Impacts of fighting against COVID-19 on critical care nurses’ psychological and physical health: a literature review
Arisara Malairojsiri
Fundamental Nursing Department, Academic Affairs Division, The Royal Thai Army Nursing College, Ratchathewi, Bangkok, 10400, Thailand
Abstract: Objective:To provide insight into the effects of the coronavirus disease (COVID-19) pandemic on the physical and psychological health of critical care nurses in adult units.Methods:A systematic search through the CINAHL,MEDLINE,and EMbase databases were performed.Studies that addressed “critical care nurses,” “COVID-19,” “physical effect,” and “psychological effect” from different perspectives were reviewed.Results:A total of 42 articles were reviewed based on 2 aspects: critical care nurses’ psychological and physical health.Negative emotions were the most common conditions: fear,anxiety,depression,and post-traumatic stress disorder (PTSD).Burnout,falling ill and having thoughts of self-harm,fatigue,physical burden,sleeping disorders,and chronic work overload also adversely affected the nurses’ health.The nurses’ health deteriorated because of the changes in the unfamiliar working environment and processes,colossal workload and chronic exhaustion,worries about themselves and their families,social response,and witnessing the death toll.Conclusions:Critical care nurses experienced adverse effects of the institutional reaction,social response,and individuals’ reply to the COVID-19 pandemic upon their psychological and physical health.Supporting services and preparation for other unprecedented situations should be sustainably available.
Keywords: critical care nurses • ICU nurses • COVID-19 • physical health • physical wellbeing • psychological health • psychological wellbeing
1.Introduction
The coronavirus disease of 2019 (COVID-19) has caused the deterioration of healthcare facilities and global health since early December 2019.1As of 3 April 2022,more than 6 million deaths had been recorded throughout the 2 consecutive years,while there were more than 1–2 million daily new cases confirmed with COVID-19.2The COVID-19 disease commonly damages the respiratory system,resulting in a range of effects from no physical signs and symptoms to severe respiratory conditions or death.3This communicable disease is still disrupting the world healthcare system and causing a heavy toll,because it has not been eradicated promptly.
In the healthcare system,the COVID-19 pandemic is the greatest threat to healthcare workers who have continued to provide care for patients.4The professionals’ welfare has been declining progressively for a few years.There are enormous difficulties,namely exhaustion,personal risk of infection,fear of transmission to family members,and illness or the loss of surrounding people.However,the healthcare workers continue to provide care for patients.Moreover,various sources of anxiety and stress also disrupt professionals’ ability to cope,namely extended shifts,unprecedented population restrictions,and personal isolation.5A national survey among the United States healthcare workers reported that 61% were afraid of exposure or transmission,38% were anxious or depressed,43%suffered from work overload,and 49% were suffering burnout.6Another cross-sectional study was performed at a single center in China with 2299 participants.The frontline healthcare workers,who worked in respiratory departments,emergency departments (EDs),intensive care units (ICUs),and departments of infectious disease were twice as likely to suffer anxiety and depression as non-healthcare workers.7Meanwhile,some studies that investigated on critical care nurses and physical health are separately regarded.
It is necessary to gather comprehensive data on the effects of COVID-19 on critical care nurses’ psychological and physiological health,because poor physical or psychological health could also affect everyone concerned.Moreover,psychological symptoms can interfere with daily activities,namely relationships,daily life,and work performance,8and therefore these symptoms might affect the performance of their duties.It is a worrisome problem,particularly among critical care nurses responsible for caring for severely ill patients with COVID-19,along with their families and themselves during the unusual situation.Consequently,this study aims to provide insights into the effects of the COVID-19 pandemic on both the physical and psychological health of critical care nurses,particular in adult units,by reviewing the available papers.
2.Methods
2.1.Data sources and search strategy
The available relevant studies were sought through 3 databases: CINAHL,MEDLINE,and EMbase.Both MEDLINE and EMbase were considered as the most significant sources for identifying trials and critical international healthcare databases.9Similarly,CINAHL is associated with the literature on nursing and allied health,including nursing journals and publications from the National League for Nursing and the American Nurses Association.10Moreover,these databases were relevant to the chosen topic and easily accessible.The Population,Exposure and Outcome (PEO) framework was also applied to form the research question and develop a strategy for searching the literature through these databases,11based on “critical care nurses,”“COVID-19,” “physical effect,” and “psychological effect.” The search terms are shown in detail are shown in Table 1.I also applied EndNote X9 to assist me in organizing texts and references.
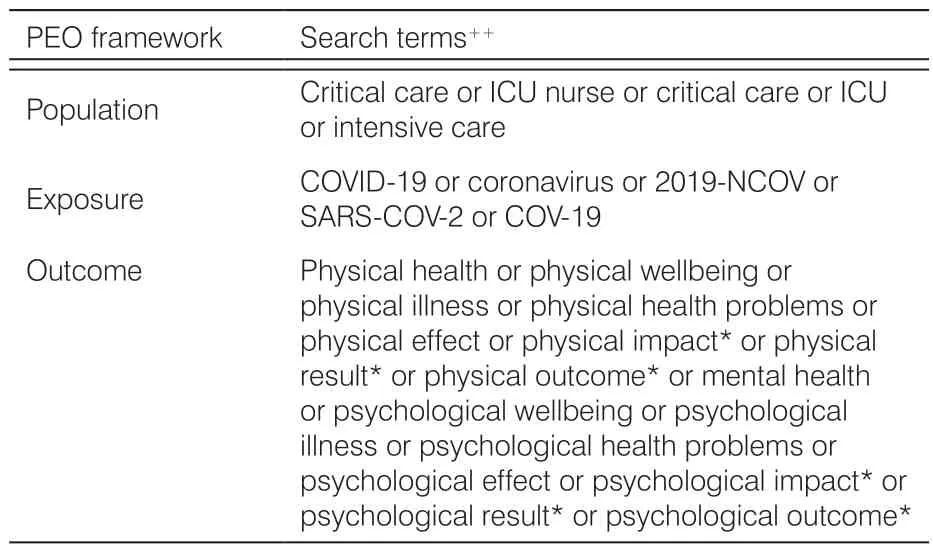
Table 1.Search terms based on PEO framework.
2.1.1. Inclusion criteria
(1) Quantitative analysis,qualitative analysis,and mixed methods research to examine the effects of COVID-19 on the physical or psychological wellbeing of critical care nurses;(2) critical care nurses in adult units;(3)no geographical restrictions to evaluate the impacts of COVID-19 on critical care nurses in different countries;(4) studies published in English;and (5) published articles from 2019 to 1 May 2022.
2.1.2. Exclusion criteria
(1) Critical care nurses in pediatric units or without care for patients with COVID-19;(2) studies published in other languages;and (3) correspondences,editorial,and review articles.
2.2.Screening and selection of study
Titles and abstracts were screened before reviewing full texts to identify the ineligible texts based on the inclusion and exclusion criteria.Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)flowchart was used to encourage transparent and systematic literature search processes12and then independently screened each title and abstract before reviewing full texts to identify the eligible texts based on the predefined criteria.
2.3.Data extraction
Information was extracted from the eligible texts based on the 2 specified domains: the psychological and physical health of critical care nurses.The information on study characteristics was also extracted.
2.4.Quality appraisal
A supplementary review is not essential to assess the quality of the included evidence.13The review included all studies that satisfied the inclusion criteria,and regardless of the quality of the research conducted,to consider all impacts of the COVID-19 pandemic on critical care nurses’ psychological and physical health.
3.Results
The search terms were run through the selected databases,Figure 1 shows the process of study selection based on the predefined inclusion and exclusion criteria.A total of 161 records were scanned and their title and abstract before screening the full text.Finally,42 eligible studies were obtained.
Figure 1.PRISMA flow diagram of study selection.COVID-19,coronavirus disease;PRISMA,Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
3.1.Psychological effects
3.1.1. Negative emotional states
Most published papers reported that the nurses caring for patients with COVID-19 experienced negative emotional states: fear,anxiety,anger,insecurity,regret,grief,loneliness,and other feelings.Critical care nurses typically witness not only life-and-death situations in ICUs,but also the manner of providing care with restrictions and difficulties due to COVID-19.From the included studies,the negative emotional states were commonly reported as anxiety,stress,depression,and fear.14–20Furthermore,the COVID-19 crisis and its impacts on patients’ lives,colleagues,and families predisposed nursing staff to posttraumatic stress disorder (PTSD),particularly in nurses who had no experience in critical care units.21–24Changes in job tasks,nursing approaches,and caring processes can possibly trigger mental illness and persistent psychological problems in nursing staff.Many papers that examined the effects of the COVID-19 pandemic on the psychological wellbeing of critical care staff reported that female gender and nursing roles in critical care were frequently associated with a greater risk of negative emotions rather than male gender,physicians,and ward nurses.14,25–30
Additionally,the use and shortage of personal protective equipment (PPE) for caring for patients with COVID-19 was an unavoidable issue.The problem of PPE also induced negative emotions.Although PPE could protect healthcare staff from direct contact with those patients,it increased the burden and difficulties of providing nursing care and resulted in working exhaustion.Additionally,reusing PPE and the appropriate use and availability of PPE were reported as considerable concerns for healthcare staff.15,31,32If PPE was inappropriately used it would be worthless as PPE,and affected the mental health when nurses came into contact with patients with COVID-19 despite wearing PPE.33Consequently,sufficient knowledge for utilizing PPE could be essential to relieve stress.
Furthermore,social effects and the families of nursing staff were also significant in dealing with this crisis;however,they seemed to be a catalyst for mental illness.Most studies showed that nursing staff underwent terrible experiences due to the isolation of colleagues,social stigma,bereavement,and inability to take care of their families.The mental states of nursing staff were affected by the health of their families and others,changes in work,and concerns about isolation.The survey revealed that among nurses who worked in the COVID-19 ICUs,there were high levels of depression and anxiety.30,34Meanwhile,stigma from the community was significantly associated with emotional distress or burnout among 1651 respondents with almost 50% of the participants being critical care nurses.32Additionally,the relevant determinants of the symptoms of mental illness were revealed,including fear of infection,struggling against negative emotions,incapacity to rest,inability to care for family or bringing the virus home,undergoing hasty end-of-life care,and remorse concerning the limitations on visitation.35
Another cross-sectional survey after the 1-year COVID-19 outbreak reported that working in ICUs was significantly associated with sustained psychological problems,including emotional exhaustion and a cynical attitude towards work.18Moreover,the psychological distress of critical care nurses might be induced by continuously witnessing the death toll.Conversely,the interviews with 15 ICU nurses reported positive emotions,namely confidence,job pride,and inner satisfaction.36However,this seemed to be less than the negative emotions reported by most of the existing studies.
3.1.2. Burnout
As Dall’Ora et al.37found,negative occupational qualities,namely,high workload,low staffing levels,lengthy shifts,and low control,were associated with nurses’burnout.The potential effects were severe for both nursing staff and patients.In all,91 studies evidenced these relations between emotional exhaustion and the nursing field.Even without the conditions of the COVID-19 pandemic,nursing staff were at high risk of burnout due to their regular working conditions.
The COVID-19 pandemic immediately and enormously changed the typical approach to caring for patients and increased the strain on the frontline workers.Women nurses who worked in ICUs involving patients with COVID-19 had a significant prevalence and risk of emotional burnout syndrome.35,38,39Similarly,Chen et al.40reported that among 12,596 nursing participants who were women,and worked in ICUs with COVID-19 patients,there was a greater risk of burnout.This is because COVID-19 was a significant cause of changes in the work environment,tasks,and duties,namely,different working areas,locations,and roles.14,26Additionally,insufficient PPE access,stigma from the community,and poor communication with supervisors were related to burnout.32Thus,critical care nurses thought of undertaking a career change or developed a strong desire to leave healthcare.41Nevertheless,before leaving the nursing profession,most critical care nurses underwent negative feelings and undesirable consequences from the spread of this terrible disease,leading to becoming patients themselves.
3.1.3. Falling ill or making the decision to self-harm
The high levels of mental health disorders were associated with critical care professionals during the first wave of the COVID-19 pandemic.Furthermore,among 845(70%) responders,66% were nursing staff.Around 7.7%of those responders took a psychotropic drug daily.35Consequently,nurses not only have responsibility for caring for severely ill patients,but critical care nurses also had to take care of themselves with changes in mental health and wellbeing.According to the data on the difficulties of dealing with the COVID-19 pandemic,709 critical care staff included 344 (49%) nursing staff,and 13% of the staff often thought of hurting themselves in the past 2 weeks or being off due to death.When examined by role,these thoughts arise in a greater proportion of nurses with 19% compared with just 10% in other clinical staff or 8% in physicians.Meanwhile,7%of 709 ICU staff had problems with drinking.29Similarly,another study reported that there was an increase in alcohol and tobacco consumption among ICU caregivers,representing 49 (24%) professionals and 46 (22%)professionals,respectively.23It is a significant issue that must be considered before critical care nurses endanger their lives,self-harm,or take their own life due to shouldering the burden of responsibility.Apart from mental health,physical wellbeing is associated with stress that could influence the quality of life,particularly via the impacts of the COVID-19 pandemic,42as shown in Figure 2.
Figure 2.The effects of COVID-19 on critical care nurses.COVID-19,coronavirus disease.
3.2.Physical effects
3.2.1. Fatigue or physical burden
Critical care nurses typically carry a significant responsibility to care for severely ill patients.During the threat of COVID-19,most patients required immediate care and had severe worsening within a short period of time.Thus,most patients with COVID-19 were admitted to ICUs,exceeding the ICU availability.
Based on the study of Peñacoba et al.42the impacts of COVID-19 were associated with physical health according to the questionnaires comprising 8 domains:physical functioning,physical role limitations,bodily pain,general health,vitality (energy and fatigue),social functioning,emotional role limitations,and mental health.The results showed that critical care nurses suffered from extreme physical and mental exhaustion during the unprecedented situation.The nurses also perceived high levels of stress from this situation.They have also seen their work demands increase.Therefore,stress was associated with physical health components involving quality of life through self-efficacy and resilience.42Self-regulation and external support were also associated with the enormous strain from the COVID-19 pandemic.43Additionally,both pandemic-related and psychological variables were associated with reduced wellbeing and lower resilience levels among 1305 frontline participants from the United Kingdom and the Republic of Ireland.Thus,it is crucial that critical care nurses can serve the ongoing and acute care requirements of their communities in a state of wellbeing,while they recover from and absorb the impact of the unexpected event.44Nevertheless,this unavoidable hardship could overwhelm critical care nurses and lead them to lose their physical wellbeing.
3.2.2. Sleeping disorders or insomnia
A study conducted among healthcare workers reported high insomnia in women,particularly those in nursing roles,and ICU staff.30Another cross-sectional survey among 441 professionals also reported similar results.The healthcare workers who were directly involved in caring for patients with COVID-19 in Eds,infectious wards,and ICUs were at high risk of sleep disorders.27As Saracoglu et al.45concluded the prevalence of sleep disturbance was greater in ICU professionals.Meanwhile,critical care nurses were the group with the highest deterioration in sleep quality.A feeling of tiredness is a consequence of inadequate sleep quality.These sleeping disorders could contribute to shortcomings in daily functioning,thinking,and physical health,as well as symptoms of underlying psychological health issues.Additionally,there might be repercussions from the sleeping disturbance upon patient care.It is important to raise awareness of the need for sufficient sleep and to provide a solution for improved quality of sleep for those ICU nurses.
Sleep,food,and water are the basic physical necessities of living according to Maslow’s hierarchy of needs,as shown in Figure 3.Hence,when some of the most vital needs are unmet demands,physical or psychological health could be adversely affected.To illustrate,many hours of continuous work with no guarantee of relaxation or satisfaction of daily needs,could decrease critical care nurses’ psychological and physical wellbeing.These supporting factors are found in the bottom levels of the pyramid and have affected many people during the COVID-19 pandemic.This shift in primary necessities has resulted in a significant change in individual emotional states and a trend toward negative feelings.46Therefore,they ought to be promised a place to satisfy their daily needs and relax independently.47Furthermore,psychological disorders could result from sleep deprivation,losing work–life balance,and being under considerable strain.

Figure 3.Maslow’s hierarchy of needs.
3.2.3. Chronic work overload
Apart from sleep disturbance,chronic work overload was an unresolved issue during the COVID-19 outbreak.Healthcare professionals,including physicians,nurses,and other professionals,worked beyond the limit of their capacities,particularly in the first wave of the pandemic.They were on duty for extra hours or without taking suitable breaks.They were also placed on high alert,leading to critical care nurses facing medical uncertainties and the possibility of suffering from chronic physical strains.The consequential results of being overworked and facing a missing work–life balance were explicit and possibly caused the professionals to be vulnerable to and infected with COVID-19.48,49Likewise,the physical pain of chronic overload was expressed.Furthermore,the shortage of the staff combined with the tendency to be overworked would be increased when individuals fell ill,resulting in a vicious circle.
The daily stress would induce upsetting feelings,leading to persistent negative emotions,detrimental effects on the physical and mental health,and triggering new problems to the situation.The COVID-19 pandemic can be likened to a domino effect hitting critical care nurses,who shoulder the responsibility for saving patients’ lives under unexpected circumstances and inducing worsening outcomes,as shown in Figure 4.

Figure 4.The effects of COVID-19 inducing relevant factors on the psychological and physical health’s critical care nurses.COVID-19,coronavirus disease;PPE,personal protective equipment.
3.3.Suggestions for alleviating the suffering of critical care nurses
The health and wellbeing of clinical staff,particularly nurses,significantly deteriorated during this recent pandemic.These nurses have frequently been frontline staff and involved in patients’ care.The nurses should have adequate working conditions and health protection,namely,the provision of essential and sufficient PPE,and appropriate and sufficient rest and rehabilitation programs that promote resilience and psychological wellbeing.24,28,32,33,50The methods for reducing the negative experiences of nurses were required,including financial and non-financial support,quality communication,adequate training or hiring of staff,adequate PPE,and suitable work shifts.36Furthermore,limiting the number of night shifts,assuring holidays,raising salaries,and closely monitoring professionals who worked in the ICU for extended periods should be considered.51Educational strategies,plans,and preparation would also be vital to deal with unforeseen circumstances that might occur in the future.26,31,35,52Hence,the following issues are vital to be guaranteed for critical care nurses,including basic daily needs,suitable and adequate PPE and training,proper work shifts,appropriate salaries and holidays,and effective communication and support services.
4.Discussion
In this comprehensive review of various existing studies,the threat of COVID-19 resulted in critical care nurses undergoing the changes from routine work to an unfamiliar working environment and processes,enormous workload and prolonged exhaustion,worries about being infected and infecting their families,disruption to their daily life,and witnessing the unsuccessful attempts to cure critically ill patients with this infectious disease.Additionally,there was no cure for COVID-19 during the time this review was conducted.Supportive nursing care was the dominant form of care for patients like that provided for a new communicable disease—Ebola.53Moreover,nurses had to treat the illness and raise the morale of worried patients,which emotionally took a toll on them.Therefore,due to the COVID-19 pandemic,the nursing profession was transformed into a very tough challenge,straining nurses physically and psychologically through institutional,social,and individual factors.
Institutional factors include work organization,work area,location,role change,lack of PPE,protocol inconsistencies,a shortage of staff (workload),and unsatisfactory training.Meanwhile,being afraid of infecting family members,bereavement,inability to take care of family members,stigma from the community,and the seriousness of the disease were the main social factors.These could cause mental conditions followed by a reduced quality of care and burnout due to over-stretching,as occurred with the H1N1 influenza pandemic.54,55Individual characteristics also have an impact on ICU nurses’ psychological and physical health,including female gender,resilience,self-perceptions,self-efficacy,and self-adjustment.Unsurprisingly,healthcare professionals,especially nurses,encountered difficulties during the pandemic.Similarly,nurses who cared for patients with communicable diseases such as Severe Acute Respiratory Syndrome (SARS) or Middle East Respiratory Syndrome (MERS) experienced high levels of psychological trauma during and after caring for the patients.56,57The intention,professionalism,and mental health of nurses could be negatively impacted by psychological pressures,according to studies conducted during the MERS and influenza outbreaks.58–60
A system for managing nurses’ psychological wellbeing and offering necessary support is clearly required to prevent psychological trauma,particularly in frontline nurses.56Additionally,basic daily needs,suitable and adequate PPE and effective training,proper work shifts,appropriate salaries and holidays,and effective communication are suggested to help critical care nurses successfully encounter this situation.24,28,32,33,36,50,51,56Providing the necessary training for using PPE and the adequate supply of quality PPE could decrease the fears of staff during the MERS pandemic.61Apart from supportive services,training during the pandemic is vital and is highlighted because information overload could be a handicap to proper patient care.Thus,necessary knowledge and effective training including evidencebased knowledge and clinical skills should be of considerable concern.58,62
According to studies during the past outbreak,adverse effects could also be diminished through the provision of social support.56,63–65Similarly,institutional support,including recognition of nurses and sufficient logistics provision could be important facilitators to nurses’ health.66–68Although it is critical to protect the nursing community during a pandemic through social campaigns or organizational policies,providing social support by considering national and cultural factors is suggested to enhance the effect of such movements.69,70Furthermore,a program for stress control and mental health is necessary to prevent psychological trauma among nurses.56Plans and preparations for unforeseen circumstances are also needed for frontline nurses.26,31,35,52
Most of the existing studies were conducted in general healthcare workers who were involved in caring for patients with COVID-19.14,16,18,25–27,30,32,33,41,45,48,71–75ICU professionals were also more paid attention.15,20–23,28–29,35,39,43,49,51,76–78A few studies focused on general nurses.31,40,79,80Meanwhile,some recent studies were performed in critical care nurses.17,19,24,36,42Moreover,those studies concentrated on the psychological health of healthcare staff during the COVID-19 pandemic rather than physical consequences.However,this communicable disease could not be eradicated.Healthcare workers who are in the frontline and encounter critically ill patients with new diseases and no cure should be taken care of both mentally and physically and should receive supportive services.Institutional plans and preparation are also needed beforehand.
5.Limitations and practice
There are several limitations.Owing to most studies conducting a survey,self-reporting and interviews might lead to individual bias.However,they were obtained from the firsthand experiences of critical care nurses who have directly dealt with the COVID-19 pandemic.Moreover,this review article may be biased because of the nature of the study design and the specific aspects of the selected topical issues.Conducting individual studies provided differences in place,time,and situation.Thus,the findings were possibly different.Additionally,this study was limited to studies published in English;hence,other significant articles may have been excluded.However,this article also gathered information from the most up-to-date studies that were performed in critical care nurses in diverse areas of the world.Consequently,the trends of COVID-19 impact on critical care nurses could be drawn and broadly presented to emphasize the appropriate solutions.
These findings might raise the awareness of critical care nurses and institutions about the impacts of the COVID-19 pandemic on nurses’ health.The causes and outcomes identified may assist in improving supportive services and preparations or plans for further pandemics.Nurses who shoulder the responsibility of caring for severely ill patients could have psychological and physical support,services,and strategies for addressing unforeseen changes.
6.Conclusions
Critical care nurses’ psychological and physical health were overwhelmed by the adverse effects of the institutional and social response and individuals’ reactions to the COVID-19 pandemic.Loss of wellbeing disrupted daily life and falling ill was a consequences of the nurses’ hard work.Preparation for the unexpected circumstances of other communicable pandemics and methods for mitigating the suffering of the nurses should be considered and sustainably developed.
Ethical approval
Ethical issues are not involved in this paper.
Conflicts of interest
All contributing authors declare no conflicts of interest.
- Frontiers of Nursing的其它文章
- Investigating adverse events in long-term care facilities: a systematized review
- A bibliometric analysis and visualization of research on heart failure complicated with malnutrition
- Implementation and achievements of enhanced recovery after surgery program in perioperative management of gastric cancer patients†
- Dietary adherence and the associated factors among Indonesian patients with type 2 diabetes: what should we be concerned about?†
- Factors related to self-management behavior among persons with mildto-moderate chronic obstructive pulmonary disease in Wenzhou,China
- Knowledge,attitude,and practices related to medication errors among nursing professionals: a questionnaire-based study in a tertiary care hospital