Comparison between upfront surgery and neoadjuvant chemotherapy in patients with locally advanced gastric cancer: A systematic review
Stylianos Fiflis, Menelaos Papakonstantinou, Alexandros Giakoustidis, Gregory Christodoulidis, Eleni Louri,Vasileios N Papadopoulos, Dimitrios Giakoustidis
Abstract
Key Words: Gastric cancer; Locally advanced gastric cancer; Neoadjuvant chemotherapy; Surgery; Survival
INTRODUCTION
According to Globocan there were 1089000 new cases of gastric cancer (GC) and 768000 GC related deaths worldwide in 2020 with almost twice the prevalence and mortality in males than in females. The highest prevalence is observed in Eastern Asia whereas the lowest in Africa and the highest mortality rate in Eastern Asia while the lowest in Northern America, Australia and Europe. GC is subcategorized according to Lauren’s classification into intestinal and diffuse subtypes which demonstrate different epidemiology, clinical behavior, chemoresistance, progression and prognosis but there have been no trials or analyses to evaluate whether these two subtypes would potentially benefit more from different treatment modalities[1].
Locally advanced GC (LAGC) is defined as T2 or higher clinical disease, with or without nodal involvement, and surgical resection with an adequate D2-lymphadenectomy is the cornerstone of the medical approach with curative intent alongside with other perioperative treatments such as chemotherapy and radiotherapy[1]. The role of neoadjuvant chemotherapy (NAT) is being rigorously studied as an important treatment regimen that aims to eliminate micrometastasis, downstage tumors and thus prolong OS, DFS and improve recurrence and R0 resection rates. LAGC patients are at high risk of developing distant metastases therefore they should be offered NAT. And patients who undergo surgery without NAT are at high risk of recurrence and should be submitted to adjuvant chemoradiation[2].
Even though NAT is being offered to patients with LAGC in Europe and the United States, the treatment regimens differ between the Western and the Eastern countries. For instance, adjuvant chemoradiotherapy is largely administered in the United States, neoadjuvant followed by adjuvant chemotherapy in the United Kingdom and solely postoperative chemotherapy is administered in Korea and Japan according to INT0116 trial, MAGIC trial, ACT-GC trial and CLASSIC respectively[3-6]. In this systematic review we assess the role of NAT in patients undergoing surgery for LAGC. We aim to investigate the approach that offers the highest overall survival (OS) and disease-free survival (DFS) rates.
MATERIALS AND METHODS
Search strategy
A thorough literature search was performed in PubMed using the terms “gastric cancer”, “locally advanced gastric cancer”, “adjuvant chemotherapy”, “neoadjuvant chemotherapy”, “perioperative chemotherapy”, “upfront surgery” and“surgical resection” in various combinations. The search yielded 648 results and after excluding duplicates and irrelevant studies by title and abstract, 36 were assessed for full text screening and 18 were finally included in the review. The study selection algorithm is shown in the PRISMA flowchart in Figure 1[7]. Our study protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO, ID CRD42023405111) and the date of the last search was February 18th, 2023.
Data extraction
Two reviewers (Fiflis S and Papakonstantinou M) independently completed the search and extracted the following data into a predetermined datasheet form: Author, year of publication, sample size, population sex and age, follow-up period,TNM stage, esophagogastric junction tumor involvement, length of hospital stay, type of surgery, chemotherapy regimens, OS and DFS rates, mortality and morbidity of the patients, R0 resection rates and tumor recurrence.
Inclusion and exclusion criteria
We included studies in the English language published over the last decade up until February 2023. The inclusion criteria were studies with patients with LAGC who had received no prior treatment and would undergo surgical resection and/or NAT. The outcomes of the studies should include data on the survival of patients after NAT and surgery and compare them to upfront surgery (US). Cohorts of patients with metastases before surgery and studies with less than 10 participants were excluded. Pilot studies, studies investigating predictive factors, case reports and letters to the editor or comments were also excluded (Table 1).
Risk of bias assessment
The risk of bias of each individual cohort study included in our systematic review was assessed with the Cochrane Tool to Assess Risk of Bias in Cohort Studies. This tool consists of the following 8 questions: (1) Was selection of exposed and non-exposed cohorts drawn from the same population? (2) Can we be confident in the assessment of exposure? (3) Can we be confident that the outcome of interest was not present at the start of the study? (4) Did the study match exposed and unexposed for all variables that are associated with the outcome of interest or did the statistical analysis adjust for these prognostic variables? (5) Can we be confident in the assessment of the presence or absence of prognostic factors? (6)Can we be confident in the assessment of outcome? (7) Was the follow up of cohorts adequate? and (8) Were cointerventions similar between groups? Depending on the answer, which varies from definitely yes to probably yes,probably no or definitely no, each study is classified as low or high risk of bias.
RESULTS
The original search yielded 648 results and after excluding irrelevant and duplicate papers, 18 studies with 4839 patients in total were included in our systematic review[8-25]. The demographics and the clinical characteristics of the patients are shown in Table 2. All patients were treated for LAGC and were separated into two groups; one receiving NAT and then undergoing surgical resection (NAT group) and the other undergoing US (US group). After the initial intervention the patients received either adjuvant chemotherapy or radiotherapy or no adjuvant treatment at all. The outcomes of interest were primarily the OS, the DFS and the morbidity and mortality rate, and secondarily the R0 resection rate. Seven of the studies included were propensity score-matched analyses[10,11,16,21-24]. Only the results of the matched groups were included in our study.
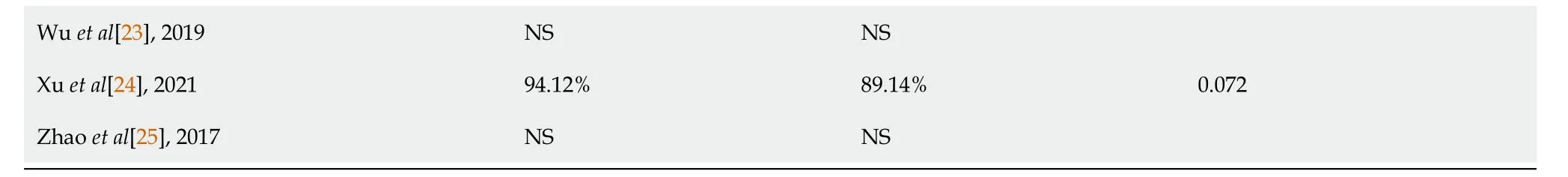
Survival, morbidity and mortality
The OS ranged from 41.6% to 74.2% in the NAT group and from 30.9% to 74% in the US group[14,15,20,21]. The difference was statistically significant in 5 studies[11,21,22,24,17]. Details on the OS and the DFS of each of the included studies can be found in Table 3. In general, the OS was greater in the NAT group in all of the studies except for one,where the OS was 70% in the NAT and 74% in the US group (P> 0.05)[14]. Of note, Linet al[17] in their study compared the results between Eastern and Western institutions. The difference in OS of patients with LAGC treated with NAT or US was significantly different in the Eastern cohort (60.1%vs49.3% respectively,P= 0.02). In the Western cohort the OS of patients who received NAT was 57.3% and 39.5% for those undergoing US (P= 0.11)[17]. The greatest difference in OS was reported in the study of Xuet al[24] where after NAT the OS reached 72.29%, while after US it was as low as 36.22% (P< 0.001)[24].
The highest DFS was reported in the NAT group of the Kanoet al[16] cohort and was statistically significantly higher than that of the US group (80%vs58.7%,P= 0.037). In all of the studies included, except for one, the DFS was longer after NAT, however the difference was statistically significant in 4 studies[16,24,15,13]. Bracaleet al[10] reported greater DFS in the US group, but the difference was not significant (75%vs71% after NAT,P= 0.34).
The complications related to the chemotherapy or the surgery ranged from 6.4% to 38.1% in the NAT group and from 5% to 40.5% in the US group[10,16,19,22]. The difference in morbidity between the two groups was statistically significantin two studies. In the study of Bracaleet al[10] the morbidity was 38.1% in the NAT group and 21.6% in the US group (P=0.019). In the study of Xuet al[24] the morbidity after NAT was 6.79%, while after US it was 12.67% (P= 0.037). The morbidity varied among the studies and depended on multiple factors included but not limited to chemotherapy regimen, patient status, surgical team experience, surgical technique and the extend of the disease and as a result a general conclusion could not be drawn. More detailed information is shown in Table 4. Among all the studies, death was more common in the US groups. In 7 studies no deaths occurred in the patients who received NAT, in 3 of which the mortality of the counterpart US group was 2.1%, 2.1% and 3.7% (Table 4)[8-10]. Finally, the highest mortality rate was observed in a US group, however it was not significantly different than that of the NAT group (5.3%vs2.8%,P= 0.142)[20].
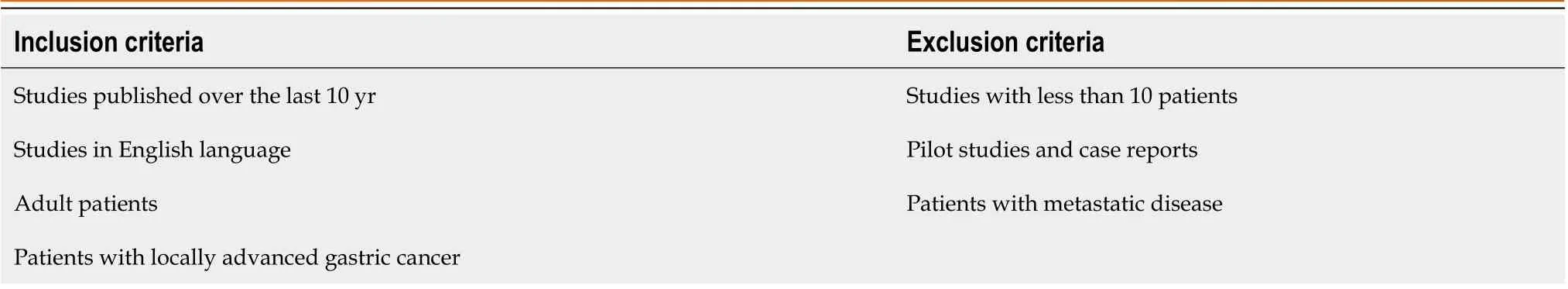
Table 1 Inclusion and exclusion criteria
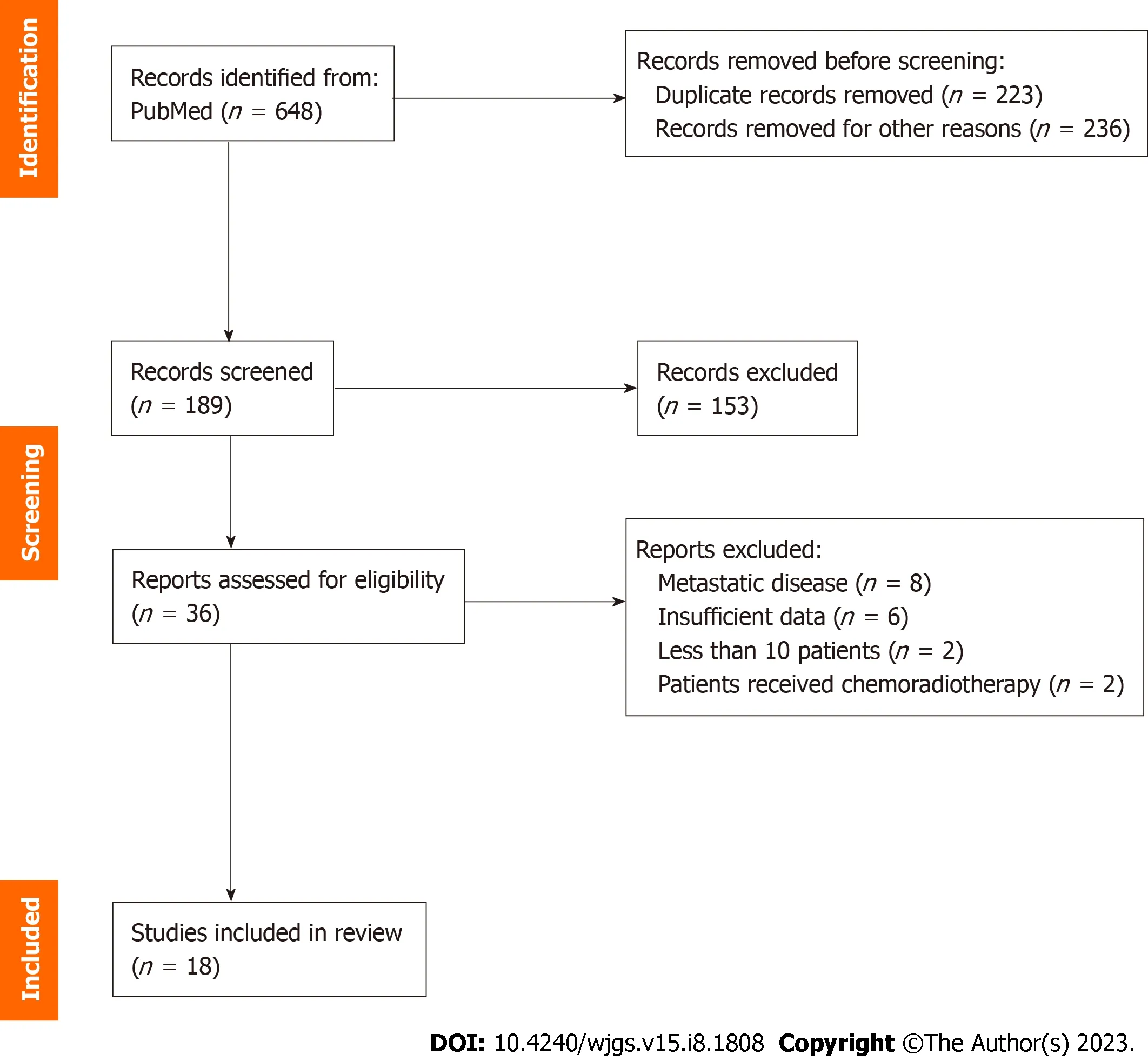
Figure 1 PRISMA flowchart.
R0 resection
Our secondary endpoint was the comparison of the R0 resection rate between patients who received NAT and those who underwent US (Table 5). The R0 resection rates were not statistically significantly different among all the studies except for one. In the study of Wanget al[13], 84.6% of the patients underwent a complete tumor resection after NAT, while the corresponding percentage for the US group was significantly lower (56.7%,P= 0.029). In a subgroup analysis where they compared neoadjuvant cheomoradiotherapy with NAT they showed that neoadjuvant cheomoradiotherapy resulted to better R0 resection rate, although not statistically significantly different (96%vs89%,P= 0.06)[22].

Table 2 Patient demographics and clinical characteristics
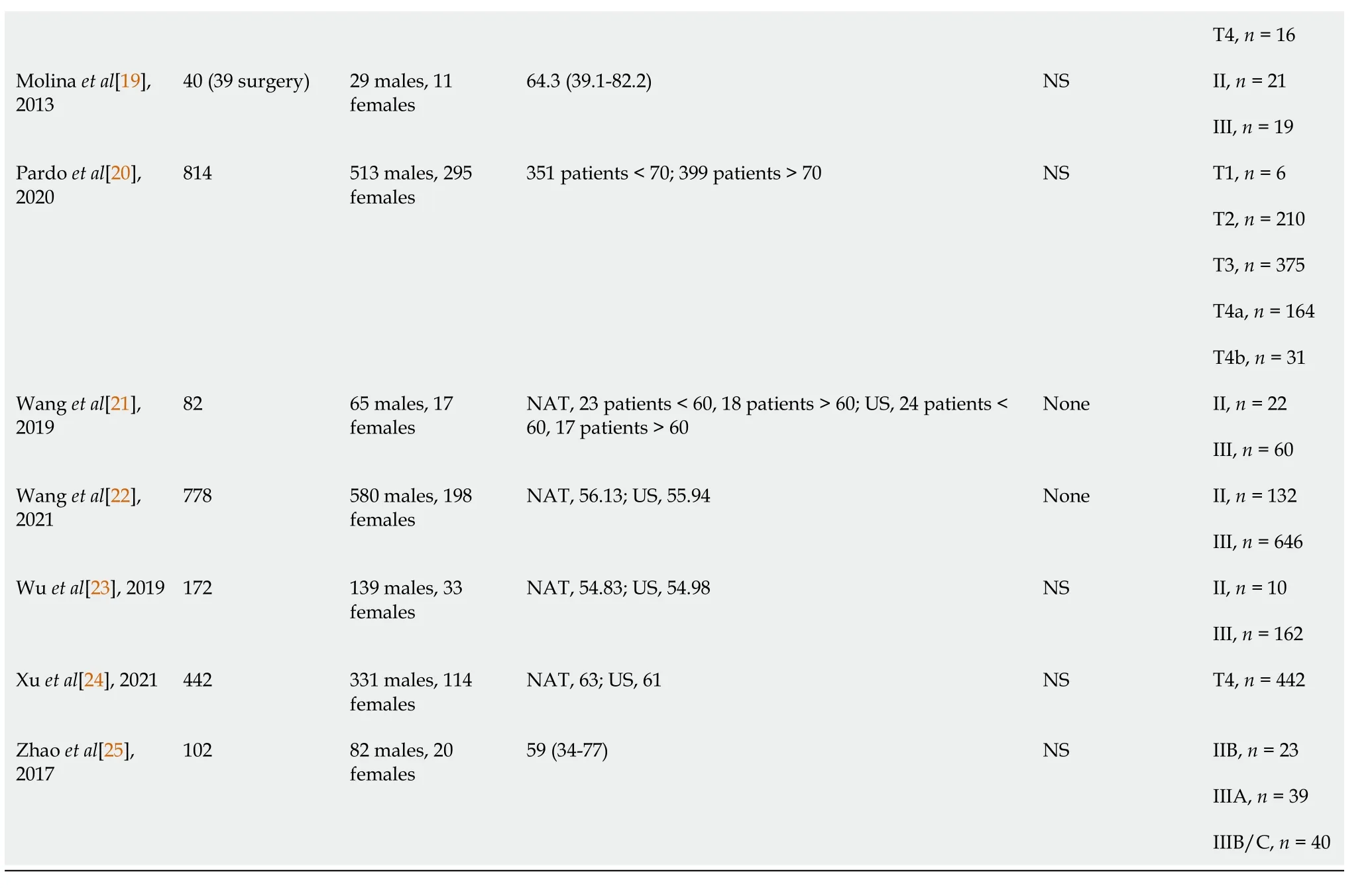
EGJ: Esophagogastric Junction; NAT: Neoadjuvant chemotherapy; US: Upfront surgery; NS: Not stated.
DISCUSSION
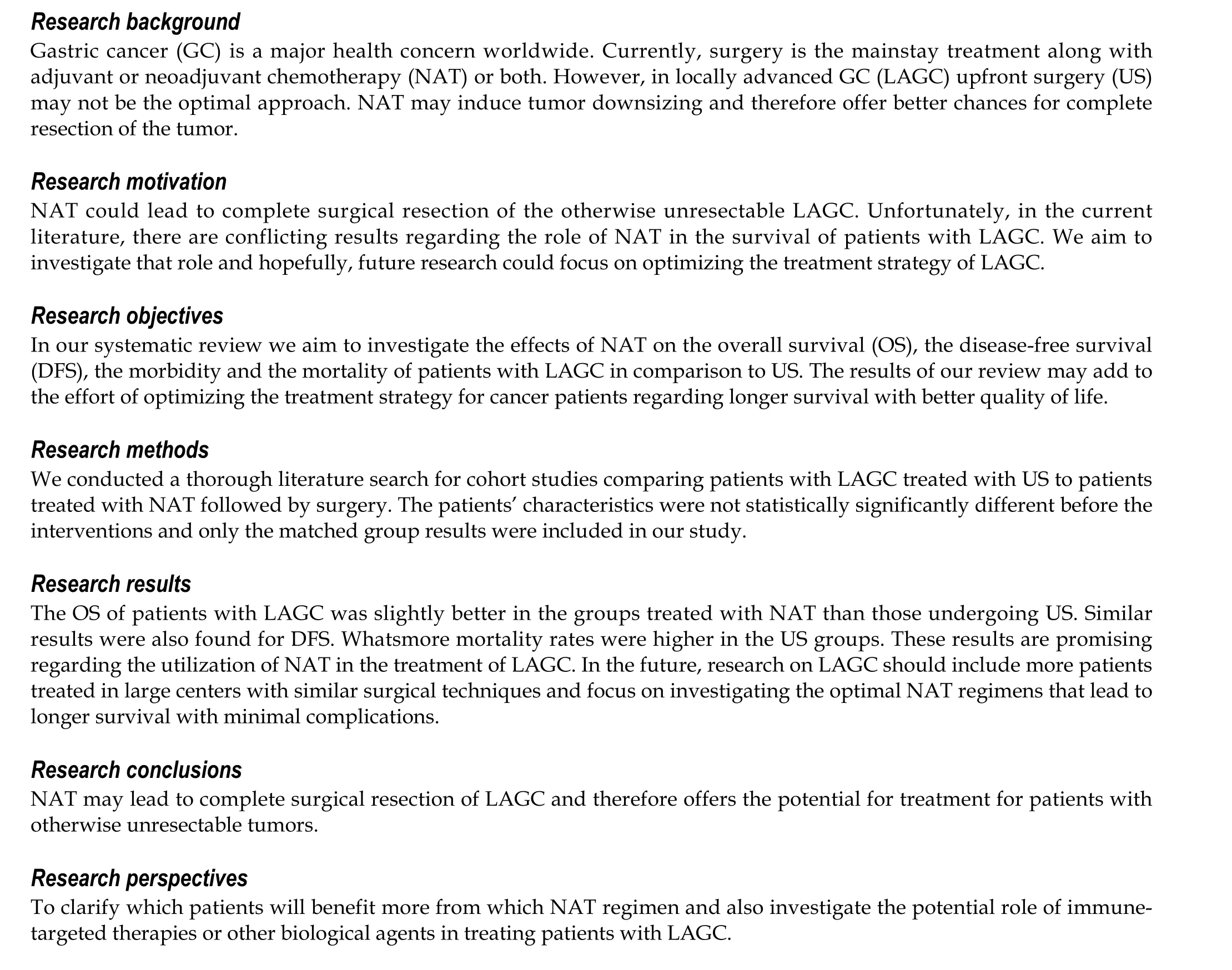
In our systematic review we aimed to investigate the effect of NAT in the survival of patients with LAGC in comparison to US. Most of the studies included in our systematic review showed an OS and DFS benefit in patients treated with NAT.In general, NAT does not increase morbidity and mortality after surgery therefore constitutes a safe treatment regimen for patients with LAGC. Whatsmore, Fenget al[12], Kanget al[15] and Molinaet al[19] demonstrated that patients treated with NAT accomplished significant tumor downstaging which translates to better surgical outcomes. Kanget al[15] also demonstrated that patients with more advanced disease benefited the most from NAT.
However, surgery should not be delayed unnecessarily, as not all patients with LAGC will benefit from perioperative chemotherapy. GC is highly heterogeneous pathologicaly and the response to treatment could vary since different subtypes present with different tumor and clinical characteristics. Zurloet al[1] showed in their retrospective analysis that patients with diffuse type GC had worse OS than those with intestinal type GC when NAT was implemented in their therapeutic approach. Even though histology-driven decisions are appealing, these results need to be confirmed by larger and prospective trials.
There has been a number of trials in Europe such as the MAGIC trial and the FNCLCC/FFCD trial that showed that patients submitted to NAT had longer OS and DFS compared to US patients[4,26]. Moreover, the FNCLCC/FFCD trial showed that the NAT group had higher R0 rates. It is noteworthy that the complication rates remain the same between NAT and US groups which indicates that NAT could be safely administered in clinical practice. NAT followed by surgery and adjuvant chemotherapy is considered the standard of treatment in Europe and the United States.
In the Asian countries the standard of treatment differs from the West. According to the Japanese GC treatment guidelines 2018 (5thedition) NAT should not be offered in LAGC patients. Instead they should undergo US followed by adjuvant chemotherapy[27]. In agreement to these guidelines, the CLASSIC trial with patients from Korea, China and Taiwan demonstrated the necessity of adjuvant chemotherapy due to the significantly higher DFS in adjuvant chemotherapy and surgery group in comparison to surgery only group (P< 0.0001)[6]. On the other hand, the RESOLVE trial in China and the PRODIGY in Korea proved that NAT significantly improves DFS and can be safely administered to patients with LAGC.
In the modern era, the research aims at the molecular level and various biomarkers, prognostic factors and immunotherapeutic agents have been introduced in the management and treatment of LAGC. For instance, the MAGIC and the CLASSIC Trials showed that there is no benefit from chemotherapy in patients with GC and microsatellite instability or mismatch repair protein deficiency[4,6]. A study performed in a Western population suggests additional molecular marker testing as patients showed better prognosis when treated with the anti-programmed cell death protein 1 agent,nivolumab[28]. These results are furtherly supported by a phase 3 trial which showed that the addition of nivolumab in the therapeutic regimen of GC patients provided a statistically significant DFS benefit[29]. Lastly, a phase 2 trial, the FIGHT study, demonstrated that Bemarituzumab, an antibody that selectively binds to fibroblast growth factor receptor 2isoform IIb (FGFR2b) and mediates cytotoxicity, improved the OS, DFS and overall response rate when administered to patients with human epidermal growth factor receptor 2 negative and FGFR2b positive unresectable locally advanced gastric tumor[30].
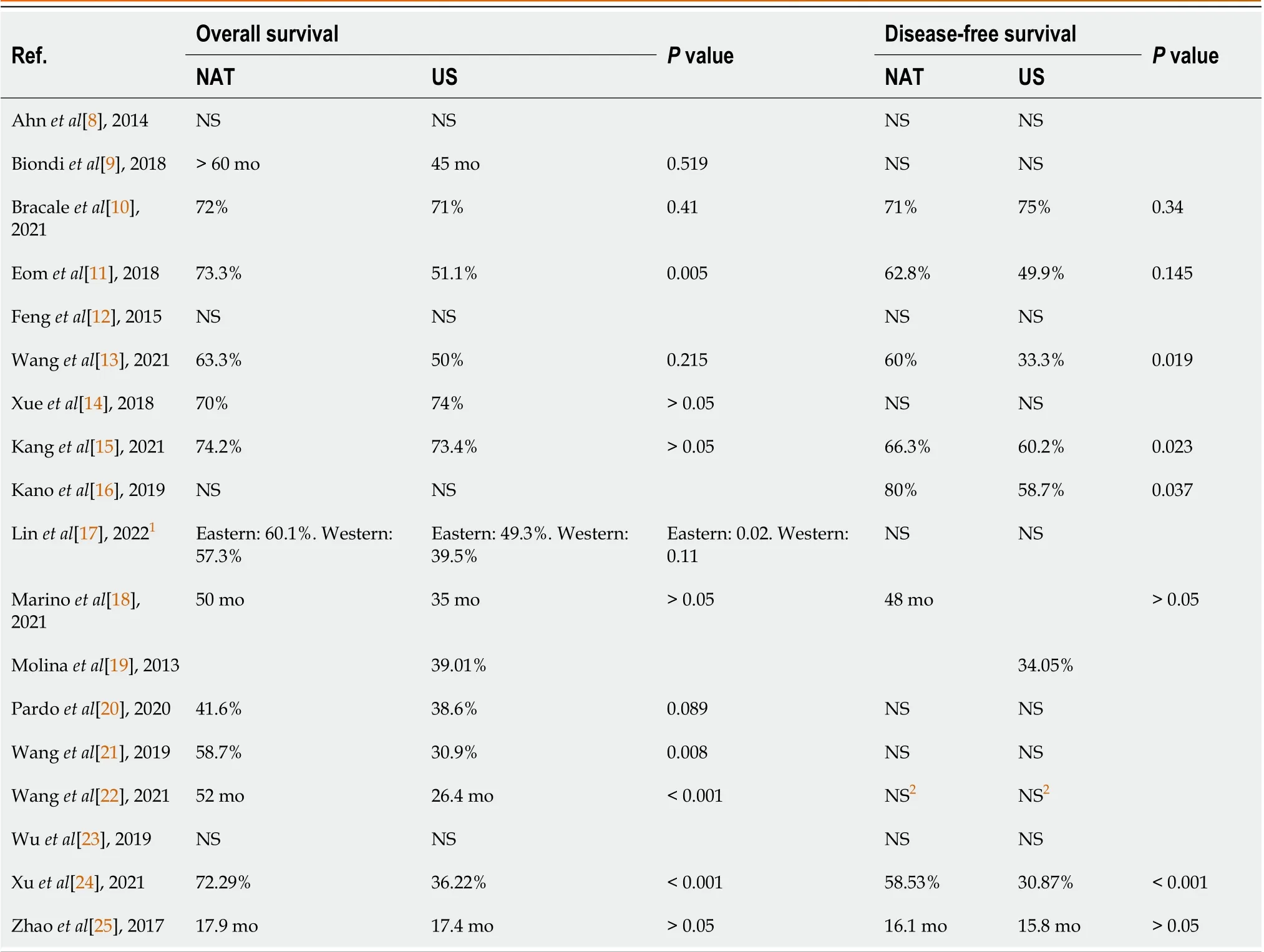
Table 3 Overall survival and disease-free survival of patients after neoadjuvant chemotherapy and surgery versus upfront surgery
Limitations
One limitation of our study is that not all of the patients had the same histological type of GC, which as discussed above may affect the efficacy of the chemotherapy regimen. Also, the chemotherapy regimens were not standardized among the studies. Due to that heterogeneity of data a meta-analysis could not be performed. Furthermore, most of the included studies were retrospective cohort studies, a type of study more frequently susceptible to selection or recall bias. Finally,the operations were not performed by the same surgical teams, and even though we included studies from large centers with high volume of patients the surgical technique and experience may vary.
CONCLUSION
NAT followed by surgery is safe for patients with LAGC and offers potentially better OS and DFS compared to US.However, the optimal treatment regimen for patients with LAGC today is still perplexed, as it is not distinct which patients could benefit the most from NAT. Even though D2 gastrectomy remains the gold standard in patients that can be submitted to surgery, more research is needed to clarify which LAGC patients will benefit more from NAT and immunetargeted therapies or other biological agents. Patients should also be stratified into chemosensitive and chemoresistant groups according to the tumor’s response to initial treatment for more optimal results. To conclude, since each patient with LAGC presents with different clinicopathological features and responds differently to chemotherapy, the treatment plan should be individualized in order to achieve the optimal results.
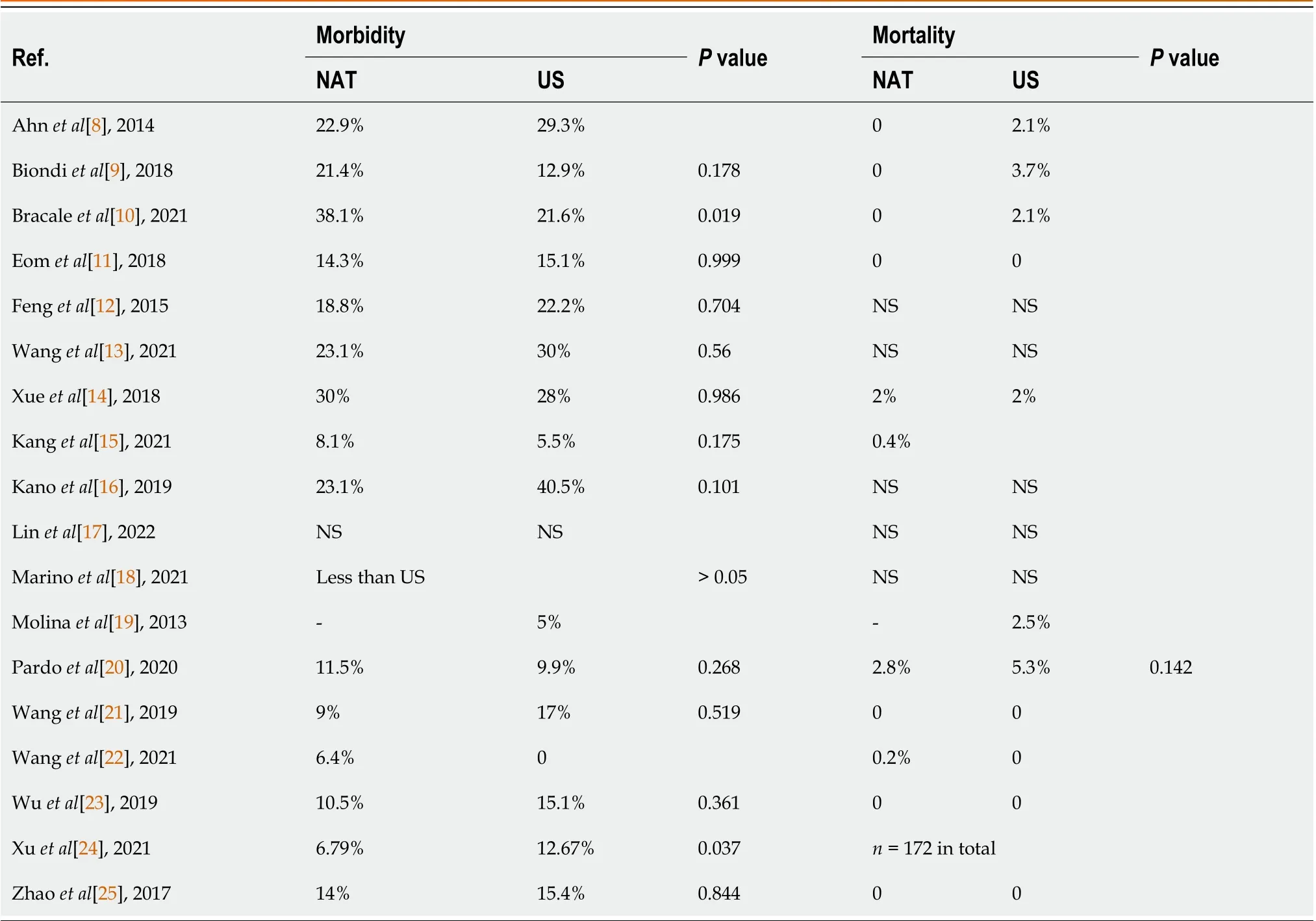
Table 4 Morbidity and mortality of patients after neoadjuvant chemotherapy and surgery versus upfront surgery
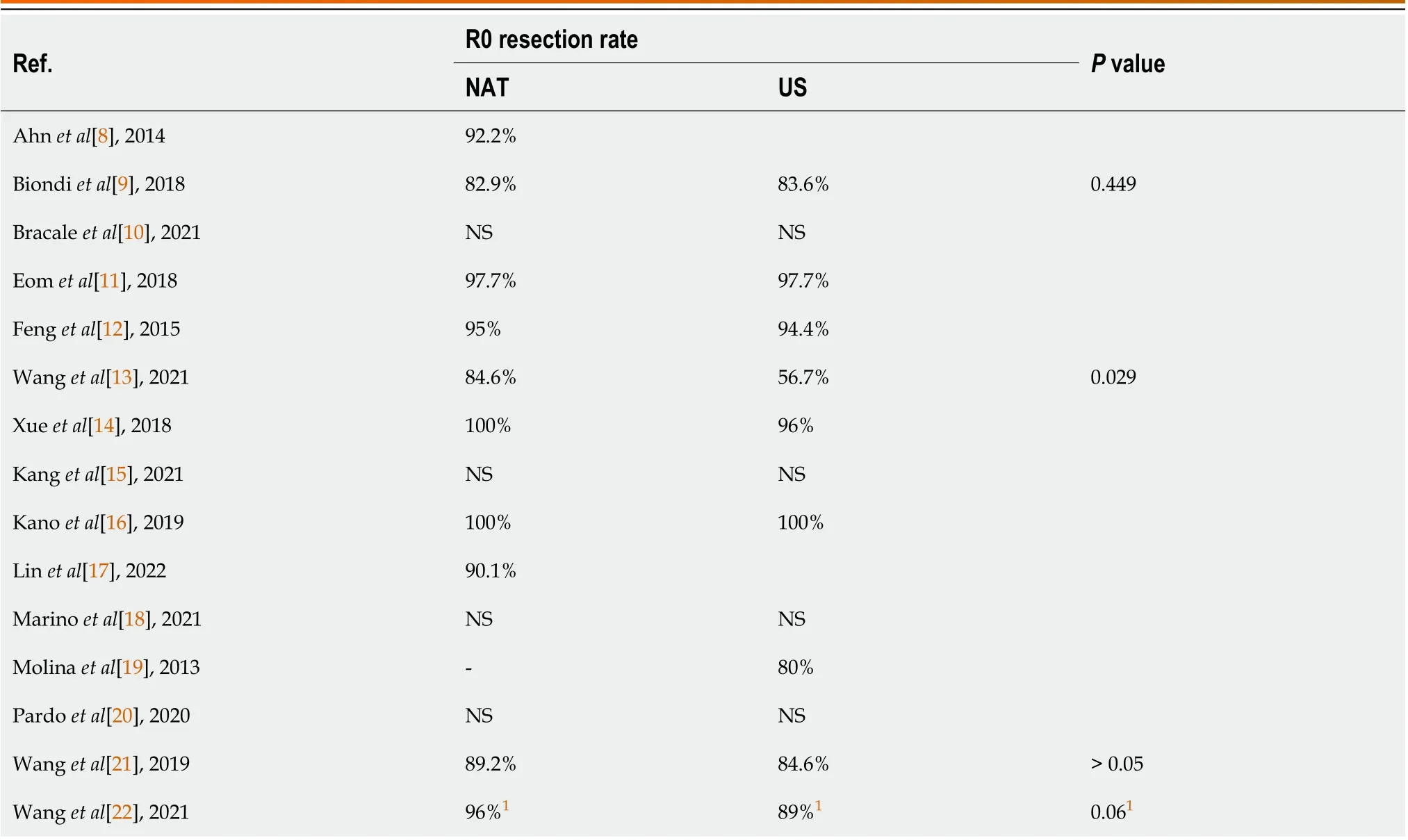
Table 5 R0 resection rate of gastric cancer in patients after neoadjuvant chemotherapy and surgery versus upfront surgery
1Neoadjuvant chemoratdiotherapy versus neoadjuvant chemotherapy (96% vs 89%, P = 0.06).NAT: Neoadjuvant chemotherapy; US: Upfront surgery; NS: Not stated.
ARTICLE HIGHLIGHTS
FOOTNOTES
Author contributions:Fiflis S designed and performed the research and wrote most of the manuscript; Papakonstantinou M performed the research, analyzed the data and wrote part of the results and the discussion; Giakoustidis A resolved conflicts during the article screening, offered guidance and performed manuscript revisions; Christodoulidis G perceived the idea, performed manuscript revisions and assisted as a corresponding author; Louri E wrote part of the discussion and performed manuscript revisions; Papadopoulos VN performed manuscript revisions; Giakoustidis D offered guidance and assisted as a supervising author; and all authors have read and approved the final manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 checklist, and the manuscript was prepared and revised according to the PRISMA 2009 checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Greece
ORCID number:Stylianos Fiflis 0000-0003-0427-6859; Menelaos Papakonstantinou 0000-0001-5030-7009; Alexandros Giakoustidis 0000-0002-3786-4609; Gregory Christodoulidis 0000-0003-3413-0666; Eleni Louri 0000-0003-4790-419X; Vasileios N Papadopoulos 0000-0002-1009-1685;Dimitrios Giakoustidis 0000-0002-6023-4744.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ
 World Journal of Gastrointestinal Surgery2023年8期
World Journal of Gastrointestinal Surgery2023年8期
- World Journal of Gastrointestinal Surgery的其它文章
- Initial suction drainage decreases severe postoperative complications after pancreatic trauma: A cohort study
- Vascular complications of chronic pancreatitis and its management
- Historical changes in surgical strategy and complication management for hepatic cystic echinococcosis
- Post-transplant biliary complications using liver grafts from deceased donors older than 70 years:Retrospective case-control study
- Goldilocks principle of minimally invasive surgery for gastric subepithelial tumors
- Prognosis after splenectomy plus pericardial devascularization vs transjugular intrahepatic portosystemic shunt for esophagogastric variceal bleeding
