Efficacy of scleral buckling for the treatment of rhegmatogenous retinal detachment using a novel foldable capsular buckle
Fang-Fang Fan, Chang Xiao, Liang Wang, Xin-Ting Wang,3, Dan-Dan Liu, Xing Ge,Ya-Lu Liu,3, Su-Yan Li,3
1The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
2Department of Ophthalmology, Xuzhou First People’s Hospital, Xuzhou 221116, Jiangsu Province, China
3Eye Disease Prevention and Treatment Institute of Xuzhou,Xuzhou 221116, Jiangsu Province, China
4The Affiliated Shuyang Hospital of Xuzhou Medical University, Shuyang 223600, Jiangsu Province, China
Abstract
● KEYWORDS: rhegmatogenous retinal detachment;scleral buckling; foldable capsular buckle
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) occurs on the basis of retinal breaks, where liquefied vitreous enters the potential subneuroepithelial space, causing the separation of the retinal neuroepithelium from the retinal pigment epithelium[1-3].Patients often have symptoms such as fixed black shadows in front of the eyes, distortion of vision when the macula is involved, and loss of visual acuity[4-6].Retinal breaks are mainly closed surgically, and for uncomplicated RRD, treatment is primarily performed by scleral buckling operation[7-8].Scleral buckling is an extraocular procedure for RRD, and patients do not require long-term postoperative immobilization[9-10].Furthermore, this extraocular surgical operation does not accelerate cataract formation in the operated eye after surgery[11-12].However, we cannot ignore some disadvantages that still exist with scleral buckling: the need for the operator to use an indirect binocular ophthalmoscope intraoperatively, which means a long learning curve for inexperienced surgeons.Furthermore, intraoperative stretching of the rectus muscle may increase the oculo-cardiac reflex as well as intraoperative and postoperative pain in patients, and long-term scleral buckling still raises the risk of postoperative refractive dioptre changes or diplopia in patients[13-17].
During the 1970s, Lincoffet al[18]developed a device, named the Lincoffballoon, for temporary indentation beneath a retinal break.However, it was not accepted for popular application mainly due to the tube being exposed outside and not being commercially available.The foldable capsular buckle (FCB)is a novel modification of the Lincoff balloon, in which the drainage tube is folded and sutured under the conjunctiva.This greatly reduces the risk of infection, as well as complications such as discomfort and foreign body sensation[18-20].
The FCB is a remodel of the foldable capsular vitreous body (FCVB) AV-10P model[21-23]and an innovative product independently developed by Vesber Biotechnology Co., LTD,Guangzhou, China.It has been approved by the State Drug Administration as a Class III medical device (Registration Certificate No.20173123296) and has also passed CE certification in the European Union, TGA certification in Australia and MHRA certification in the United Kingdom.The material of FCB is the same as that of FCVB, which is made of FDA-approved pure silicone that has been safely used in the human body for more than 20y with good biocompatibility.The FCB consists of a very thin lumen-shaped balloon and a tube-valve system[24-25](Figure 1A).In most selected cases,FCB can be used without fixation sutures, cryotherapy,drainage, or traction sutures for external ocular muscles.It can replace the conventional silicone buckle in scleral buckling surgery.
However, only a few studies have been reported on FCB scleral buckling to treat RRD.Our present series of observational studies were conducted to investigate the effectiveness and safety of FCB scleral buckling in the treatment of RRD.In this study, we used FCB scleral buckling and observed the intraocular pressure (IOP), best corrected visual acuity(BCVA), refractive dioptre, astigmatism degree, intraoperative complications, eye movements, and retinal reattachment rate.The results were analysed to provide practical support for the treatment of RRD with FCB scleral buckling.
SUBJECTS AND METHODS
Ethical ApprovalThe research process conformed to the Helsinki Declaration and was reviewed and approved by the Ethics Committee of Xuzhou First People’s Hospital.The ethical approval document is xyyll [2020]49.The study purpose, study steps, precautions, and contingency management measures were fully explained.All subjects understood and agreed to participate in this study, and an informed consent form for enrolment was signed before the start of the examination.
SubjectsThis was a series of case observation studies.The inclusion criteria were as follows: 1) patients who voluntarily participated in the study; 2) patients who were older than 18 years old, male or female; 3) patients who met the diagnostic criteria for RRD with a single break [size<2 papillary diameter(PD)] or multiple adjacent breaks <3 PD in one quadrant,proliferative vitreoretinopathy (PVR)-C2 level or less; 4)patients who were in good general condition and had no contraindications to surgery; 5) patients who understood the purpose of the study, voluntarily participated and signed the informed consent form.
Exclusion criteria were as follows: 1) retinal break that had a rolled edge, with pulling, or was located in the ora serrata, the posterior pole of the fundus; 2) other ophthalmic concomitant diseases that could not be controlled, such as glaucoma,grade 3 or higher nuclear cataract and macular disease; 3)endophthalmitis; 4) history of previous ocular surgery, or ocular trauma; 5) known allergy to silicone, presence of keloids.
Ophthalmic ExaminationEach patient’s BCVA was checked with a standard logarithmic visual acuity chart.IOP was measured with a noncontact tonometer, and the dioptre and astigmatism degree were measured with autocomputer optometry and retinoscopy.The anterior segment of the eye was examined with a slit lamp microscope.The fundus was examined with a 120 D preplaced mirror, and a B-scan ultrasound instrument was used to examine the vitreous condition.Retinal detachment was examined, and retinal reattachment and subretinal fluid absorption were recorded using optical coherence tomography (OCT).
Surgical ProcedureThe surgeries were all performed by the same experienced clinician (Li SY).Preoperatively, the retrobulbar and supraorbital nerves were anaesthetized with a total of 5 mL of 2% lidocaine and 0.75% bupivacaine (1:1).Traction sutures were made along the corneal limbus at the meridian line of the retinal break.The bulbar conjunctiva 5-66 mm posterior to the limbus was cut approximately 4-5 mm long parallel to the limbus.The bulbar conjunctiva and Tenon fascia tissues were separated, and a narrow tunnel was made approximately 12-14 mm long along the episclera posteriorly.Anterior chamber puncture was performed to release a small amount of aqueous humour to lower the IOP.The localization of retinal breaks was performed with scleral indentation under an indirect ophthalmoscope or operating microscope.Prefixed sutures were made with 5-0 nonabsorbable sutures 4 mm anterior to the posterior margin of the retinal break.The FCB was filled with sterilized air to test for leakage, evacuated and folded, and then placed through the premade tunnel with the spherical surface facing the sclera using intraocular lens (IOL) platform forceps.Approximately 1 mL of balanced salt solution was injectedviathe tube valve,which was secured with a 5-0 nonabsorbable suture at the tube proximal to the FCB.After checking the indentation position,the conjunctiva with Tenon’s capsule incision was closed with sutures, and the tube valve was buried under Tenon’s capsule.Tobramycin dexamethasone eye ointment was applied, and the eye was bandaged (Figure 1).
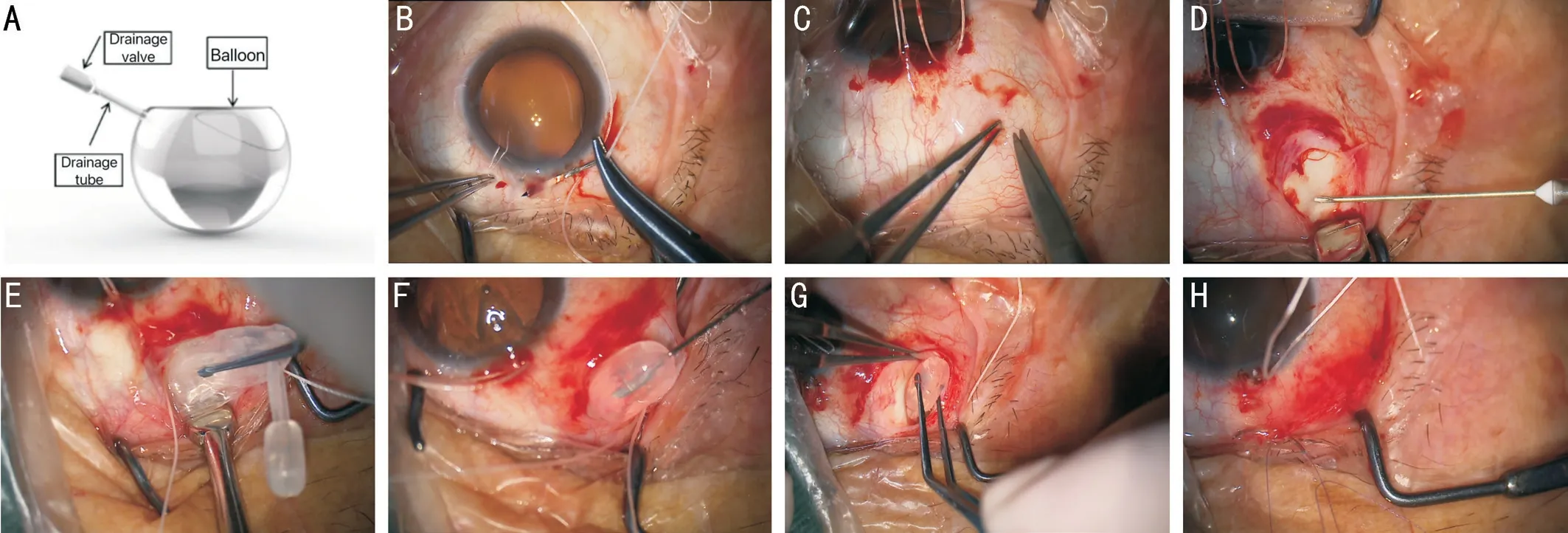
Figure 1 Photographs of FCB and brief procedure of FCB scleral buckling A: FCB composed of a balloon, drainage tube and drainage valve; B:Traction sutures are made along the corneal limbus at the meridian line of the retinal break; C: The bulbar conjunctiva 5-6 mm posterior to the limbus is cut about 4-5 mm long parallel to the limbus; D: A 1-mL syringe needle is used to puncture the sclera and drain the subretinal fluid;E: FCB is filled with sterilized air to test for leakage, evacuated and folded, using an IOL platform forceps; F: Approximately 1 mL of saline was injected via the tube-valve; G, H: FCB is embedded and the conjunctival with Tenon’s capsule incision is closed.FCB: Foldable capsular buckle;IOL: Intraocular lens.
The postoperative medication included levofloxacin and tobramycin dexamethasone eye drops.Combined vitreous cavity gas injection and laser photocoagulation were performed when needed according to the retinal reattachment status.Patients with high IOPs were treated with combined IOPlowering drugs.
The patients were followed up for 3-6mo postoperatively.The balloon fluid was removed 3mo after surgery using a 1-mL syringe under surface anaesthesia in the outpatient clinic or the operating room, depending on the retinal recovery and the patient’s balloon position.
Statistical AnalysisThe statistical software SPSS 26.0 was used for statistical analysis of the data.Normally distributed measures are expressed herein as the mean±standard deviation.Overall differences at each preoperative and postoperative follow-up time point were compared using repeated-measures ANOVA.Two-by-two comparisons at multiple time points were statistically performed using the LSD-ttest.Nonnormally distributed measures are expressed as the median and interquartile range [M (Q1, Q3)]; the Friedman test was used for different indicators at multiple time points.Differences were considered statistically significant atP<0.05.
RESULTS
General Preoperative ConditionsFinally, 18 patients (18 eyes) were diagnosed with RRD and determined to be eligible for FCB scleral buckling.The basic clinical characteristics of the study subjects are presented in Table 1.All 18 patients received complete FCB scleral buckling surgery.At the 3-month postoperative follow-up, the retina was reattached in 16 eyes in a single operation, with an 88.9% single-operation anatomic success rate.Six months postoperatively, the final retinal reattachment rate was 100%.All patients underwent intraoperative cryopexy therapy, with 1 patient receiving preoperative laser photocoagulation and 3 patients receiving preoperative laser photocoagulation.Intraoperatively, two eyes were intravitreally injected with 0.3 mL of perfluorocarbon gas (C3F8).In 2 cases, a secondary buckling procedure was performed, one for a new retinal break and an undetected break, and the retina was reattached thereafter.No intraoperative complications occurred in any of the procedures (Figure 2).The BCVA of the patients significantly improved after surgery.The difference was statistically significant when comparing the BCVA at each time point before and after surgery(Ftime=15.905,P=0.001).There was a negative trend for increased dioptres in the operated eye after surgery.However,the difference was not statistically significant (P>0.05).There was also a negative trend for increased astigmatism degree after surgery in the operated eye (P>0.05; Table 2).
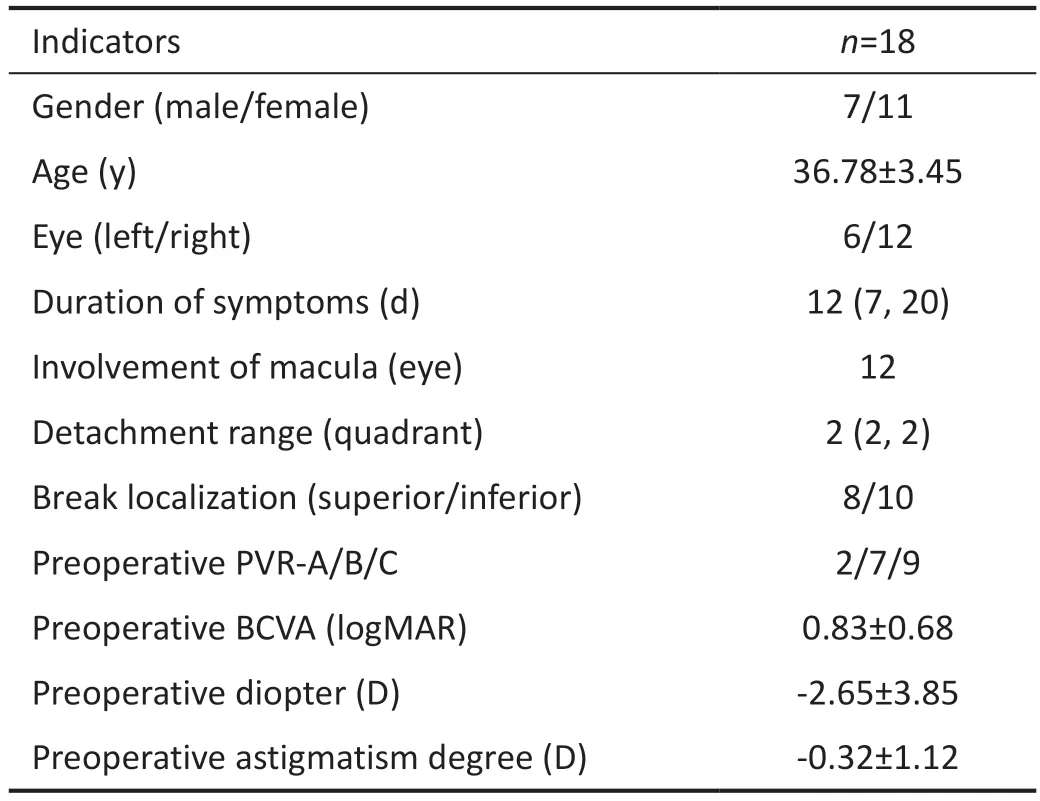
Table 1 Clinical characteristics of the study subjects
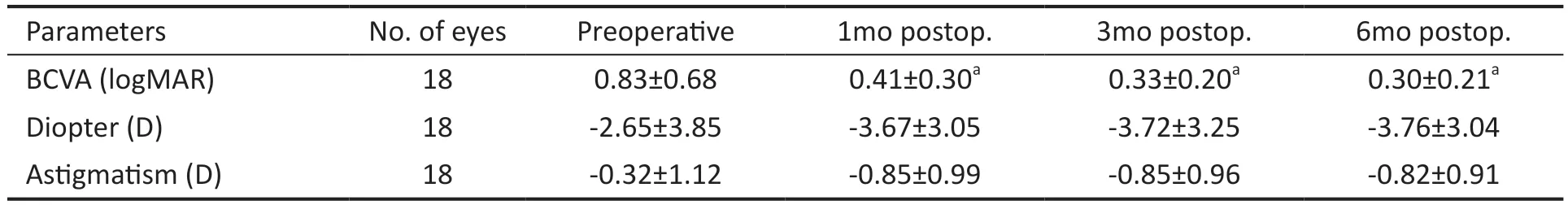
Table 2 Changes in BCVA, dioptre, and astigmatism degree after surgery
Three patients had transiently high IOPs within one week after surgery, which returned to normal levels after the use of IOP-lowering drugs.Five patients had diplopia after surgery,which disappeared after balloon fluid removal.There was no postoperative balloon displacement.
DISCUSSION
In this study, we analysed 18 patients who were treated for RRD using scleral buckling with FCB.The study aimed to evaluate the postoperative retinal reattachment rate, BCVA,IOP, and other factors.The results showed that the success rate of postoperative retinal reattachment using FCB scleral buckling for the treatment of RRD was high, with anatomical success achieved in 16 out of 18 patients (88.89%).However,retinal redetachment occurred in 2 patients, and they needed secondary surgery.Previous studies have reported that the single-operation anatomical success rate of balloon-assisted scleral buckling for RRD ranges from 80% to 100%[1,18,20,22,24,26-27].Factors contributing to the failure of the procedure include inadequate buckling, undetected breaks, new breaks discovered after surgery, choroidal detachment, balloon prolapse,another break, inadequate adhesion, break caused by vitreous retraction, proliferative vitreoretinopathy (PVR),etc[19].Secondary surgical procedures may involve scleral buckling surgery or minimally invasive pars plana vitrectomy (PPV).In this study, the reasons for the two patients requiring secondary surgery were a new break discovery and an undetected break,respectively.Both patients had high myopia, and the extent of retinal detachment was limited in these cases.The location of the breaks was clearly defined.As a result of the secondary surgery, final retinal attachment was achieved in 2 patients through scleral buckling surgery.
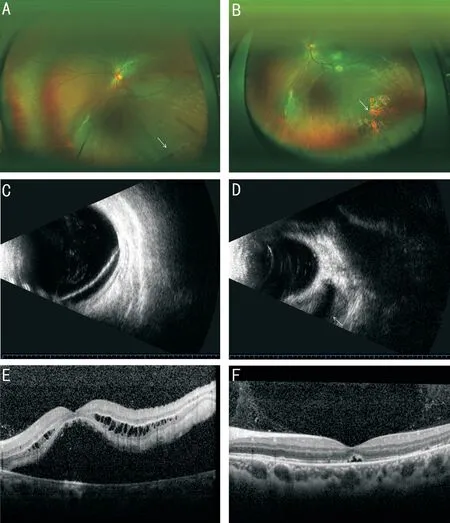
Figure 2 Fundus images of a 19-year-old male with retinal detachment treated using FCB A: Ultra-field fundus photo shows a horseshoe retinal tear (arrow) with inferior-temporal detachment and macular off.B: The retina completely reattached with the tear sealed (arrow).B-scan ultrasound photos show retinal detachment before operation (C) and the retina reattached with FCB indentation(arrow) postoperatively (D).OCT shows the macula highly detached(E) and flatten with a tiny residual subretinal fluid 6mo after surgery (F).FCB: Foldable capsular buckle; OCT: Optical coherence tomography.
In this study, we found that FCB scleral buckling surgery resulted in improved postoperative BCVA compared to the preoperative BCVA.The patients’ eyes also experienced an increase in dioptre, particularly in the astigmatism degree,although this difference was not statistically significant when comparing the preoperative and postoperative periods.However, it is worth noting that in traditional scleral buckling surgery, the sutured silicone buckle exerts pressure on the eye in different directions, especially when the retinal break is located under the rectus muscle.This can potentially cause deformation of the eye and result in changes in refractive status.On the other hand, in FCB scleral buckling surgery,the fluid in the balloon used can be removed after closing the retinal break.This feature helps to minimize the impact on the astigmatism degree of the affected eye, which is consistent with another study by Xueet al[28].However, in our study,patients still showed a slight trend of an increasing astigmatism degree.Nevertheless, it is possible to remove the balloon fluid in the later stage based on the patient’s retinal recovery situation to alleviate the impact on the astigmatism degree.Further research is needed to better understand the long-term effects of FCB scleral buckling surgery on refractive status and astigmatism degree.
Previous studies have reported that there may be some risks and complications associated with scleral buckling surgery[26-27,29].These include an increased risk of postoperative infection.The balloon used can be completely buried under Tenon’s capsule, reducing the risk of infection, and removal of the balloon can be performed within a few days or a couple of weeks after surgery.Additionally, some patients may experience recurrent retinal detachment, which may require a second operation.Furthermore, the balloon fluid is removed after three months based on the patient’s retinal recovery,which allows for a longer placement of the balloon under Tenon’s capsule.This offers flexibility, as the FCB can be removed based on the patient’s preferences.It is worth noting that four patients in this study had delayed (between 3 and 6mo) balloon fluid removal due to the presence of PVR and proliferating membranes, which hindered the absorption of subretinal fluid.
In terms of IOP, three patients experienced transiently high IOPs within the first week after surgery.The increase in IOP may be attributed to the extrascleral pressure caused by the balloon, which can cause a shallow anterior chamber depth.Prolonged pressure may lead to ciliary body oedema, thereby hindering aqueous efflux and maintaining an elevated IOP.However, this was manageable and successfully relieved with medication.The results of this study align with previous research conducted by other scholars[30].Postoperatively,diplopia occurred in 5 eyes.However, the diplopia symptoms disappeared after the balloon fluid was removed, which was consistent with the findings of previous studies[31].
The maximum area of the balloon pressure on the sclera is approximately 1 cm in diameter.Therefore, the indications for using this technique are the same as those for the Lincoffballoon.It is suitable for a single break within a quadrant with a size of less than 2 PD or multiple adjacent breaks with an extent of less than 3 PD.Additionally, the procedure is applicable for cases with grade PVR-C2 and less.If the retina is not successfully reattached after surgery, further treatment with conventional procedures such as scleral buckling or PPV surgery is also possible.
This study demonstrated that FCB scleral buckling surgery for the treatment of RRD is simple and easy to perform, with few postoperative complications.Additionally, the use of a balloon allows for its removal after retinal reattachment,avoiding refractive changes caused by deformation of the eyeball and minimizing effects on eye muscles and local blood circulation.However, this investigation is limited because it was only a descriptive study comparing FCB scleral buckling to traditional scleral buckling, without a control group.The analysis of the advantages and disadvantages of the two methods was based on previous experience and lacked substantial data.Furthermore, the study had a short follow-up time and a small sample size, potentially missing long-term surgical complications and other adverse events.Therefore,future research should focus on increasing the sample size and implementing longer-term, randomized, controlled studies to further investigate the benefits of FCB scleral buckling,with the aim of developing a safer, more efficient, and more comfortable surgical procedure for patients.
ACKNOWLEDGEMENTS
We wish to thank Zheng-Pei Zhang, Hai-Yang Liu, Su-Juan Ji, Li-Na Guan, Wei Fan, Ai-Qin Sheng and Jie Li from the Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University for the support in this research project.
Authors’ contributions:Concept and design: Fan FF, Li SY;data acquisition: Fan FF, Xiao C, Ge X, Liu DD; data analysis/interpretation: Fan FF; drafting manuscript: Fan FF; critical revision of manuscript: Wang L, Xiao C, Wang XT, Liu DD,Ge X, Liu YL, Li SY; supervision: Li SY.
Foundations:Supported by Xuzhou Health Outstanding Talents Project (No.XWJC001); Critical Special Project for Social Development of Xuzhou (No.KC21153); Science and Technology Innovation Project of Xuzhou Municipal Health Commission (No.XWKYHT20230039); Applied Basic Research Project of Xuzhou (No.KC23016).
Conflicts of Interest: Fan FF,None;Xiao C,None;Wang L,None;Wang XT,None;Liu DD,None;Ge X,None;Liu YL,None;Li SY,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
