A psychometrics evaluation of the Thai version of CaregiverContribution to Self-Care of Chronic Illness Inventory Version 2 in stroke caregivers
Nuntporn Klinjun ,Jom Suwnno ,Knnik Srisomthrong ,Juk Suwnno ,Mtthw Klly
a Faculty of Nursing, Prince of Songkla University, Songkhla, Thailand
b School of Nursing, Walailak University, Nakhon Si Thammarat, Thailand
c The Excellent Center of Community Health Promotion, Walailak University, Thailand
d Stroke Care Center, Hat Yai Hospital, Songkhla, Thailand
e National Centre for Epidemiology and Population Health, Australian National University, Canberra, Australia
Keywords:Caregivers Chronic disease Caregiver contribution Family support Psychometrics Self-care Stroke Thailand
ABSTRACT Objective: To evaluate the psychometric characteristics of the Thai version of Caregiver Contribution to Self-Care (CC-SC) of Chronic Illness Inventory version 2 (CC-SC-CII-v2) in stroke caregivers.Methods: We conducted a multicenter,cross-sectional study following the COSMIN guidelines,evaluating validity and reliability of three separate scales,CC-SC Maintenance,CC-SC Monitoring,and CC-SC Management,as well as overall CC-SC-CII-v2.From September to December 2022,we enrolled 422 stroke caregivers from primary care centers in southern Thailand.Structural validity was assessed through confirmatory factor analysis (CFA),while concurrent validity was evaluated using Pearson’s correlation r coefficients between CC-SC-CII-v2 and the Caregiver Self-Efficacy in Contributing to Patient Self-Care Scale (CSE-CSC).Internal coherence reliability was assessed using Cronbach’s α coefficient,the composite reliability index,and the McDonald’s ω coefficient.Additionally,test-retest reliability was assessed with intraclass correlation coefficients (ICCs).Results: The study included mostly middle-aged women who cared for their parent.CFA supported the two-factor structure of the CC-SC Maintenance and Management scales and the one-factor structure of the CC-SC Monitoring scale.A simultaneous CFA on the combined set of items supported the more general model.The concurrent validity of CC-SC-CII-v2 with CSE-CSC was established (r ranging 0.47-0.65,all P <0.001).Reliability estimates supported adequate Cronbach’s α coefficient (ranging 0.83-0.89),composite reliability (ranging 0.84-0.85),McDonald’s ω coefficients (ranging 0.83-0.85),and ICCs (ranging 0.86-0.90) across the three scales.Conclusions: The Thai CC-SC-CII-v2 demonstrated strong psychometric properties among stroke caregivers.It can be a valuable instrument to investigate the role of caregivers in contributing to stroke patients’ self-care in diverse cultural contexts like Thailand.
What is known?
· The Caregiver Contribution to Self-Care of Chronic Illness Inventory(CC-SC-CII)is a valid and reliable instrument developed in the western context to measure caregiver contribution to the self-care of individuals with non-specific chronic illnesses.
· The instrument has recently been updated to version 2(CC-SCCII-v2) and is now available.
· The CC-SC-CII-v2 has the potential to be used by a range of caregivers of patients with specific conditions like stroke,including in diverse contexts such as Thailand.
What is new?
· We examined psychometric properties of the cross-culturally adapted Thai CC-SC-CII-v2 among caregivers of patients with specific chronic illness such as stroke.
· All three scales(maintenance,monitoring,and management)as well as the overall Thai CC-SC-CII-v2 are valid and reliable.The scale can be used by clinicians and investigators in Thai context,and for specific conditions such as stroke.
1.Introduction
Stroke patients often experience physical,psychosocial,and cognitive limitations that make it difficult for them to perform selfcare at home[1].Self-care is essential for all patients with chronic conditions,including stroke,as it helps maintain stability,control symptoms,prevent conditions from worsening,and promote overall health status [2].In patient-family-centered care,self-care approaches shift from solely patient-focused to caregiver-focused or integrate both patient and caregiver dyads [3].Caregivers play a critical role in providing direct patient care,offering holistic support,and enhancing self-care for stroke patients [1,4].Family caregivers,also known as informal caregivers,provide a vital resource for the patients by offering care modalities that may not be possible for the patients themselves[1,3].
Caregiver contributions to self-care (CC-SC) for patients with chronic illnesses encompass three processes: CC-SC maintenance,CC-SC monitoring,and CC-SC management [3].These processes align with the self-care of patients with chronic illness[2,3].CC-SC maintenance involves assisting the patients or care recipients(CRs)in performing behaviors that maintain physical and emotional stability,such as health promoting behaviors (e.g.,avoiding sickness,physical activity) and illness-related behaviors (e.g.,taking medication as prescribed)used to maintain stability and prevent an exacerbation of the CRs condition [3].CC-SC monitoring involves observing changes in CRs conditions and signs and symptoms.CCSC management involves responding to signs and symptoms of the CRs to control a situation before it worsens and requires urgent or emergency response [3].Caregivers can operate autonomously,such as changing what the CRs eats or drinks to alleviate the symptom,or by consulting a health care provider and talking about the symptoms with the doctor or nurse during the next office visit[3].
In order to effectively evaluate and address the caregiver’s role in supporting self-care,it is essential to have a valid and reliable instrument that captures the multidimensional nature of this construct.One such instrument,the Caregiver Contribution to Self-Care of Chronic Illness Inventory(CC-SC-CII)[5],was developed to measure the level of caregiver involvement in facilitating self-care behaviors.Although the CC-SC-CII has demonstrated promising psychometric properties in different cultures and clinical contexts,it has not been validated in Thai stroke caregivers.Cultural and contextual factors can significantly influence the caregiving experience and the dynamics of caregiver involvement in self-care.Therefore,it is crucial to adapt and validate the CC-SC-CII within the Thai context to ensure its relevance,validity,and reliability in assessing the caregiver’s contribution to self-care among Thai stroke caregivers.
Caregiver competence in contributing to self-care of the patient is a vital aspect of stroke management.Nurses and healthcare teams have developed effective methods to improve caregiver competence,which can result in improved stroke care and better outcomes [6].CC-SC has been proposed as a caregiver-focused outcome that can mediate consequential outcomes for both caregivers and CRs [3].Caregivers who improve their caregiving competence and self-efficacy to meet CR needs have been shown to experience fewer negative impacts,such as depression,anxiety,strain,burden,and burnout [7,8].Improvements in caregiver competence have also been linked to positive impacts on caregiver mental well-being,self-efficacy,health-related quality of life,and overall health status[8,9],as well as positive patient outcomes such as functional independence,health-related quality of life,and overall health status [9].
Recent research on caregiving competence has largely focused on psychoeducational interventions,specific task-oriented approaches,and resource support [9].In Thailand,as in countries worldwide [10,11],stroke is a prevalent and debilitating health condition that demands long-term care.This continuous care for people with chronic conditions typically takes place within the home and involves family members[12-14].The roles of caregivers in contributing to self-care,as well as providing comprehensive support for older adults and individuals with chronic conditions,including stroke,have long been interest in Thailand,particularly within the context of nursing practice and literature [12,13,15,16].However,there has been little emphasis on interventions specifically aimed at enhancing CC-SC,and a comprehensive instrument for measuring CC-SC in stroke patients has not been developed.In diverse family background,healthcare contexts,and country background,caregivers may encounter distinct cultural expectations and norms related to family caregiving [3,17].These cultural factors can influence their roles and responsibilities in supporting self-care for stroke patients.Given the significance of caregiving competence and the influence of CC-SC on both caregiver and patient outcomes,a high-quality instrument is still required to comprehensively identify these outcomes.The valid and reliable instrument can help clinicians and investigators gain a deeper understanding of the unique caregiving dynamics in the Thai context,ultimately improving support and outcomes for both patients and caregivers.
To our knowledge,two measurement forms have been developed to assess CC-SC of patients with chronic illnesses: diseasespecific instruments [18-20] and a generic or none diseasespecific instrument [5].These measures are grounded in the parent theories of Self-Care of Chronic Illness [2] simultaneously with the situation-specific theory of Caregiver Contributions to Heart Failure Self-Care [3].While both measurement forms share basic constructs and items describing caregivers’ behaviors that contribute to self-care,the advantage of the generic measure is its broad applicability.The CC-SC-CII[5]is currently the only available instrument that can assess CC-SC of patients with any chronic condition,regardless of the diagnosis or number of conditions.
The CC-SC-CII [5] measures three related structures of CC-SC,similar to patient self-care: CC-SC Maintenance,CC-SC Monitoring,and CC-SC Management scales.Despite adequate validity,reliability,and cross-cultural appropriateness of the CC-SC-CII among Asian populations,some differences were found in how they responded to the maintenance and management components[21].While potentially suitable for stroke caregivers,the instrument lacks psychometric evaluation in this specific population.The instrument has been currently updated to version 2(CC-SC-CII-v2).Although both the English and Thai translation versions of CC-SCCII-v2 are available (https://self-care-measures.com),its validity and reliability across specific populations remain to be verified.Our research team specifically translated the Thai version and conducted psychometric testing in this study.Likewise,the patient version of self-care,the developers deserve recognition for their comprehensive approach to designing the caregiver version of selfcare contribution tool.Notably,they incorporated three basic caregivers’ contribution behaviors (Sections: A,CC-SC Maintenance;B,CC-SC Monitoring;and C,CC-SC Management),along with the caregiver motivation aspect (Section D: Caregiver Self-Efficacy in Contributing to patient Self-Care [CSE-CSC] scale),into the instrument provided on their website.Based on the theoretical proposed [3] and previous studies [5,21-23],the CSECSC was not regarded as a direct measure of caregiver behaviors in contributing to patients’self-care itself.Instead,it was classified to be a motivating factor that influences caregiver involvement in patients’self-care[3,5,21-23].Consequently,in this study,the CSECSC was not incorporated as a component of CC-SC-CII-v2.It was considered a determinant of caregivers’ contribution to stroke patients’ self-care,consistent with the methodology employed in previous studies [5,21-23].
To determine whether the generic CC-SC-CII-v2 is a useful tool for assessing the contribution of stroke caregivers to patient selfcare,we evaluated the psychometric properties of the crossculturally adapted Thai version of CC-SC-CII-v2.This included evaluating the structural validity (dimensionality),concurrent validity,internal coherence reliability,and test-retest reliability of the three scales and the overall Thai CC-SC-CII-v2.Based on the relevant theory of caregiver contribution to self-care[3],caregiver self-efficacy [22-24] is an important factor that contributes to caregiver competence in supporting patient self-care,and vice versa [3].Then,the CSE-CSC scale [22,23] was used to assess the concurrent validity of the CC-SC-CII-v2.
2.Methods
2.1.Research design
A multicenter,cross-sectional study was conducted from September to December 2022.Our study reports following the COSMIN (COnsensus-based Standards for the Selection of Health Measurement INstruments) Reporting Guideline for studies on measurement properties [25].
2.2.Study setting and participants
Convenience sampling was employed in this study to enroll participants who served as primary caregivers for individuals with stroke.Inclusion criteria only required being an informal caregiver who was a family member or relative of the stroke patient.Professional or paid caregivers were excluded.The primary caregiver was identified as the person recognized by the patient as providing self-care continuity and spending the most time assisting with daily activities [26].We acknowledged that adult family members primarily carry out caregiving for chronically ill people and involve a significant amount of time and effort.Engaging in self-care contribution is an ongoing process that requires frequent attention,often in the patient’s home.Caregivers must also be prepared to handle unforeseen self-care needs that may arise soon after the patient is discharged from the hospital[26,27].We excluded certain caregiver,patient,or caregiving scenarios from our study due to the aforementioned situations.Specifically,the study did not include caregivers under the age of 18,caregivers with less than three months of caregiving experience,or caregiving that took place during hospitalization or within three months of hospital discharge.
To ensure robustness and cross-validation [5],we invited 440 caregivers to participate in our study,which exceeded the minimal required sample size [28] of 200.We rounded up this number to make it comparable to the sample size in the original study[5].We anticipated that the sample size would be close to 400 cases after excluding the outlier cases,which could allow us to capture an appropriate number of caregivers whose CRs had experienced symptoms.Recruitment focused on caregivers of stroke patients registered at 16 primary health care centers,or Health Promotion Hospitals (HPH),in five southern provinces of Thailand.The director of these HPHs compiled a list of patients diagnosed with code I60-I64 in the International Statistical Classification of Diseases and Related Health Problems version 10(ICD-10)and directly contacted their primary caregivers to invite them to participate.For the stability test of the scale,we enrolled 60 stroke caregivers from four HPHs,all of whom were included in the analysis.
2.3.Measures
2.3.1.Translation of instruments
All instruments,the CC-SC-CII-v2 and CSE-CSC scale,were granted permission,approved by the developers,and were made available online (https://self-care-measures.com) prior to the psychometric study.A committee of nine nursing experts evaluated the translational validity of these instruments,yielding an excellent content validity index (CVI) [29].The CVIs for each of the three scales and the overall CC-SC-CII-v2 were 0.99,while the CSE-CSC scale had a CVI of 1.00.
In detail,we conducted the translation and cross-cultural adaptation of both the Thai CC-SC-CII-v2 and the Thai CSE-CSC scale in parallel.The corresponding author (JS) involved in the translation processes,serving as the principal investigator,project manager and synthesizer.We adhered to the ISPOR Task Force for Translation and Cultural Adaptation’s multi-step process [30].The panel of seven experts comprised two forward translators,two back-translators,two synthesizers,and one Thai-English comparator.Six of them hold doctoral degrees in nursing and have extensive experience in the areas of self-care,chronic illnesses,cardiovascular health,and scale development.We used informal words or phrases instead of formal terms for instruction parts of the CC-SC-CII-v2(Section 1:CC-SC Maintenance)and items(items 3,4,and 17).Specific terms or actions were added to make it understandable (Sections 1: CC-SC Maintenance;Section 2: CC-SC Monitoring,and items 4,6,7,8,and 10).Examples of actions or methods of self-care contribution were added because they may be helpful in remembering specific behaviors(items 2,3,4,6,7,9,13,and 14).In addition,we adapted several items (items 3,7,17,and 18) to incorporate language and phrases that convey behaviors understandable to laypersons.For example,we replaced “do physical activity”in item 2 with“exert energy on daily activities or exercise” and described “do something to relieve stress” in item 7 as“mindful relaxation,being aware of stress or overthinking.”Five items required no change (items 1,5,11,12,and 15).
For the CSE-CSC scale,four items required minimal revision(items 1,4,6,and 7).In item 1,the phrase “physical as well as emotional stable” was added to provide clarity regarding the conditions.In item 4,the phrase “physical and emotional” was also added.For item 6,the word “worsen” was included to specify the changes.Lastly,in item 7,the word“important”was replaced with“urgent” to indicate the significance of the event.
Consequently,we obtained the prefinal Thai and English versions of CC-SC-CII-v2 and CSE-CSC scale.During the proofreading step,minor errors were corrected.Subsequently,the final adapted Thai versions of both instruments were approved by all panel experts,while the final back-translated English versions were approved by the original developers.As a result,the final Thai version has been generated and proofread and is now ready for psychometric evaluation.
2.3.2.Caregiver Contribution to Self-Care of Chronic Illness Inventory version 2(CC-SC-CII-v2)
The CC-SC-CII-v2 [5] comprises three fundamental scales: the CC-SC Maintenance scale (items 1-7),the CC-SC Monitoring scale(items 8-12),and the CC-SC Management scale (items 13-19).All items were rated on a 5-point ordinal response scale.The CC-SC Maintenance and CC-SC Monitoring scales asked caregivers to rate how often they recommended certain self-care behaviors for the CRs,with response options ranging from never (score=1) to always (score=5).The CC-SC Management scale assesses caregivers’likelihood of using specific self-care strategies when the CRs experience symptoms,with response options ranging from not likely(score=1)to very likely(score=5).Two items on the CC-SC Management scale had options with scores ranging from 0 to 5.These items were as follow: item 13,with a score of 0 indicating“The person I care for had a symptom,but I did not recognize it as a symptom of his/her health condition”,and a score of 5 indicating“very quickly”;item 19,with a score of 0 indicating “I did not do anything”,and a score of 5 indicating “very sure” [5].
2.3.3.Caregiver Self-Efficacy in Contributing to patient Self-Care(CSE-CSC)scale
The Thai CSE-CSC was used to test the concurrent validity of the Thai CC-SC-CII-v2.Initially,the CSE-CSC scale was part of the CCSC-CII but later separated and developed independently [22,23].The CSE-CSC is a self-rating questionnaire with ten items,rating on a 5-point ordinal scale.It asks caregivers to rate their confidence in their ability to contribute to the self-care of the CRs.Response ranges from “not confident” (score=1) to “very confident”(score=5).
2.3.4.Socio-demographic and illness characteristics
We used a structured questionnaire to collect sociodemographic and illness characteristics data.Caregivers provided all data,including socio-demographic information about themselves and the CRs (e.g.,age,sex,education,marital status,living arrangement,work status,household income,relationship),caregiving situation (e.g.,duration of caregiving,involvement of secondary caregiver).We asked caregivers about other chronic diseases the CRs might have,apart from stroke,and relevant chronic conditions (e.g.,dyslipidemia,visual problems,hearing problems,immobility,wheelchairs,and bedridden).We classified and counted all reported chronic diseases and conditions to determine the total number of comorbidities.
2.4.Data collection
Data was collected using a paper-pencil data collection package form by nurse research assistants from each study setting.All of them received training on the research protocols from the principal investigator.Research assistants informed and obtained consent from participants prior to collecting data.Participants chose the time and place (HPH or home) for face-to-face data collection.Caregivers took 30-45 min to complete all data collection forms on average,including 10-15 min for CC-SC-CII-v2.Caregivers involved in the test-retest reliability completed the CC-SC-CII-v2 twice within 10-14 days apart.
2.5.Ethical considerations
Approval was obtained from the Ethics Board Committee of Walailak University (Approval no.WUEC-22-232-01) prior to data collection.This study adhered to the standards outlined in the Declaration of Helsinki.Participants gave oral and written informed consent,with awareness of their rights,including confidentiality and the ability to withdraw.The analyzed data was anonymized and confidential.
2.6.Data analysis
Descriptive statistics,including frequency (%),mean with standard deviation (Mean±SD),and medians with interquartile range(IQR),were analyzed using SPSS(IBM Statistics 28.0)to summarize the characteristics of the participants and item descriptive.The raw scores of the CC-SC-CII v2 and CSE-CSC were standardized on a scale of 0-100 using the method recommended by the developer[5].Prior to confirmatory factor analysis (CFA),we conducted a Mahalanobis distance test to identify multivariate outliers.A value of less than 0.001 indicated the presence of outliers [31].The normality test was conducted using skewness and kurtosis,with values within the threshold of ±1.00 indicating normality [5].Additionally,the Kolmogorov-Siminov test was performed,with non-significant values(P>0.05)indicating the normal distribution of the data [32].
In order to evaluate the structural validity of the Thai CC-SC-CIIv2,we conducted CFA utilizing AMOS 24.0 to ascertain its dimensional structure.We examined various models based on the originally identified scale [5],including the two-factor CC-SC Maintenance scale,one-factor CC-SC Monitoring scale,two-factor CC-SC Management scale,and simultaneous CC-SC-CII-v2.We selected a parameter estimation method based on the data distribution,and the robust maximum likelihood was recommended for items with non-normally distributed[5].Factor loadings of ≥|0.30|were considered minimally acceptable,and loadings ≥|0.40| were adequate based on the rule of thumb,while loadings ≥|0.70| were considered very good [31].To evaluate the model fit,we used several goodness-of-fit indices,including the Comparative Fit Index(CFI),the Tucker and Lewis Index(TLI),the Root Mean Square Error of Approximation (RMSEA),and the Standardized Root Mean Square Residual(SRMR)[33].The required limited values of each fit indices[5,34] were CFI ≥0.90,TLI ≥0.90,RMSEA ≤0.08,and SRMR≤0.08.CFI and TLI values 0.90-0.95 indicated acceptable fit,and values >0.95 indicated good fit [35].RMSEA values of ≤0.05 indicated a well-fitting model,between 0.05 and 0.08 indicated a moderate fit,and ≥0.10 indicated a poor fit[36].Also,RMSEA with 90% confidence intervals (lower bound ≤0.05 to upper bound≤0.08)establishes a good fit[37].The test of close-fit examines the probability that the approximation error is low with insignificant values (P>0.05) indicating a good fit.SRMR values of ≤0.08 indicated a good fit.Although we reported chi-square statistics,we did not use them to interpret model fit due to their sensitivity to large sample size [5].
Concurrent validity is one among two types of criterion validity[38].Concurrent validity reflects the degree to which the scores from the validated instrument correlate with scores from other instruments assessing the same point of time simultaneously,whereas predictive validity reflects the instrument’s ability to accurately predict future outcomes.In order to establish concurrent validity,we examined the degree to which scores from the CC-SCCII-v2 were correlated with scores from CSE-CSC.We hypothesized that caregiver contribution to self-care would exhibit a positive correlation with their higher self-efficacy [22].We estimated Pearson’srcorrelation coefficients[39]to examine the association between each scale,dimension,and overall CC-SC-CII-v2 scores and the CSE-CSC scores [22].
Internal coherence reliability was estimated following a dimensionality test of the final model [5] using various methods.An internal coherence reliability value of ≥0.70 was considered acceptable for all methods[40].We used the global reliability index for multidimensional scales as well as scales with residual covariances[41].The methods used included the composite reliability index [42] and the McDonald’s ω coefficient [43],which were estimated based on the first-or second-order factor extracted from a final CFA model.For completeness,we also estimated the Cronbach’s α coefficient [44],similar to the original study.Item discrimination was assessed by calculating items-total corrected correlation coefficients,with a threshold of ≥0.30 considered acceptable[45].A higher corrected item-total correlation indicated greater reliability of both the total score and the individual items in capturing the internal structure of the scale [46].Intraclass correlation coefficients (ICCs) were used to estimate test-retest reliability (ICCs),with values of ≥0.70 indicating stability over time[47].
3.Results
Of the eligible caregivers (n=440),six declined to participate due to time constraints,resulting in 434 participants completing the instruments.After excluding 12 multivariate outlier cases as indicated by the Mahalanobis test,there remained a final sample of 422 participants with a minimum of three months of caregiving experience.Among them,359 reported symptomatic occurrences in their CRs.Skewness and kurtosis analysis revealed that multiple items from each scale exhibited non-normal distributions.Also,the Kolmogorov-Siminov resulted in significant deviations from normality for all items (P<0.05).
3.1.Characteristics of participants
Table 1 shows the final sample consisted of 422 caregivers,mostly adults (aged 48.02 ± 12.94,ranging 18-88),women,married or partnered,had completed secondary school or higher,lived with a large family,worked with regular income,and had sufficient or comfortable household income.Most provided care for their parents,lived in the same house with the CRs,and had approximately two secondary caregivers,with a median duration of caregiving of five years.The CRs (Table 2) mainly were older adults(aged 66.77 ± 13.16,ranging 20-102),women,had completed primary school,and lived with a large family.Stroke patients had an average of two chronic diseases and three overall chronic conditions.The most common chronic comorbidities were hypertension,diabetes,walking difficulty,and dyslipidemia.

Table 1 Characteristics of the caregivers (n=422).
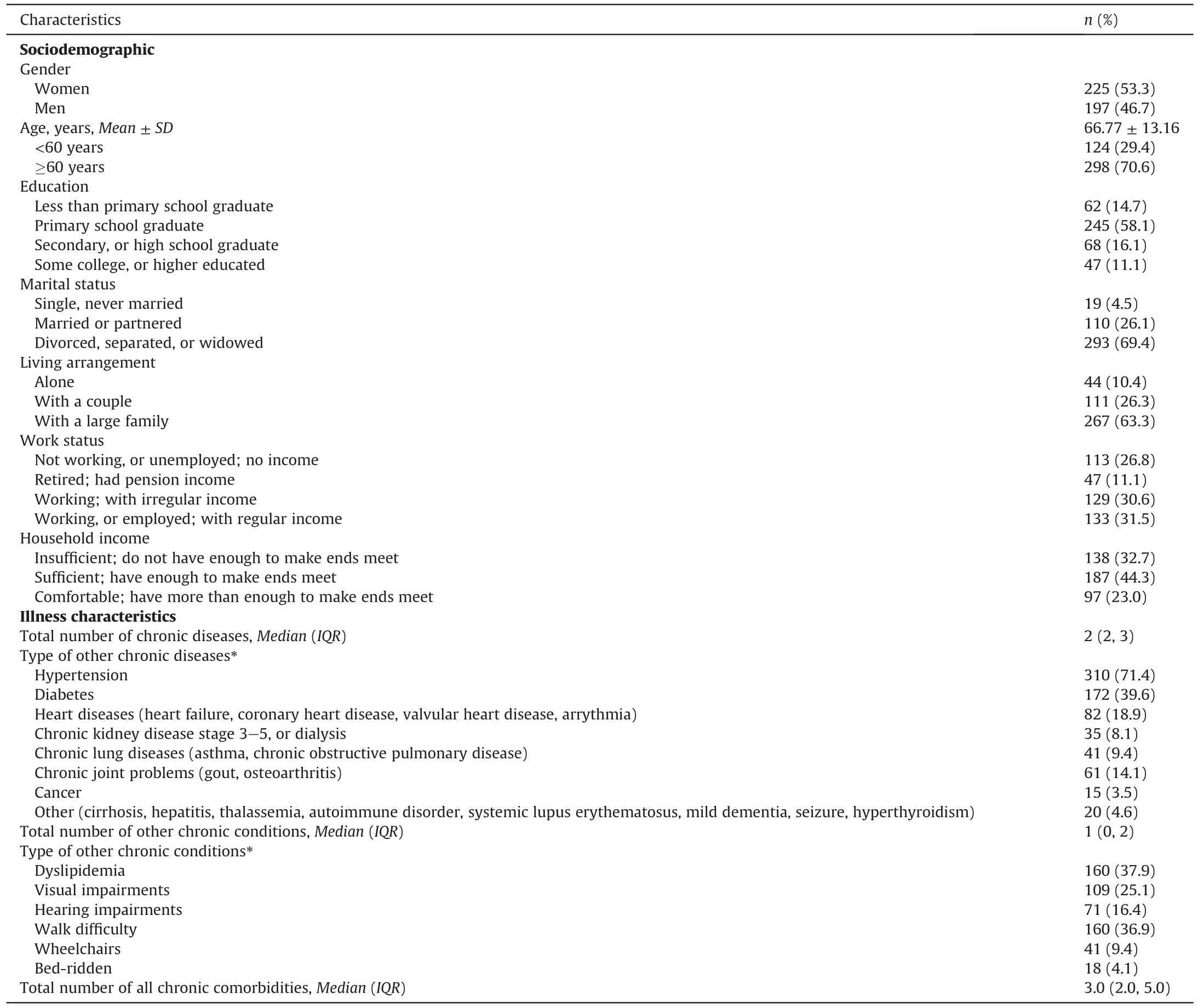
Table 2 Characteristics of the stroke patients (n=422).
3.2.Item descriptive analysis
Table 3 displays the mean scores for the 19 items of the Thai CCSC-CII-v2.Five items (items 1,8,14,16,and 18) achieved the theoretical score[48]of 4,while nine items(items 2,4,5,6,9,10,11,12,and 17) had scores higher than the theoretical score,The remaining five items had moderate scores.Item 5 had the highest score,while item 13 had the lowest score.Two items (items 3 and 18)had a high standard deviation of over 1.00.Several items(items 5,6,9,10,11,12,13,17,18,and 19) were not normally distributed,with skewness or kurtosis indices [5] greater than 1.00.
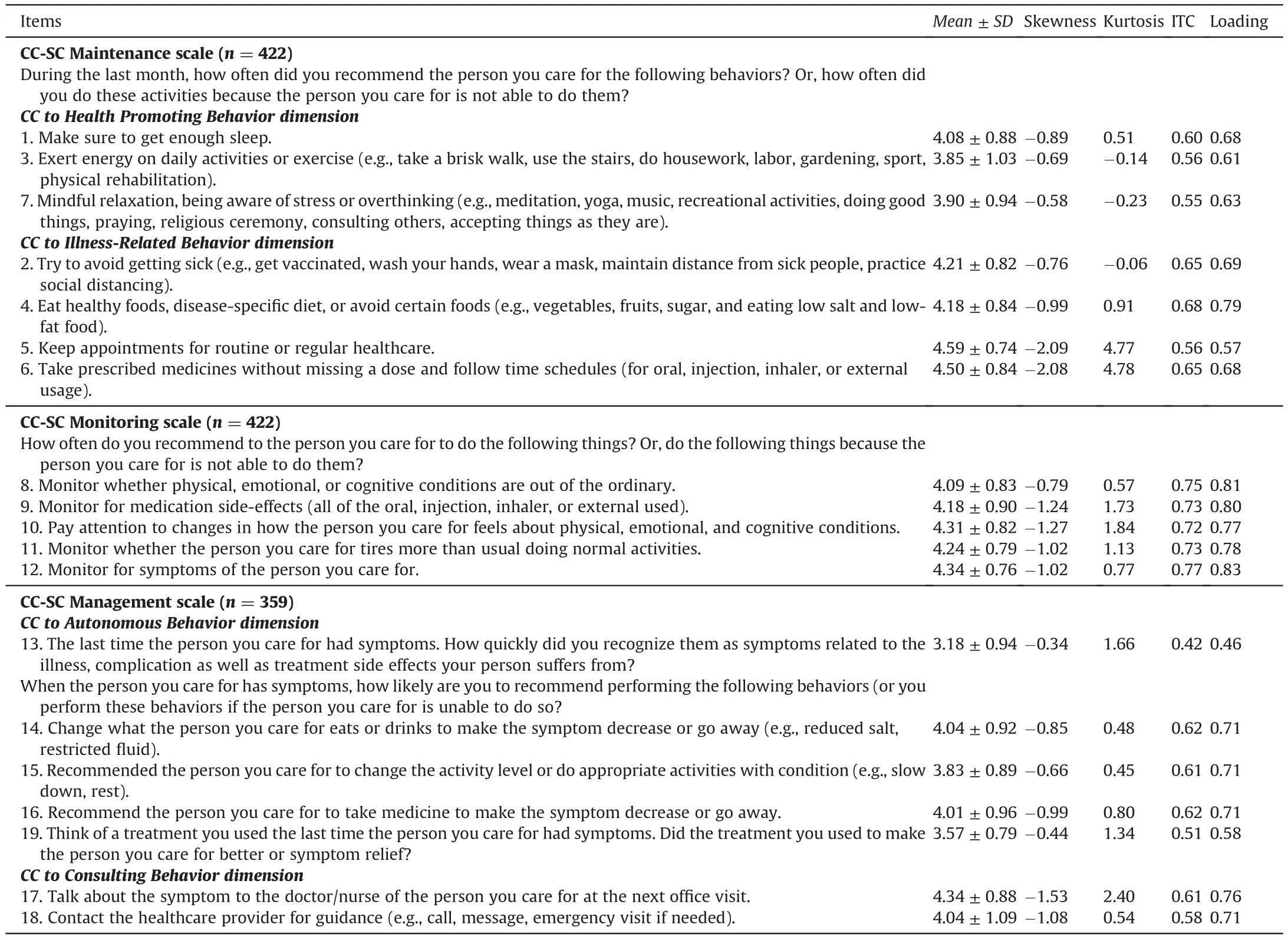
Table 3 Descriptive statistics of the CC-SC-CII-v2 and confirmatory factor analysis of each CC-SC-CII-v2 scale in Thai stroke caregivers.
3.3.Validity
3.3.1.Structural validity(dimensionality)
CC-SC Maintenance scale.We examined a first-order CFA of CCSC Maintenance scale with two dimensions of CC to Health Promoting Behavior(HPB)and CC to Illness-Related Behavior(IRB)[5].The initial analysis showed inadequate goodness of fit indices(Appendix A: Figure A1): χ2[13,n=422]=136.68,P<0.001,CFI=0.88,TLI=0.82,RMSEA=0.15(90%CI 0.12-0.17),P<0.001,SRMR=0.04.Further inspection of the modification indices suggested that the poor fit was caused by covariance between two item pairs (items 2 and 3,and items 5 and 6).The model was then specified to include these residual covariances,resulting in an excellent fit (Appendix A: Figure A2): χ2[11,n=422]=21.21,P=0.031,CFI=0.99,TLI=0.98,RMSEA=0.04(90%CI 0.01-0.07),P=0.523,SRMR=0.02.All factor loadings were significant and greater than 0.40 (ranging 0.57-0.79),which is considered adequate [31].Since the two dimensions were significantly correlated at 0.99,we specified a second-order hierarchical model [5]that resulted in excellent fit indices as well (Appendix A:Figure A3): χ2[11,n=422]=17.17,P=0.103,CFI=0.99,TLI=0.99,RMSEA=0.03(90%CI 0.00-0.06),P=0.71,SRMR=0.01.Unfortunately,the standardized estimates of the CC to Health Promoting Behavior dimension and the standardized error of residuals of this dimension were both over 1.00.Therefore,a multidimensional model of CC-SC Maintenance scale at the second-order factor was not supported [5].
CC-SC Monitoring scale.The one-factor CFA of CC-SC Monitoring scale[5],produced a perfect fit(Appendix B):χ2[5,n=418]=17.47,P=0.004,CFI=0.99,TLI=0.97,RMSEA=0.07(90%CI 0.04-0.11),P=0.105,SRMR=0.01.All factor loadings were significant and greater than 0.70 (ranging 0.77-0.83),which is considered very good[31].
CC-SC Management scale.We examined a first-order CFA of CCSC Management scale with two dimensions of CC to Autonomous Behavior and CC to Consulting Behavior [5].The results showed a good fit(Appendix C:Figure C1):χ2[13,n=359]=54.01,P<0.001,CFI=0.95,TLI=0.93,RMSEA=0.08(90%CI 0.06-0.10),P=0.011,SRMR=0.03.All factor loadings were significant and greater than 0.40 (ranging 0.46-0.76),and were considered adequate [31].We found a significant correlation of 0.87 between the two dimensions,so we specified a second-order hierarchical model [5],which also produced a good fit (Appendix C: Figure C2): χ2[13,n=359]=54.09,P<0.001,CFI=0.92,TLI=0.95,RMSEA=0.08(90% CI 0.06-0.11),P=0.005,SRMR=0.03.Unfortunately,the standardized estimates of the CC to Autonomous Behavior dimension were equal to the standardized error of residuals,indicating that the scale is multidimensional at the primary factor level but unidimensional at the secondary order level [5].
Simultaneous model of CC-SC-CII-v2 in Thai stroke caregivers.Simultaneous CFA was conducted for a model of 19 items and three scales [5].The simple CFA model without allowed covariance residual yielded acceptable fit,as indicated by most goodness-of-fit indices,but not all (Appendix D): χ2[147,n=359]=534.71,P<0.001,CFI=0.90,TLI=0.88,RMSEA=0.07(90%CI 0.07-0.08),P<0.001,SRMR=0.03.However,high residual covariances were observed between three pairs of items(items 5 and 6,3 and 15,and 4 and 14).A trimmed model allowed all three covariances,resulting in improved fit indices,but an overfit with CC to Health Promoting Behavior dimension having standardized estimated value over 1.00.We attempted to address the overfitting issue by re-running the model and included only one pair of items with the highest residual covariances(items 5 and 6).However,this also resulted in an overfit model.We then further specified the model by including two pairs of residual covariances (items 3 and 15,and 4 and 14),which produced the final model with adequate fit indices(Fig.1):χ2[145,n=359]=455.97,P<0.001,CFI=0.92,TLI=0.91,RMSEA=0.07(90%CI 0.06-0.07),P<0.001,SRMR=0.03.All four dimensions in the final model had standardized estimated values lower than 1.00.All factor loadings were significant and greater than 0.40 (ranging 0.48-0.83).
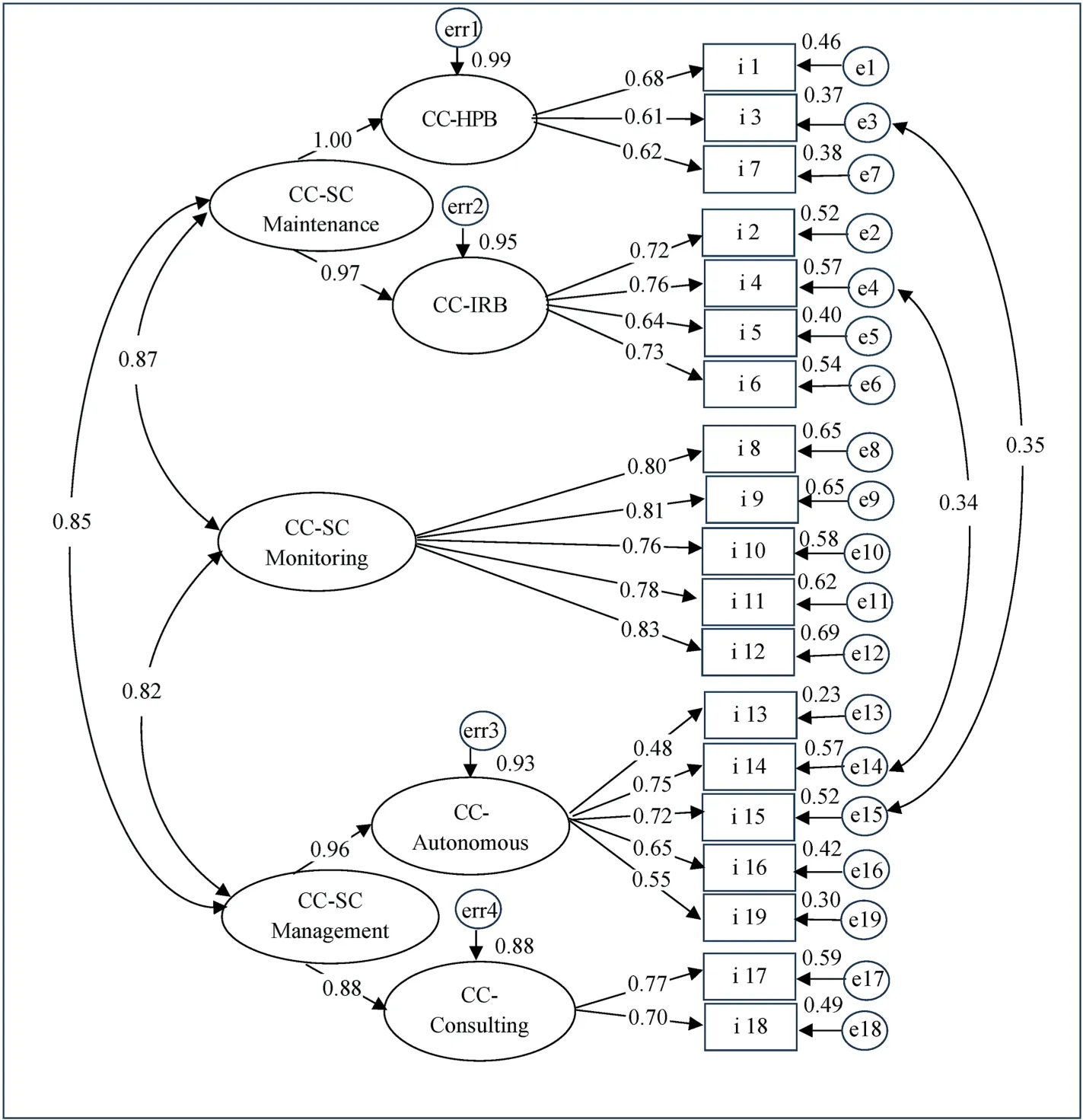
Fig.1.Second-order factor analysis of the final simultaneous model of Caregiver Contribution to Self-Care of Chronic Illness Inventory version 2 in Thai stroke caregivers.Note: CC-SC=Caregiver Contribution to Self-Care.HPB=Health Promoting Behavior dimension.IRB=Illness-Related Behavior dimension.i=item.
3.3.2.Concurrent validity
To assess concurrent validity [38],we calculated Pearson’srcorrelation coefficients [39] between each dimension (Health Promoting Behavior,Illness-Related Behavior,Autonomous Behavior,Consulting Behavior),each scale (CC-SC Maintenance,CC-SC Monitoring,and CC-SC Management),and the total Thai CC-SCCII-v2 with both the Thai CSE-CSC.In Table 4,as expected,all dimensions (coefficientsrranging 0.47-0.63,allP<0.001),scales(coefficientsrranging 0.53-0.63,allP<0.001),and total Thai CCSC-CII-v2(r=0.65,P<0.001)were positively correlated with Thai CSE-CSC.
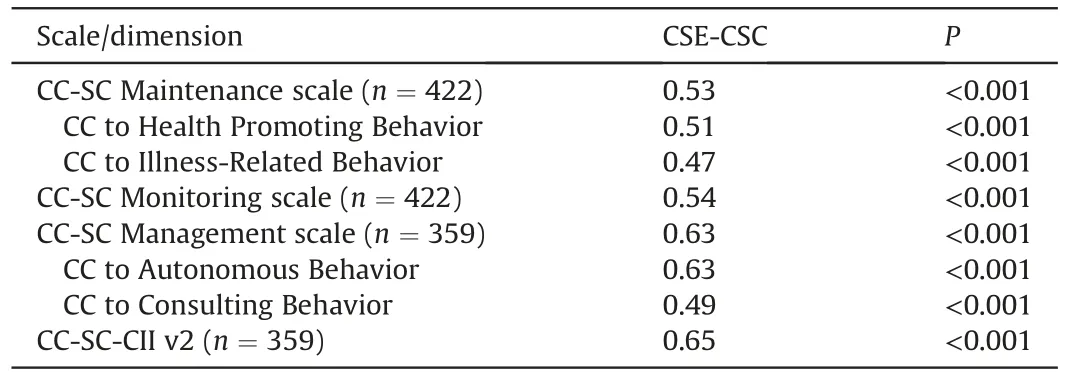
Table 4 Pearson’s correlations coefficient between CC-SC-CII v2 and CSE-CSC scale scores in Thai stroke caregivers.
3.4.Reliability
3.4.1.Internal coherence reliability and item analysis
The reliability of the CC-SC Maintenance scale resulted in Cronbach’s α coefficients of 0.84 and 0.85 standardized (n=422),indicating good internal coherence reliability.The Cronbach’s α coefficient remained high at 0.81-0.83 even if any item was deleted,indicating that no single item significantly impacted overall reliability.All items showed adequate discrimination,with item-total corrected correlation between 0.55 and 0.68 (Table 3),exceeding the acceptable threshold of 0.30.The composite reliability [42] was 0.85 as well as the McDonald’s ω coefficient [43]was consistently good at 0.85.
The reliability of the CC-SC Monitoring scale resulted in Cronbach’s α coefficients of 0.89 and 0.89 standardized (n=422),indicating good internal coherence reliability,with consistent high values of 0.86-0.87 even if any item was deleted,suggesting that no single item significant affected overall reliability.All items presented good discrimination,with item-total corrected exceeding the acceptable threshold of 0.30 and ranging 0.72-0.77(Table 3).
The reliability of the CC-SC Management scale resulted in Cronbach’s α coefficients of 0.82 and 0.83 standardized (n=359),indicating good internal coherence reliability.The Cronbach’s α coefficients remained high at 0.79-0.82 even if any item was deleted,suggesting no significant impact of a single item on the overall reliability.All items presented adequate discrimination with item-total corrected correlation ranging 0.42-0.62 (Table 3),exceeding the acceptable threshold of 0.30.The composite reliability [42] was 0.84,and the McDonald’s ω coefficient [43]consistently showed good reliability at 0.83.
Additionally,we estimated the reliability of the simultaneous CC-SC-CII-v2.Cronbach’s α coefficients of 0.93 and 0.94 standardized(n=359)indicated excellent internal coherence reliability.The α coefficients remained consistently high at 0.92-0.93 even if any item was deleted,indicating that no single item significantly impacted the overall reliability.Item-total corrected correlation between 0.44 and 0.74,demonstrating adequate discrimination,exceeding the acceptable threshold of 0.30.The composite reliability coefficients [42] for CC-SC Maintenance scale,CC-SC Monitoring scale,CC-SC Management scale,and overall CC-SC-CII-v2 were 0.85,0.89,0.84,and 0.95,respectively.Also,the McDonald’s ω coefficient [43] was consistently at 0.93 for the full CC-SC-CII-v2.
3.4.2.Test-retest reliability
The Thai CC-SC-CII-v2 demonstrated good-to-excellent stability reliability[47]in stroke caregivers.The ICCs[47]were 0.89(95%CI 0.85-0.93)for CC-SC Maintenance,0.90(95%CI 0.86-0.93)for CCSC Monitoring,0.86 (95% CI=0.80-0.90) for CC-SC Management,and 0.94 (95% CI 0.91-0.96) for overall instrument.
4.Discussion
This study evaluated the psychometric properties of the crossculturally adapted Thai CC-SC-CII-v2 in stroke caregivers.The structural validity of the scale was consistent with the proposed theory [5],with the CC-SC Maintenance and CC-SC Management scales having two dimensions,while the CC-SC Monitoring scale was unidimensional.The Thai CC-SC-CII-v2 also demonstrated adequate structural validity,concurrent validity,internal coherence reliability,and test-retest reliability.These findings suggest that this generic scale is applicable for use in various context and populations,including stroke caregivers in Thailand.
To our knowledge,this study is the first to examine the psychometric properties of the CC-SC-CII-v2 measure,specifically in the context of stroke caregivers.The findings demonstrated that the instrument is not only structurally valid in this context but also applicable across different caregiver populations and cultural contexts.Although the original instrument was developed in Western settings to measure CC-SC of patients with non-specific chronic conditions [5],our study shows that the CC-SC-CII-v2 is well-suited to the context of stroke caregiving in Thailand.This is particularly relevant given the concomitant common chronic illnesses such as hypertension,diabetes,and hyperlipidemia that require similar self-care support.The CC-SC-CII-v2 can effectively measure the level of self-care contribution by caregivers in stroke patients with multiple chronic conditions [5].Our findings also support the original model that the CC-SC Maintenance and CC-SC Management had characterized as a first-order rather than secondorder hierarchical construct [5].
Thai stroke caregivers described CC-SC Maintenance in a similar way to Italian[5]and Chinese caregivers[21],with three-item CC to Health Promoting Behavior and four-item CC to Illness-Related Behavior dimensions.However,Thai stroke caregivers’ self-care contribution behaviors allocated to each of two dimensions were similar to Italian caregivers [5],but differed from Chinese caregivers[21]who illustrated several behaviors related to CC to Health Promoting Behavior (item 5 “Keep appointments for routine or regular health care” and item 6 “Take prescribed medications without missing a dose”)and CC to Illness-Related Behavior(item 3“Do physical activity”and item 7“Do something to relieve stress”)that depart from the original model [5].The original CC-SC Maintenance scale [5] has also been proposed as multidimensional in disease-specific instruments,such as the Caregiver Contribution to Heart Failure Self-Care Index [26,49],which demonstrated diverse numbers of dimensions and items allocated to each dimension.This reflects how cultural values may influence caregiver contribution to the stroke patient’s daily self-care routine for maintaining health and managing illnesses [3].Overall,the scale’s psychometric properties suggest it is an appropriate tool to evaluate stroke caregivers involving in health maintenance and illness management behaviors of the stroke patients.
Our findings affirmed that the Thai CC-SC Monitoring scale,with five items,is a unidimensional construct with excellent goodnessof-fit indices consistent with the original model [5].Similar caregiver monitoring behaviors were found in previous Italian [5] and Chinese caregivers[21]as well as Thai stroke caregivers,suggesting a clear theoretical construct for this scale.Therefore,the CC-SC Monitoring scale is a suitable tool for addressing stroke caregivers’contribution to monitoring changes in health conditions and symptoms of their CRs.
The seven-item Thai CC-SC Management scale includes two dimensions of CC to Autonomous Behavior and CC to Consulting Behavior,consistent with the original model [5].We found good model fit and clear theoretical construct without the need for modifications or allowing residual covariance among items.Unlike the original model [5] that allowed covariance residuals between specific pairs of management behaviors items,these pairs included item 14,which involved changing the diet or fluids of the CRs to alleviate or eliminate symptoms,and item 15,which focused on recommending appropriate activities of modifying the activity level.Additionally,item 13 assessed the speed at which symptoms related to illness were recognized,and item 19,explored the effectiveness of the treatment in improving the CRs condition or providing symptom relief.The scale’s psychometric properties make it suitable for evaluating stroke caregiver contribution to symptom management for their CRs.
As theorized,the Thai CC-SC-CII-v2 model was found to be a complex construct and fit well with five basic structures [5],as demonstrated by simultaneous CFA.This model was further extended to include two self-care contribution behaviors for health maintenance relevant to symptom management,taking into account theoretical and logical relationships between sets of behaviors.Our study found that the Thai CC-SC-CII-v2 model was better explained by considering the correlations between caregiver contribution to routine physical activity for self-care maintenance and changing the activity level or doing appropriate activities with conditions for self-care management behaviors.Additionally,there was a linkage between caregiver contribution to stroke patient selfcare on eating healthy foods,disease-specific diet or avoiding certain foods,and to change what the patients eats or drinks to make the symptom decrease or go away.The general Thai CC-SCCII-v2 model was found to differ somewhat from the original model,whereas the Italian model was better explained by several residual covariances between items within the same scale [5].However,the 19 items in the general Thai CC-SC-CII-v2 model had adequate factor loadings,indicating that the psychometric properties of the full instrument are suitable for stroke caregiver contributions to comprehensive self-care maintenance,monitoring,and management.
Further,the concurrent validity of the Thai CC-SC-CII-v2 was established in stroke caregivers.As expected,scales,dimensions,and overall CC-SC-CII-v2 were positively correlated with caregiver’s self-efficacy.Higher CSE-CSC scores were associated with higher CC-SC-CII-v2 scores,suggesting that self-efficacy is a powerful determinant of caregiver contribution to self-care in stroke patients,as it is in other chronic conditions [19,49].Studies have linked self-efficacy to caregiver ability to perform specific tasks[50,51] as well as their involvement in comprehensive stroke rehabilitation,caregiver engagement in stroke care,caregiver readiness,caregiving competence,self-care enhancement,and secondary prevention behaviors[1].Caregiver self-efficacy is one of the determinants of caregiver health outcomes.Studies in stroke caregivers have demonstrated a link between lower self-efficacy and caregiver burden [52],while higher self-efficacy is associated with better general health status or quality of life [53].
The Thai CC-SC-CII-v2 was reliable for stroke caregivers across the cultural background of Thailand.The Thai CC-SC-CII-v2,including its three scales,exhibited good-to-excellent internal coherence reliability across different methods,consistent with previous studies’ findings [5,21].In addition,our study provided evidence that the instrument also had good test-retest reliability in this population.
Overall,the Thai CC-SC-CII-v2 exhibits robust psychometric properties,affirming its validity and reliability.This generic instrument holds considerable potential as a predictor of outcomes for both caregivers and CRs in the context of stroke caregiving.
4.1.Strengths and limitations
One of the key strengths of our study is the robust psychometric characteristics of the Thai CC-SC-CII-v2.This generic tool enables us to accurately assess the caregiver contribution to self-care of patients with specific chronic conditions such as stroke.Goodness-offit indices support the structural validity of this theory-derived instrument [3,5],which also has robust internal coherence reliability across three scales and full CC-SC-CII-v2.Additionally,the ICCs suggest that the instrument has good to excellent stability over time.Our study also contributes to existing knowledge by establishing the concurrent validity of the instrument for assessing the determinant factor of self-care contribution among Thai stroke caregivers.The strong correlations between caregiver contribution to self-care and their self-efficacy can support the robust concurrent validity of the Thai CC-SC-CII-v2.Secondly,the participants in this study accurately represented the nature of stroke caregiving.Our study recruited caregivers who provided home-based care throughout the continuum of stroke recovery.This allowed us to accurately reflect the processes of caregiver contribution to selfcare maintenance,monitoring,and management.Additionally,the multicenter approach of including primary healthcare centers and communities allowed us to capture a diverse range of samples and cross-validate our findings.Our study mainly included middle-aged women who were providing care for their parents or spouses after a stroke,which is a typical profile of caregivers in Thailand [13] and globally [14].The findings of our study may be applicable to this population.Finally,the CC-SC-CII-v2 was a feasible instrument,even for low-education caregivers.This is encouraging as it means that the instrument can be used to assess the self-care contribution of stroke caregivers from various backgrounds.
The following limitations have been taken into account in this study.Firstly,although we recruited participants from multiple centers,the use of convenience samplings may have introduced selection bias.Secondly,our study was conducted in the southern region of Thailand,where the culture of self-care contribution may differ from other parts of the country.These may limit the generalizability of our results.Finally,we were unable to address the interobserver reliability of the scale.Despite the training of nurse research assistants to follow data collection protocols and the ability of most participants to complete the instrument on their own,this raises doubts about the consistency and accuracy of the data collected.
4.2.Implication for practice
The non-disease-specific CC-SC-CI-v2 can be used to assess caregiver contribution to the self-care of stroke patients in different linguistic and cultural contexts.This tool can help clinicians tailor interventions to improve the self-care contribution of caregivers for their CRs.Identifying areas where caregivers need support or training can be particularly helpful.The results of our study suggest that caregivers of stroke patients need to improve in several areas of self-care contribution,including helping patients engage in routine physical activity,recognizing symptoms,adjusting activity levels or engaging in appropriate activities based on the condition,and utilizing effective treatment strategies to alleviate symptoms.
It is important to acknowledge caregivers as part of the healthcare team.In our context,they provide home-based care,ensuring continuity of care and serving as a vital resource for patients.Assessing caregiver contribution to patient self-care can promote communication and collaboration between caregivers and healthcare providers,enabling clinicians to comprehend the caregivers’ perspective and identify ways to provide optimal patient care while enhancing caregivers’ competence in self-care involvement.Furthermore,we found a strong and positive correlation between the caregiver’s contribution to the self-care of stroke patients and their self-efficacy in self-care contribution.It is possible that promoting self-efficacy of caregivers can enhance their competence in contributing to self-care for their CRs.This can be achieved through regular assessments of caregiver involvement in CRs’ self-care,highlighting successful actions,and providing constructive feedback on areas for improvement.This can increase their confidence and competence,ultimately resulting in better caregiving outcomes.
Finally,utilizing the CC-SC-CII-v2 can provide a valuable opportunity to improve caregiving outcomes.By improving caregivers’ competence in self-care contribution,other caregiverrelated outcomes such as caregiver burden may also be reduced.Evaluating their levels of self-care contribution can pinpoint areas where they may be struggling and provide specific support to alleviate caregiver burden.Ultimately.Improving family caregiver’s competence in self-care contribution can result in better self-care,optimal general health,and improved health-related quality of life for patients with stroke.
4.3.Implication for research
This was the first study to evaluate psychometric properties of the generic CC-SC-CII-v2 for caregivers of patients with specific conditions like stroke and to test it in a cultural and linguistic context beyond its original language.Further testing is necessary to validate the instrument,and investigators should involve caregivers from various Thai regions to ensure cultural suitability and generalizability.Researchers should investigate the measurement invariance of the CC-SC-CII-v2 among stroke caregivers in other Southeast Asian populations and across different languages and contexts.This can help to ensure that the instrument is measuring the same theoretical construct across different backgrounds and can enhance its validity and applicability in various settings.Extending the study to investigate the predictive validity of the CCSC-CII-v2 on the general health status and health-related quality of life would further establish concurrent validity.Considering various caregiving outcomes,including patients’ self-care,functional recovery,and healthcare utilization,as well as caregivers’ burden,stress,and depression,is crucial.Examining these indicators can provide valuable insight into the overall impact of caregiver contribution to self-care on both patients and caregivers.
To minimize selection bias,future studies should use random sampling methods such as simple random sampling,stratified sampling,or cluster sampling to ensure that all eligible family caregivers have an equal chance of being selected for the sample.This approach can help create a representative sample that reflects the true characteristics of the target stroke family caregivers and minimize bias that could arise from convenience sampling methods.Furthermore,to ensure the consistency of observations made using the Thai version of CC-SC-CII-v2,inter-rater reliability method should be employed to examine the observational reliability of this instrument and provide greater confidence in the accuracy of the data collected.
5.Conclusions
This study confirms the Thai CC-SC-CII-v2 as a reliable tool for measuring Thai caregiver contributions to self-care for stroke patients.Results supported the three basic domains of the general CCSC-CII-v2 model,which consists of caregiver contribution to selfcare maintenance,monitoring and management.The study provided evidence for its validity and reliability.However,further testing is needed to ensure its generalizability,cultural appropriateness,measurement invariance,criterion validity with respect to other determinant factors and caregiving outcomes,as well as observational reliability.The CC-SC-CII-v2 could be useful for assessing caregiver contributions to self-care and tailoring interventions for both caregivers and their CRs.It could be useful for researchers studying caregiver roles in supporting self-care for CRs with other chronic conditions.
Funding
The research was financially supported by Walailak University(grant number: WU-IRG-65-028,Year 2022).
CRediT author contributions
Nuntaporn Klinjun: Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Funding acquisition,Writing-original draft,Writing-review &editing,Projectadministration.Jom Suwanno: Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Funding acquisition,Writing -original draft,Writing -review &editing,Supervision,Project administration.Kannika Srisomthrong:Conceptualization,Methodology,Validation,Investigation,Writing-review &editing,Funding acquisition.Juk Suwanno:Conceptualization,Methodology,Validation,Investigation,Writing -review &editing,Funding acquisition.Matthew Kelly:Conceptualization,Methodology,Validation,Writing -review &editing,Funding acquisition.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research,authorship,and/or publication of this article.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical approval
Approval was obtained from the Ethics Board Committee of Walailak University (Approval no.WUEC-22-232-01) prior to data collection.This study adhered to the standards outlined in the Declaration of Helsinki.All the participants provided oral and written informed consent,and were aware of their rights and responsibilities.Right to withdraw and confidentiality of personal data were ensured.The analyzed data were anonymized and treated as strictly confidential.
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work,the author(s)used ChatGPT in order to improve language.After using this tool/service,the author(s) reviewed and edited the content as needed and take(s)full responsibility for the content of the publication.
Acknowledgements
We express our deep gratitude to Barbara Riegel,PhD,RN,FAAN,FAHA,University of Pennsylvania,School of Nursing,USA,and Ercole Vellone,PhD,RN,FAAN,FESC,University of Rome “Tor Vergata”,Department of Biomedicine and Prevention,Faculty of Medicine,Rome,Italy for their approval of the instruments,and for being available and supportive.We would like to express our sincere appreciation for the valuable contribution of the nurses who served as research assistants for their actively participated in the data collection process.Finally,we express our thank to Marzukee Mayeng,MSc,a biostatistician at Department of Epidemiology,Faculty of Medicine,Prince of Songkla University,for his invaluable statistical consultation and review.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.09.021.
 International Journal of Nursing Sciences2023年4期
International Journal of Nursing Sciences2023年4期
- International Journal of Nursing Sciences的其它文章
- Relationship between nurses’ perception of professional shared governance and their career motivation: A cross-sectional study
- 《国际护理科学(英文)》2024年征稿
- The associations among nurse work engagement,job satisfaction,quality of care,and intent to leave: A national survey in the United States
- The implementation and impacts of national standards forcomprehensive care in acute care hospitals: An integrative review
- Nurse-coordinated home-based cardiac rehabilitation for patients with heart failure: A scoping review
- Effectiveness of a family-based program for post-stroke patients and families: A cluster randomized controlled trial
