Anti-reflux effects of a novel esophagogastric asymmetric anastomosis technique after laparoscopic proximal gastrectomy
Li-Qun Pang, Jie Zhang, Fang Shi, Cong Pang, Cheng-Wan Zhang, Ye-Liu Liu, Yao Zhao, Yan Qian, Xiang-Wei Li, Dan Kong, Shang-Nong Wu, Jing-Fang Zhou, Cong-Xue Xie, Song Chen
Abstract
Key Words: Esophagogastric junction tumor; Proximal gastrectomy; Digestive tract reconstruction; Esophagogastric asymmetric anastomosis; Reflux esophagitis; Gastroenterography
INTRODUCTION
Gastric cancer is a common malignant tumor of the gastrointestinal tract, with over 1 million new cases and 769000 deaths globally in 2020. It ranks fifth in terms of incidence and fourth in terms of mortality among malignant tumors[1].Interestingly, the proportion of proximal gastric cancer (including upper gastric cancer and adenocarcinoma of the esophagogastric junction) has been on the rise for the past 40 years[2-5].
For early esophagogastric junction tumors, esophageal-residual gastric anastomosis after proximal gastrectomy is an effective method to reconstruct the digestive tract. Compared to total gastrectomy, this method maintains normal anatomy and functionality of the stomach and duodenum, and improves nutritional status and quality of life of patients post-operatively[6,7].
However, the loss of anti-reflux function due to surgical resection of the cardia, the decline in gastric peristalsis due to vagotomy, and the emptying delay caused by preserved pylorus can lead to several postoperative complications such as intractable reflux esophagitis, anastomotic stomatitis and stenosis, Barrett esophagus, and esophageal cell carcinoma[8-12], impacting quality of life post-surgery.
To address reflux esophagitis, several different gastrointestinal reconstruction modalities have been developed over the years. The primary anti-reflux surgical modalities in current use involve several common strategies[13-16]: (1)Extending the distance to reduce reflux using jejunal inter-positioning or double tract reconstruction; (2) reducing discharge resistance to reduce reflux, such as pyloric molding; and (3) in the esophageal-residual gastric anastomosis,improving anti-reflux function by rebuilding the structure of the gastric base and anastomotic opening using approaches such as the double-flap technique (Kamikawa anastomosis) or removing most of the stomach to reduce gastric acid secretion,viagastric tube reconstruction.
However, each of these techniques has its own limitations in terms of insufficient effectiveness of anti-reflux in the supine position, inadequate storage function or delayed emptying of the residual stomach, inadequate flow of food through the duodenum, and complexity of surgical approach[17-20].
Esophagogastrostomy is considered the simplest reconstruction method used after proximal gastrectomy because it requires only one anastomosis, allowing easy postoperative endoscopic surveillance. A survey of 145 Japanese medical institutions showed that esophagogastric anastomosis was chosen for gastrointestinal reconstruction in approximately 50% of medical institutions[21,22]. However, it is not widely accepted because of severe postoperative complications such as reflux esophagitis and anastomotic stricture[11,12].
To improve the procedure of esophagogastric anastomosis to prevent reflux after proximal gastrectomy, we designed and implemented a novel reconstruction technique called esophagogastric asymmetric anastomosis (EGAA) based on years of clinical experience. Additionally, we established the EGAA mode to study the anti-reflux theory mechanism of asymmetric anastomosis aided by computer simulation technology using finite element analysis.
Herein, we present the technical details of EGAA and elaborate on its short-term outcomes after laparoscopic antireflux surgery.
MATERIALS AND METHODS
Critical features of the EGAA
There are four critical features of the EGAA method: The asymmetric cut of the lower esophagus, the asymmetry of the esophageal diameter in relation to the incision length in the anterior wall of the residual stomach, asymmetrical torsion of the esophagus with respect to the residual stomach, and asymmetrical suturing of the seromuscular layer of the residual stomach with the esophagus.
First, because of the oblique cut of the lower esophagus, the length of the anterior wall of the esophagus at the anastomotic site is approximately 1.5 cm longer than that of the posterior wall, forming a "door and block" frame with the folded stomach parts to prevent reflux and leakage after anastomosis (Figure 1A and D).
Second, a transverse incision was made in the anterior wall of the stomach about 3.5 cm from the proximal end of the residual stomach. The length of the incision is approximately 3.2-3.5 cm that is greater than the diameter of the esophagus but equal to the length of the distal oblique incision in the flat state of the esophagus (i.e., half of the circumference of the distal oblique incision).
This design facilitates the closure of the lower end of the esophagus and helps to prevent stenosis (Figure 1A). The following formula was applied to improve the grasp of the criteria for the size of the anterior gastric wall incision:
Criterion length of gastric incision size (cm) ≈(where r is the esophageal radius and g is the gap between the front and rear lengths of the esophageal wall).
Third, the esophagus and the residual stomach are asymmetrical on the sagittal surface after suturing the lower segment of the esophagus, which has undergone a 90-degree anticlockwise torsion, to the anterior incision of the residual stomach in an end-to-side anastomosis (Figure 1B). Both the distal esophagus and anastomotic sites tended to close in a resting state.
Finally, in the posterior wall of the anastomosis, the edge of the gastric stump (about 3.0 cm from the anastomosis) is sutured to the seromuscular layer of the esophagus (0.5-1.0 cm from the anastomosis) to form a flap-like structure by folding the wall of the partial residual stomach in the gastric lumen.
The criteria for this procedure were as follows: Except for the gastric margin of approximately 0.3 cm for the anastomosis, the distance between the gastric stump margin and the suture site of the posterior esophageal wall must be greater than 2.5 cm. The length of the valve-like structure formed by the folded gastric wall must be longer than 1.0 cm to ensure the effectiveness of closure.
In the anterior wall of the anastomosis, the seromuscular layer of the residual stomach and esophagus was sutured,pushing the anterior lip toward the posterior lip of the anastomosis and increasing the tendency for anastomotic closure in synergy with asymmetrical suturing of the posterior wall of the anastomosis (Figure 1C and D).
Computer simulations of EGAA mechanisms using the finite element method
To determine whether the procedure for asymmetric anastomosis of the esophagus and stomach could achieve the expected outcome theoretically, simulations were performed according to the procedure for EGAA (Figure 1D). The contraction movement of the stomach was modeled by applying thermal strain. Rubber materials were used to simulate the elastic behavior of the stomach and esophagus. Additionally, the esophageal and duodenal ends are restricted as displacement boundary conditions, and the pressure inside the stomach was also considered.
Adobe Illustrator was used to draw the curve of the gastric section (Figure 2A). The gastric curve was then transferred into SolidWorks to generate the geometric model, and this was then used to perform the finite element simulation using the ANSYS Workbench.

Figure 1 Critical design features of the esophagogastric asymmetric anastomosis technique. A: (1) The diameter of the esophagus and the incision size of the residual gastric anterior wall are asymmetric; and (2) The length of the two sides of the lower esophagus is asymmetrical; The points a/b/c/d shows the corresponding points of asymmetric anastomosis respectively between esophagus and residual stomach; B: Asymmetry of the longitudinal section (or sagittal surface) of the esophagus and the residual stomach after anastomosis; C: After anastomosis, the seromuscular layer of the residual stomach and esophagus is asymmetrically sutured; D: The sagittal plane of esophagogastric asymmetric anastomosis: Showing the suture point of the asymmetric anastomosis; the red arrow indicates a flap structure formed by the folded gastric wall in the gastric cavity.
Patients
Thirteen patients (9 males and 4 females) were recruited for laparoscopic proximal gastrectomy (LPG) with EGAA at the Affiliated Huaian No. 1 People's Hospital of Nanjing Medical University between September 2021 and March 2023. One patient had a gastric stromal tumor. The other 12 patients had tumors that were histologically confirmed as adenocarcinoma of esophagogastric junction (AEG). The age range was 57-78 years (66.3 ± 7.0), with body mass index (BMI,kg/m2) ranging from 21.3-32.4 (24.5 ± 3.0).
Preoperative diagnosis and evaluation included endoscopy, upper gastrointestinal series, and computed tomography(CT). Tumor stages were classified according to the International Anti-Cancer Alliance TNM staging system[23], and lymph node stations were numbered according to the definition of the Japanese Gastric Cancer Association[24]. Surgical complications were classified according to the Craven-Tindo classification[25]. Endoscopic evaluation of esophagitis was performed using the Los Angeles classification[26].
Surgical technique
Mobilization and transection of the stomach and lymphadenectomy: Under general anesthesia, patients were placed in the reverse Trendelenburg position with their legs apart. The surgeon and the first assistant were positioned on the right and left sides of the patient, respectively. After pneumoperitoneum was established using an open technique at the umbilicus and maintained at approximately 13-15 mmHg abdominal pressure, an electro-laparoscope was introduced through the 12-mm umbilical trocar before placing the remaining four working trocars (Figure 3A).
Omentectomy was performed along the superior edge of the transverse colon. The right parts of the omentum were dissected from the mesocolon around the transition zone of lymph node (LN) stations 4d-6, and the right gastroepiploic vessels were preserved.

Figure 2 Computer simulations of esophagogastric asymmetric anastomosis mechanisms using the finite element method. A: Adobe Illustrator was used to draw the curve of the gastric section; B: The valve-like structure of the folded gastric wall and the posterior wall of the lower esophagus move to the upper left side like a lever at the site of anastomotic stoma, causing tightening of the anastomotic stoma; C: Because of the increased pressure in the gastric cavity and the expansion of the gastric fundus, the folded gastric wall and the esophageal wall moved to the left, which effectively tightened the anastomotic stoma.
The origin of the left gastroepiploic vessel (LGEV) was divided and ligated using hemo-clips. Dissection of the short gastric vessels (SVG) was continued along the spleen up to the esophagogastric junction before performing lymphadenectomy, including LNs 4sb and 4sa along the LGEV and SVG. The stomach was then elevated and the peritoneum along the superior edge of the pancreas was mobilized. LNs along the left gastric artery (No. 7), common hepatic artery (No.8a), celiac artery (No. 9), and proximal splenic artery (No. 11p) were retrieved. The root of the left gastric artery in the coronary vein was clipped and divided. The esophagogastric junction was mobilized. After complete exposure of the abdominal esophagus with the division of the anterior and posterior vagal trunks, LPG was completed by transection of the esophagus 2 cm proximal to the tumor with a 45-mm endoscopic linear stapler. The right pericardial (No. 1), left pericardial (No. 2), lesser curvature (No. 3), and lower thoracic para-esophageal nodes (No. 110) were completely retrieved using this procedure.
Proximal gastrectomy with an assisted abdominal incision: A small incision was made in the upper abdomen, and the stomach was exteriorized and stapled using a 60-mm linear cutting suture about 4 cm from the distal end of the tumor.The proximal margin of the specimen was examined pathologically when necessary. At the anterior wall 3.5 cm from the proximal end of the residual stomach, the transverse incision was marked and cut approximately 3.2-3.5 cm (Figure 3B).
Procedure of laparoscopic-assisted EGAA: The residual stomach was placed back into the abdominal cavity, the incision was temporarily closed, and pneumoperitoneum was re-established. A laparoscopic-assisted EGAA (hand suture) was performed following the critical features outlined previously.
The distal end of the esophagus was incised with an oblique short right and long left margin, with a difference of approximately 1.5 cm between the two sides (Figure 3C).
With a longitudinal anticlockwise torsion of the esophagus at 90°, an end-to-side anastomosis was performed between the cut end of the esophagus and the residual stomach incision.
First, one full-thickness intermittent suture was performed between the right side (point d) of the lower esophagus and the middle point (point d) of the posterior wall in gastric incision. Then, the right point of the gastric wall incision (point a) was sutured to the middle point (point a) of the anterior wall in the lower esophagus, and the left point (point b) of the gastric incision was sutured to the middle point (point b) of the posterior wall in the lower esophagus (Figure 3D). After this three-stitch full-layer suture was used to complete the positioning suture of the posterior wall of the EGAA, the points a/b/d of the esophageal and gastric wall incisions were aligned in the posterior wall of the anastomosis(Figure 1A), and the lower esophageal segment was rotated anticlockwise at 90°. The whole muscle layer was continuously sutured in the posterior and anterior walls of the anastomosis with ETHICON SXMD1B405 (tensile strength size 3-0) (Figure 3E and F), and the anterior wall of the anastomosis was further strengthened by a suture in the seromuscular layer (Figure 3G).
Then, 50 mL saline with 2 mL methylene blue was injected through the gastric tube (dimensioning 35 cm) to confirm that no anastomotic leak occurred.
The cut end of the residual stomach (approximately 3.0 cm from the anastomosis) was sutured with 3-5 stitchs to the posterior wall of the esophagus at a site 0.5-1.0 cm from the anastomosis in the seromuscular layer (Figure 3H). The residual stomach was sutured fixedly to the bilat with 3-5 stitchs eral diaphragmatic feet.
Ethical considerations
This study used clinicopathological, surgical, and follow-up data. All patients were counseled about the operative procedure, including the potential merits and disadvantages of our approach and the uncertainty of clinical outcomes. All patients were in stable condition and written informed consent was obtained from each patient prior to the procedure. All experimental and surgical procedures of the study were approved by the ethics committee of The Affiliated Huaian No. 1 People's Hospital of Nanjing Medical University and strictly adhered to the guidelines of the Helsinki Declaration of 1964 and its latest amendments.

Figure 3 Surgical Procedure of laparoscopic-assisted esophagogastric asymmetric-anastomosis. A: Reverse Trendlenborg position with both legs separated. Using five-hole method, the points I-V show the location of Trocars and operators respectively; B: The transverse incision of residual stomach wall is about 3.2-3.5 cm away from the proximal end at approximately 3.5 cm; C: The lower end of the esophagus is cut oblique, the length of both sides is asymmetric, the difference is approximately 1.5 cm; D: First, a full-thickness intermittent suture was performed between the right side (point d) of the lower esophagus and the middle point (point d) of the posterior wall in gastric incision. Then, the right point of the gastric wall incision (point a) was sutured to the middle point (point a) of the anterior wall in the lower esophagus, and the left point (point b) of the gastric incision was sutured to the middle point (point b) of the posterior wall in the lower esophagus.After performing a three-needle whole-layer positioning suture of the posterior wall in oesophagogastric anastomosis, oesophageal torsion was completed at a 90°anticlockwise; E: The back wall of the anastomosis was continuously stitched; F: The front wall of the anastomosis was continuously stitched; G: The seromuscular layer of the anterior wall of the anastomosis was further stitched; H: The residual gastric cutting end (approximately 3 cm from the anastomosis) was stitched to the posterior wall of the esophagus, about 0.5-1 cm away from the anastomosis.
RESULTS
Gastric peristalsis was simulated using the thermal-strain method. After decreasing the temperature, the model size was reduced by 30% in a clockwise direction. However, the suture of the incisal gastric margin and the posterior esophageal wall caused the valve-like folded gastric wall and posterior lower esophageal wall to move to the upper left, tightening of the anastomotic stoma (Figure 2B, Video 1).
Gastric fundus dilation simulation
To simulate the dilation of the reconstructed gastric fundus under gastric peristalsis and intragastric pressure, we applied different pressures to the gastric fundus, gastric body and antrum. During gastric peristalsis and contraction, the gas and liquid contents in the gastric cavity were observed to flow to the proximal end, increasing the pressure and expanding the gastric fundus gradually. According to the simulation results, because of the increased pressure in the gastric cavity and the expansion of the gastric fundus, the folded gastric wall and the esophageal wall moved to the left, tightening the anastomotic stoma (Figure 2C).
Following the simulations, EGAA surgeries were performed. All procedures were completed with a mean operation time of 304.2 ± 44.3 min, and the mean blood loss was 88.5 ± 46.3 mL. No intraoperative complications, conversions, or operative mortality was observed in the 13 patients. Two postoperative complications (minor grade II anastomotic leakage, cured conservatively) occurred, and patients recovered (median postoperative hospital stay: 19.2 ± 11.7 d).Patient background and surgical outcome are shown in Table 1.
One week post-surgery, abdominal CT examination (oral CO2powder) revealed that 11 patients had valve-like structures, inflatable stomach cavity and closed anastomosis (Figure 4). Upper gastroenterography showed good residual gastric excretion, no anastomotic leakage/stenosis, and no reflux (all patients, upright position). In supine/low head positions, eight patients exhibited no gastroesophageal reflux, three had mild reflux, and two had obvious reflux(Figure 5, Video 2).
Gastroscopy during postoperative follow-up (2 to 19 mo) revealed a closed valve-like structure at the anastomosis site in 11 patients. Additionally, good extensibility and gastric residual discharge were observed, with no signs of stenosis or apparent reflux esophagitis. Only two patients exhibited an uncharacteristic valve-like structure and reflux esophagitis(class LA-B, Los Angeles classification). Inverted gastroscope revealed a reconstructed gastric base (all patients), with 11 patients showing good coverage by the gastric mucosal valve-like structures at site of anastomosis. Follow-up endoscopic findings in representative cases are shown in Figure 6 and Video 3).
In the average 10.2 ± 6.2 mo of questionnaire follow-up, 11 patients recovered well with no symptoms such as stomach distension, heartburn, and dysphagia. Two patients exhibited gastroesophageal reflux (controlled by proton pump inhibitors, gastric dynamic drugs, and functional exercise). No recurrence or fatalities occurred during the median 10.2-month follow-up period (range, 2-19 mo).
By last follow-up, of the 13 EGAA surgery patients, four lost weight (one developed fatty diarrhea postcholecystectomy 6 month post-surgery). Five patients showed no change in body weight and four showed weight gain.The specific changes in BMI are shown in Table 1.
DISCUSSION
Esophagogastrostomy is considered the simplest and most convenient reconstruction procedure following proximal gastrectomy, as it preserves digestion and absorption. However, it is associated with a high incidence of reflux esophagitis and anastomotic stenosis, which significantly impact the patient's quality of life[21,27].
There are three problems to be addressed for anastomosis stoma of the esophagus and stomach to alleviate postoperative complications such as reflux and anastomosis stenosis[28-30]: (1) Maintaining closed state of anastomosis stoma and reducing gastric fluid reflux in the supine position; (2) maintaining gastric cavity tension to prevent weakness and gastric retention; and (3) prevent anastomosis narrowing.
To overcome these problems, we designed a four-asymmetric suture technique to reconstruct the gastric fundus and form a valve shape by folding part of the residual stomach wall at the posterior lip of the anastomosis in the gastric cavity. To improve study design processes and confirm a specific anti-reflux function, a computer simulation was applied using finite element analysis.
The anti-reflux effect of asymmetric anastomosis was further evaluated by imaging and endoscopy post-operatively.Abdominal CT examination (oral CO2) showed circular expansion of the residual stomach cavity, and a valve-like tightly closed stoma at the site of anastomosis. The CO2did not leak easily, confirming the "one-way valve" function. Upper gastroenterography showed good efficiency of stomach discharge or excretion to the small intestine, no gastric weakness,and no reflux even when most of the patients reached 15° in the supine and head lowered position, indicating an antireflux effect of the reconstructed anastomosis. Digestive endoscopy showed that the anastomosis was not narrowed,softened, or extended and had no mucus lake in the gastric cavity. The reconstructed gastric base and valve-like structures were observedviaan inverted gastroscope and revealed the gastric mucosa wrapped around the mirror body wall.
The results of our computer simulation and theoretical analysis further support the findings of the clinical examination.The computer simulation results demonstrate that during the peristaltic state, the folded stomach wall and the esophageal wall move in a clockwise forward motion, primarily due to the suture fixation of the residue and the rear wall of the esophagus. This movement leads to further tightening of the anastomosis stoma. Additionally, the expansion of thegastric cavity through increased peristaltic pressure applies pressure on the lower esophageal tissue, resulting in an enhanced anti-reflux effect.

Table 1 Preoperative data and clinical outcome of the patients
Based on the above results, we speculate that in the resting state, the anastomotic stoma and lower esophageal end are closed by four synergistic actions: longitudinal torsion of the lower section of the esophagus, asymmetric size of the esophageal diameter and residual gastric wall incision, suture of the seromuscular layer in the anterior wall, and the valve-like structure at the site of the posterior wall of the anastomosis stoma, acting as an anti-reflux function.Meanwhile, the joint effect of the pylorus can maintain a certain pressure in the stomach cavity, promote gastric emptying, and reduce the symptoms of fullness and discomfort caused by stomach retention.

Figure 4 Abdominal computed tomography (oral CO2 powder). A: coronal surface: The valve-like structure can be seen at the anastomosis, tightly closed;B: Sagittal plane: The gastric cavity is inflated, seeing the anastomotic valve-like structure with gear sample occlusion and a small amount of gas overflow in the esophagus.

Figure 5 Upper gastrointestinal tract angiography. A and B: Upright position: Unobstructed anastomosis, such as a normal cardia-like image; C and D:Head low foot high level: See the anastomosis is completely closed, no contrast agent reflux.
Three functional changes may occur in the state of gastric peristalsis: (1) With gastric contraction and an increase in gastric cavity pressure, gastric reflux to the esophagus occurs, pushing the valve-like stoma and further closing the anastomotic site. This valve-like structure functions as a unidirectional valve that is not prone to slip and cause reflux and leakage. However, while eating, the peristaltic pressure of the proximal esophagus and esophageal expansion by food clumps make the valve-like structure move distally but does not affect the passage of food; and (2) With peristalsis carried out from proximal to distal, the relaxation of the reconstructed gastric fundus and the subsequent passive expansion also have a certain anti-reflux effect on the compression of the lower end of the esophagus. According to computer simulation results, when the stomach contracts and shrinks, the valve-like structure moves to the upper left side, tightening the anastomotic stoma.
During follow-up, the majority of patients showed satisfactory recovery outcomes, except for two early EGAA patients who developed complications of reflux esophagitis, characterized by acid reflux and belching. This suggests that the four different asymmetric suture techniques might not have met the design standards due to lack of practical experience in the early stage of attempting the surgery, leading to incomplete closure of the valve-like structure, a half-folded gastric wall,and poor anti-reflux effect. However, with experience and improved surgical techniques, subsequent EGAA procedures were successful in achieving good anti-reflux effects, as observed in 11 patients. Notably, in the last 8 patients, gastroenterography revealed no reflux even in the supine and low head positions.
Finally, despite the advantages of our new approach, we acknowledge the limitations of the present study. As this was a single-center study with a small number of patients, more objective comparisons in multicenter trials are required to validate the procedure. Moreover, as a new technique, this requires a learning curve for surgeons to gain the necessary skills before satisfactory results can be achieved.
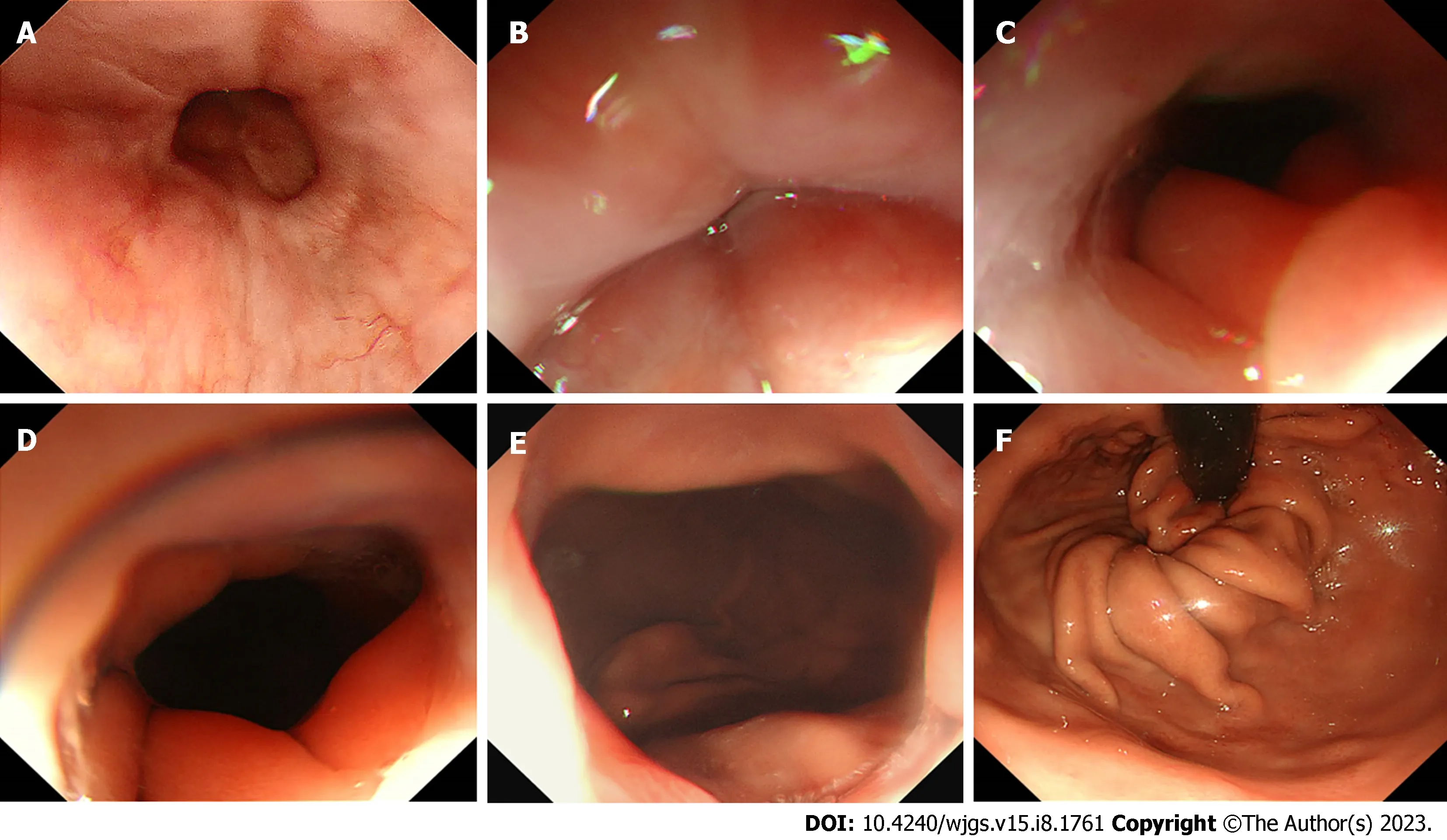
Figure 6 Gastroscope. A: The esophageal mucosa is smooth, without hyperemia and edema, with a clear capillary network; B: The valve-like structure of the anastomosis is closed in the non-inflated state; C-E: The valve-like structure of the anastomosis opens gradually in the inflated state, with good dilation and extensibility, showing a visible dentate linear-like structure; F: The reconstructed gastric base can be seen under the inverted gastroscope, which was wrapped well by the valve-like structures of the folded gastric wall mucosa at the site of the anastomosis;
CONCLUSIONS
In this clinical study, we designed the valve-like structure and anti-reflux function of the EGAA. The surgical procedures we adopted adhered to basic medical principles as well as being relatively easy to master. The clinical outcomes of 13 patients indicated that this surgical technique is practical, safe, and reliable. However, it is necessary to further investigate its long-term anti-reflux effectiveness with more patients and randomized controlled studies.
ARTICLE HIGHLIGHTS

ACKNOWLEDGEMENTS
We would like to thank Xu C and Xu R for the technical assistance in this study.
FOOTNOTES
Author contributions:Pang LQ, Zhang J, Shi F, Pang C and Chen S conceived and designed the study; Pang LQ and Zhang J performed the operation; Zhang CW, Shi F, Pang C, Liu YL, Zhao Y, Qian Y, Li XW, Xie CX, Kong D, Wu SN, Zhou JF and Chen S contributed to the study design, analysis, and interpretation of the data; Pang LQ and Chen S wrote the manuscript; all authors reviewed and approved the manuscript; Pang LQ, Zhang J, Shi F, Pang C and Chen S contributed equally to this work.
Institutional review board statement:All experimental and surgical procedures of the study were approved by the ethics committee of The Affiliated Huaian No. 1 People's Hospital of Nanjing Medical University and strictly adhered to the guidelines of the Helsinki Declaration of 1964 and its latest amendments.
Informed consent statement:All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Data sharing statement:The data that support the findings of this study are available on request from the corresponding author.
STROBE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Li-Qun Pang 0000-0003-0624-6362; Shang-Nong Wu 0000-0003-2102-5269; Song Chen 0000-0001-6412-5740.
S-Editor:Yan JP
L-Editor:A
P-Editor:Cai YX
1Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries.CA Cancer J Clin2021; 71: 209-249 [PMID: 33538338 DOI:10.3322/caac.21660]
 World Journal of Gastrointestinal Surgery2023年8期
World Journal of Gastrointestinal Surgery2023年8期
- World Journal of Gastrointestinal Surgery的其它文章
- Initial suction drainage decreases severe postoperative complications after pancreatic trauma: A cohort study
- Vascular complications of chronic pancreatitis and its management
- Historical changes in surgical strategy and complication management for hepatic cystic echinococcosis
- Post-transplant biliary complications using liver grafts from deceased donors older than 70 years:Retrospective case-control study
- Goldilocks principle of minimally invasive surgery for gastric subepithelial tumors
- Prognosis after splenectomy plus pericardial devascularization vs transjugular intrahepatic portosystemic shunt for esophagogastric variceal bleeding
