential defect, the same steroid submucosal injection combined with oral prednisone 5 mg/d were used for post-ESD treatment; nevertheless, 11 patients failed to avoid postoperative stenosis. This discrepancy may be caused by different doses of orally-taken prednisolone in these studies. A study about short-term usage of oral prednisolone (30, 20, and 10 mg/d for 1 wk each) for mucosal defects ≥ 3/4 circumference, including 3 patients with total circumferential resection that showed a stenosis rate of 18% (3/17), and 1 of 3 patients with total circumferential resection withstood stenosis[18]. Accordingly, we speculate that the prevention of esophageal stenosis after esophageal ESD by oral prednisone was correlated with the dose and the use time. In our study, we increased the dose of prednisone to 50 mg/d and prolonged the treatment time to 13 wk. During our follow-up, 14 patients had no feedback of dysphagia symptoms, and no esophageal stenosis observed by endoscopic examination. Especially the 2 patients with entire circumference mucosal defects, although the esophageal wounds were fibrotic, the 9.9 mm diameter gastroscope (GIF-Q260J; Olympus) could pass, and we did not add EBD treatment. In addition, studies have shown that the injury of the intrinsic muscle layer was one of the risk factors for esophageal stenosis after ESD for early esophageal cancer and precancerous lesions[19,20]. Therefore, we paid more attention to avoid the injury of the intrinsic muscle layer as much as possible during ESD operation, which we think is also helpful for the prevention of postoperative esophageal stenosis.
Furthermore, systemic steroids are associated with adverse events, including newly diagnosed diabetes or aggravation of diabetes, pepticulcer, adrenocortical insufficiency, aggravation of osteoporosis or fracture, and corticosteroid-related mental disorders. Stucket al[21] showed that when the cumulative dose of oral prednisone exceeded 700 mg, the risk of infectious complications in patients taking prednisone increased with the increase of prednisone dosage. One study also found that even short-term steroid use is related to increased risks of adverse events[22]. However, in our protocol, the accumulated dose of oral steroids was 3075 mg, which was higher than that of other studies, and proton pump inhibitor, oral calcium, and vitamin D3 were taken simultaneously. One patient was found to have esophageal Candida infection on the 30thd after operation, and completely recovered after 7 d of oral fluconazole 100 mg/d therapy, and no patients experienced other adverse incidents related to orally-taken prednisolone. Therefore, we believe that the treatment scheme of increasing the dose of prednisone (50 mg/d) is safe, but still needs long-term follow-up and observation.
This study had several limitations. First, this study was a retrospective analysis in single-centered, and possible bias could not be avoided. Second, the follow-up time was insufficient and could not comprehensively evaluate the feasibility and safety of the hormone. Third, the number of subjects was relatively small, and the control group was lacking, so statistical difference analysis could not be conducted. Due to these limitations, prospective randomized controlled studies should be established to validate the efficacy and safety of prophylactic steroid therapy.
CONCLUSION
In conclusion, increasing the dose of oral prednisone (50 mg/d) and prolonging the usage time (total 13 wk) may effectively prevent esophageal stenosis after ESD to remove large-area superficial esophageal squamous cell carcinoma or precancerous lesions of esophagus, and does not increase the incidence of glucocorticoid-related adverse events.
ARTICLE HIGHLIGHTS
Research background
Esophageal stenosis is one of the main complications of endoscopic submucosal dissection (ESD) for the treatment of large-area superficial esophageal squamous cell carcinoma and precancerous lesions (≥ 3/4 of the lumen). Oral prednisone is useful to prevent esophageal stenosis, but the curative effect remains controversial.
Research motivation
Explore more effective methods to prevent esophageal stenosis after ESD for early esophageal cancer and precancerous lesions.
Research objectives
We shared our experience of the precautions against esophageal stenosis after ESD to remove large superficial esophageal lesions.
Research methods
Patients with large superficial esophageal squamous cell carcinoma and high-grade intraepithelial neoplasia experienced ESD were enrolled. Prednisone (50 mg/d) was administered orally on the 2ndd after ESD for 1 mo, and tapered gradually (5 mg/wk) for 13 wk.
Research results
According to the range of esophageal mucosal defect, 11 cases involved ≥ 3/4 and < 7/8 circumference, 1 case involved ≥ 7/8 circumference, and 2 cases involved the entire circumference. The incidence of esophageal stenosis was 0% (0/14), and only 1 patient developed esophageal Candida infection on the 30thd after ESD and recovered completely after 7d of treatment with oral fluconazole 100 mg/d.
Research conclusions
Further investigation of larger samples is required to warrant feasibility and safety.
Research perspectives
In conclusion, increasing the dose of oral prednisone (50 mg/d) and prolonging the usage time (total 13 wk) may effectively prevent esophageal stenosis after ESD removing large-area superficial esophageal squamous cell carcinoma or precancerous lesions of esophagus, and does not increase the incidence of glucocorticoid-related adverse events.
FOOTNOTES
Author contributions:Zhan SG and Wang LS were responsible for the design of the study and reviewed the manuscript; Zhan SG, Wu BH, Li DF, and Yao J extracted the data; Zhan SG, Xu ZL, Zhang DG, Shi RY, and Tian YH performed the data analysis; Zhan GS and Wang LS were responsible for revising the manuscript; All authors have read and approved the final manuscript.
Institutional review board statement:This study was approved by the Ethics Committee of Second Clinical Medical College of Jinan University, Shenzhen People’s Hospital (Approval No. LL-KY-2022150-02).
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Sheng-Gang Zhan 0000-0002-3318-2635; Ben-Hua Wu 0000-0002-9392-9470; De-Feng Li 0000-0003-3118-6840; Jun Yao 0000-0002-3472-1602; Zheng-Lei Xu 0000-0002-5413-7390; Ding-Guo Zhang 0000-0001-7728-9672; Rui-Yue Shi 0000-0001-9123-2103; Yan-Hui Tian 0000-0003-4671-2938; Li-Sheng Wang 0000-0002-7418-6114.
S-Editor:Liu GL
L-Editor:Filipodia
P-Editor:Liu GL
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
