Drug delivery systems for colorectal cancer chemotherapy
Wen Chen ,Kun Shi ,Yan Yu,Peipei Yang,Zhongwu Bei,Dong Mo,Liping Yuan,Meng Pan,Yu Chen,Zhiyong Qian
Department of Biotherapy,Cancer Center and State Key Laboratory of Biotherapy,West China Hospital,Sichuan University,Chengdu 610041,China
Keywords: Colorectal cancer Chemotherapy Drug delivery systems Solubility Targeted Local administration
ABSTRACT Colorectal cancer causes the third most common type of malignant tumors with high morbidity and mortality.Chemotherapy is currently one of the most effective and common treatments for colorectal cancer.However,the poor water solubility of some chemotherapeutics,untargeted drug delivery,and the undesirable systemic side effects of conventional treatment remain the major issues for colorectal cancer chemotherapy.Fortunately,drug delivery systems (DDS) based on biomaterials have been widely investigated and found to be capable of resolving those issues with good performance.Therefore,the main goal of this review is to summarize and discuss the progress and potential advantages of different DDS for colorectal cancer chemotherapy.We not only reviewed the nanocarriers used to improve the solubility of chemotherapeutics,including liposomes,micelles,and nanoparticles,but also discussed targeted DDS based on specific ligand-receptor recognition and tumor microenvironmental stimulus responses.Furthermore,locally administered systems based on hydrogels and microspheres,which have been shown to increase drug accumulation at the tumor site while decreasing systemic toxicity,were also emphasized.DDS provides a good option for improving the efficacy of chemotherapy in the treatment of colorectal cancer.
1.Introduction
Cancer is one of the leading causes of human death worldwide,with increasing incidence and mortality every year [1].Colorectal cancer causes the third most common type of malignant tumors and has become one of the main public health problems in both developed and transitional economies.According to the latest estimates and reports,the number of new cases of colorectal cancer has exceeded 1.9 million,and the death toll has reached 935,000,accounting for approximately 1/10 of cancer cases and deaths,making colorectal cancer the second leading cause of cancer-related deaths [2].From the data over the past five years (2012-2016),mortality among the elderly population is decreasing,while that in younger individuals is rapidly increasing [3-5].Surprisingly,younger patients are more likely to be diagnosed at an advanced stage,making for a non-optimistic survival rate.At present,the cause of the rejuvenation of the disease has not been entirely determined.
More than 95% of colorectal cancer cases evolve from colorectal polyps,which is one of the most common sites of gastrointestinal polyps.The formation of adenomatous polyps (also called precancerous polyps) due to the hyperplastic and hypertrophic nature of the normal intestinal mucosa usually leads to colorectal cancer [6].Because most colorectal cancer cases are considered to be the result of genetic and epigenetic changes in stem cells or stem cell-like cells that cause oncogenes to be activated,people with a clear history of intestinal polyps are at high risk for colorectal cancer [7].Certain lifestyle choices,such as smoking,excessive alcohol use,inactivity,and a diet that is unhealthy,are also inextricably linked to the increased incidence of colorectal cancer [8].Coupled with the fact that the early symptoms of colorectal cancer are not obvious and the wide range of screening is weak,many patients are found to be in an advanced stage when diagnosed [9].At this time,the cancerous tissue of the tumor has invaded the plasma muscle layer,which may even involve the adjacent peritoneum or organs,and the majority of these cases are accompanied by multiple metastases,making radical surgery difficult or the opportunity to operate be lost entirely [10].Colorectal cancer has become a severe threat to human life and health and is also a major challenge in current medical research worldwide.Therefore,controlling and treating of colorectal cancer are essential to reduce patient death and pain.
Currently,the standard clinical treatments for colorectal cancer include surgery,radiotherapy,and chemotherapy.In addition,some new treatment methods,such as targeted therapy and immunotherapy,have emerged in recent years.However,there are still many limitations in colorectal cancer treatment in clinical practice.Although surgery is the main means of radical treatment for early-stage colorectal cancer,the therapeutic effects of surgical resection are restricted by local relapse and metastasis,which greatly affect the survival rate [11,12].Therefore,postoperative chemotherapy is still needed to reduce the risk of recurrence.Radiation therapy has a strong killing effect oninsitutumors and is less damaging to normal tissues,but it is challenging to locate early metastases accurately,and this treatment modality may also cause bladder and sexual problems [13].Chemotherapy remains an essential choice for most cases that cannot be treated surgically or with radiotherapy.First,palliative chemotherapy in patients with advanced colorectal cancer can control colorectal cancer development to prolong and improve the quality of life [14,15].In addition,chemotherapy as neoadjuvant or adjuvant therapy before and after surgery is an irreplaceable treatment for preventing the recurrence and metastasis of colorectal cancer [16,17].Unfortunately,limiting factors such as the poor water solubility of some chemotherapeutics,nontargeted drug delivery,and the undesirable systemic side effects of conventional chemotherapy still lead to poor clinical benefits and affect the quality of life of and acceptance by patients.
As early as the 1950s,drug delivery systems (DDS) for cancer treatment began to emerge,dramatically changing the current drug therapy landscape [18-20].What is remarkable is that DDS based on biomaterials was able to resolve the above issues while showing good performance in colorectal cancer chemotherapy.Among them,the nanoencapsulation of chemotherapy drugs by biomaterials has been widely studied and can surpass some limitations of traditional chemotherapy drugs,namely,boosting the solubility of therapeutics that are weakly soluble in water,reducing systemic toxicity and enhancing drug efficacy.In addition,nanoencapsulation can coload drugs in the same nanocarrier to simultaneously deliver two or more drugs [21-23].Compared to normal cells,nanodrugs preferentially target solid tumors by utilizing the enhanced permeability and retention (EPR) effect of the vascular system of solid tumor tissues,making them likely to accumulate in tumors over time [24,25].For the treatment of colorectal cancer,a number of nanodrug delivery systems are being investigated,including liposomes,micelles,polymer nanoparticles,and inorganic nanoparticles.Abraxane,a paclitaxel (PTX) albumin nanoparticle,is available in more than 50 countries worldwide and has been approved for multiple indications,including breast,lung and pancreatic cancer [26].Moreover,drug-loaded nanoparticles can not only accumulate in tumor tissues as a result of the EPR effect (passive nanocarriers) but also actively target cancer cells [27-29].The surface of colorectal cancer cells selectively expresses specific receptors or molecules,which can bind to the corresponding ligand and initiate a series of signal transduction pathways related to the proliferation of cancer cells [30].Thus,the surface of the nanocarrier can be functionalized with ligands to identify and bind to highly expressed receptors on the surface of tumor cells,enabling active targeting [31-33].In addition,chemotherapeutics are typically adsorbed onto,conjugated to or coated within the nanocarrier and released to the tumor targets as the local environment changes,such as by varying the pH,enzymes,reactive oxygen species (ROS),glutathione (GSH),and magnetic fields [34].
It is worth mentioning that,compared with traditional chemotherapy,local drug administration can not only realize the local sustained release of chemotherapeutics but also reduce systemic toxicity,thereby significantly improving the effectiveness of chemotherapy [35,36].Various systems,such as hydrogels,nanocomposite hydrogels,and microspheres,have been investigated to deliver drugs locally to treat colorectal cancer.Owing to their slow drug release performance,hydrogel systems can ensure the local concentration of therapeutic drugs and inhibit the side effects brought on by high levels of chemotherapeutics in the blood[37].In addition,some nanomaterials can confer excellent mechanical and physical properties or special stimulus responsiveness to hydrogel systems due to their inherent nano properties.
These various DDS provide excellent options for enhancing chemotherapy efficacy in colorectal cancer treatment.Here,we review the progress and potential advantages of DDS for colorectal cancer chemotherapy,including those used for improving the solubility of chemotherapeutics,those that are targeted based on specific ligand-receptor recognition and tumor microenvironmental stimulus responses,and those that are administered locally (Fig.1).

Fig.1.Schematic illustration of DDS for colorectal cancer chemotherapy,including those that can improve drug solubility,targeted delivery,and local delivery.
2.Drug delivery systems for improving drug solubility
Chemotherapy is one of the most effective and common treatment modalities for colorectal cancer,along with surgery and radiation therapy,and collectively,these options are known as the three significant therapies for cancer.Many commonly used chemotherapeutic drugs,such as PTX,docetaxel (DOC),camptothecin (CPT),and capecitabine (CAPE),have low bioavailability due to their poor solubility,limiting their clinical application.Taking commercial PTX as an example,although ethanol and Cremophor EL have been used together to improve the solubility of PTX,Cremophor EL can produce serious side effects,such as severe anaphylactoid hypersensitivity reactions,peripheral neuropathy and neutropenia [38-40].The rise of the use of DDS has brought new hopes for improving the water solubility of these insoluble drugs.In particular,encapsulating hydrophobic drugs into nanoparticles can effectively improve their water solubility.In addition,due to the enhanced EPR effect of the vascular system of solid tumor tissue,nanoparticles can be preferentially concentrated in the tumor site and serve as a local drug repository to continuously supply therapeutic drugs [41,42].Because of this passive tumor targeting mechanism,nanodrug delivery systems may become promising hydrophobic anticancer drug delivery systems widely used in solid tumor chemotherapy [43,44].This section mainly summarized the research progress of nanodrug delivery systems based on liposomes,micelles,polymer nanoparticles,and inorganic nanoparticles to improve the solubility and stability of insoluble chemotherapeutics in colorectal cancer chemotherapy.
2.1. Liposomes
Liposomes were first described as drug carriers encapsulating anticancer drugs in 1973 and thus became one of the most widely used nanodrug systems approved by the Food and Drug Administration (FDA).Liposomes are monolayer or multilayer vesicular substances usually composed of phospholipids [43,45].Phospholipids are amphiphilic molecules,with the hydrophilic portion at the head and the hydrophobic portion at the tail,which colloids in water.Liposomes have a wide range of drug loading abilities,high efficiency,and low toxicity and can carry both hydrophilic and lipophilic drugs,which may enhance the solubility of chemotherapeutics and endow them with sustained release properties [46-48].Liposomal DDS can generally be classified into four types: conventional liposomes,sterically stabilized liposomes,ligand-targeted liposomes,and their combinations [49].
Lipusu,PTX liposomes for injection,is the first PTX liposomal drug to be marketed globally [50].PTX,which is difficult to dissolve in water,was encapsulated in a new drug carrier-liposome phospholipid bilayer,which solved the solubility problem of PTX.Studies have shown that different concentrations of PTX liposomes restrict the growth of rectal cancer Colo320 cellsinvitroand promote cell apoptosis [51].The Chinese treesCamptothecaacuminataandMappiafoetidaare used to produce CPT,a naturally occurring water-insoluble alkaloid that has potent anti-colorectal cancer activity.An innovative CPT-liposome (egg phosphatidylcholine and 1,2-dioleoyl-3-trimethylammonium-propane liposome,EPC-DOTAP liposome) was found to dissolve more CPT,achieving therapeutic concentrations in excess of 200 mg/mL [52].However,due to the rapid adhesion of plasma proteins to the surface of the liposomes,traditional liposomes in the liver and spleen stimulate their immediate clearance from the blood circulation by the mononuclear phagocyte system (MPS) [53].Stereo stable liposomes (or long circulating liposomes) were introduced to overcome the above deficiencies.The surface of these liposomes are modified by hydrophilic materials such as polyethylene glycol (PEG),which endows the material with a long circulation time and threedimensional stability,so this approach has been widely studied.Another study conducted by Yoshizawaetal.tested PTX formulations synthesized by PEG liposomes to improve the water solubility of PTX,increase the accumulation of PTX at the location of the colorectal cancer tumor,and reduce side effects [54].This study assessed the distribution of solid colon-26 tumors in mice and the ability of PTX-liposomes to treat cancer.Invivo,the outcomes of the experiment indicated that the PEGylation of liposomes increased the area under the plasma concentration-time curve (AUC)in the tumor by 3.8-fold and the AUC tumor value of PTX by 1.8-fold,so the PTX-PEG liposomes considerably increased the survival time of colon-26 tumor-bearing animals.A reliable liposomal formulation of 9-nitro-camptothecin (9-NC) was created and profoundly improved the lactone stability of CPTinvivoand consisted of phospholipids,cholesterol,and short-chain PEG fatty acids [55].9-NC was 100 times more soluble in the preparation with a mean vesicle size of 900 nm,which caused the biological half-life to increase by more than a factor of 10.
2.2. Micelles
Polymer micelles have been synthesized and assembled by various amphiphilic block copolymers with a hydrophobic core and a hydrophilic outer portion.Hydrophobic drugs can be wrapped in the core of the micelle by hydrophobic interactions between molecules [56,57].After being loaded into micelles,hydrophobic drugs are uniformly dispersed in aqueous solution to form a uniform suspension,increase bioavailability and improve the cancer treatment effects [58,59].
While many researchers are working to solve the problem of the poor water solubility of chemotherapeutics,they have also managed to use multimodal combination therapies based on micelles,such as dual drug combinations,triple drug combinations,and chemotherapy/gene therapy,to treat colorectal cancer.The nontoxic micelles prepared by poly(ethylene glycol)2000-phosphatidyl ethanolamine conjugate (PEG2000-PE) and D-α-tocopheryl polyethylene glycol 1000 succinate (TPGS) effectively solubilized the insoluble anticancer drug PTX and were stable at low pH values and in bile acid,which could be a viable method by which PTX could be delivered orally [60].Block copolymer micelles made of poly(ethylene glycol) and poly(L-aspartate ester) successfully incorporated CPT with mean particle diameters ranging between 60 and 110 nm and a high incorporation efficiency generated by an evaporation method [61,62].Because of the higher bioavailability of CPT released from the polymer micelles,both a single injection of 30 mg/kg CPT micelles and three separate injections of 10 mg/kg generated considerable tumor regression in mice with solid colon cancer tumors.By using the dialysis process,polymeric micelles based on chitosan were created and then added to CPT previously dissolved in DMSO at a concentration of 1 mg/mL to obtain CPT-loaded micelles with stirring to give 15%(w/w) drug loading (Fig.2) [63].This CPT-loaded micelle with a particle size of 178±6 nm had an association efficiency of 55.5%± 8.9% and a drug loading of 8.3% ± 1.3%.Additionally,these CPTloaded micelles demonstrated a considerable reduction in tumor growth in more sophisticatedinvivochemically induced colorectal cancer and HCT116 xenograft tumor models.Gaoetal.prepared mixed PTX and curcumin (Cur) polymeric micelles (PTX-Cur-M) and aimed to apply polymeric micelles to simultaneously codeliver two hydrophobic chemotherapeutic drugs,PTX and Cur,to make the commercial formulation of PTX less toxic and increase colon cancer antitumor efficacy [64].Their results demonstrated that PTX-Cur-M could release PTX and Cur over a long period of timeinvivoandinvitroand had antiangiogenic activity.Moreover,apoptosis-inducing and anti-angiogenesis functions might be main mechanisms by which CT26 colon cancer cells were inhibited by PTX-Cur-M.Choetal.synthesized poly(ethylene glycol)-block-poly(D,L-lactic acid) (PEG-b-PLA) micelles that were used to eliminate colon cancer tumors with optical imaging and drug delivery properties [65].In the LS180 human colon transplantation model,these micelles were used to carry three insoluble anticancer drugs,PTX,17-allylamino-17-demethoxygeldanamycin,and rapamycin (PTX/17-AAG/RAPA) and reduced tumor volume by a factor of 1.6.

Fig.2.(A) Experimental schedule.(B) Body weight changes over time.(C) Tumor growth (%) in the experimental group.(D) Tumor volumes in every animal following treatment.(E) Survival curves of mice after treatment with various concentrations.Copied with permission [63].Copyright 2022,Elsevier.
Additionally,multimodal cancer therapy combined with chemotherapy and gene therapy can result in an excellent drug codelivery system.Jangetal.used a conjugate (DA3) of low molecular weight polyethylenimine and deoxycholic acid (DA) (PEI 1.8 kDa) to synthesize micelles (DA3 micelles) for codelivering water-insoluble PTX and siRNAs to colorectal cancer tumor cells in a single vehicle [66].Solvent diffusion was used to create PTX-loaded DA3 micelles with a 15.6% drug loading content that condensed siRNA just as well as the drug-free DA3.The results of theinvitroexperiments showed that PTX/DA3/siRNA could allow the conjugates to enclose and dissolve PTX in a micelle-like core-shell configuration.
2.3. Polymer nanoparticles
The excellent properties of polymers,such as biocompatibility,low toxicity,and biodegradability,allow chemotherapeutics to be embedded or wrapped in their polymer matrix for drug delivery [67].Similar to polymeric micelles,polymer nanoparticles have the advantages of improving the solubility of insoluble drugs,increasing bioavailability,and enhancing biological distribution during drug delivery [68].
Smithaetal.developed PTX-loaded amorphous chitin nanoparticles (PTX-AC nanoparticles) assembled by an ionic cross-linking technique to address the problem of the poor solubility of PTX[69].In detail,they prepared novel amorphous chitin nanoparticles with an entrapment efficiency of 55%,which was appropriate for passive targeting through the EPR effect in the delivery of therapeutics for colorectal cancer.The results showed that the AC nanoparticles were hemocompatible and that the PTX-AC nanoparticles had activity against colorectal cancer cells (COLO-205 and HT-29 cells) and induced apoptosis.Additionally,this research assisted in the rationalization of polymer nanoparticle designs such as PTX-AC nanoparticles as a potential drug delivery platform to improve the water solubility of PTX.Optimized polycationic cyclodextrin (CD) nanoparticles for CPT administration were made,and these nanoparticles had a positively charged surface after being coated with polyethylenimine (PEI) or chitosan [70].With a diameter of 135 nm and a zeta potential of +40 mV,the best CPTloaded poly-CD-C6 nanoparticle formulation successfully delivered 52% of the encapsulated CPT to the simulated colon.Zakietal.designed poly(lactic-co-glycolic acid) (PLGA) nanoparticles containing certain pharmaceutical excipients (TPGS,Pluronic P85 and chitosan) to encapsulate hydroxycamptothecin (HCPT) that showed the maximum encapsulation efficiency and the lowest particle size[71].
Finally,unlike unmodified polymer nanoparticles,PEG-modified nanoparticles are frequently employed in DDS due to the advantage of being able to avoid the reticuloendothelial system (RES)barrier [72-75].Encapsulating free drugs in PEGylated polymer nanoparticles can not only improve the solubility of the drugs but also prolong the circulation time and provide sustained drug release,thus enhancing the anti-colorectal cancer effect [76].Phungetal.encapsulated PTX and dihydroartemisinin (DHA) into a PTXPEG-DHA complex (PD@PDD nanoparticles) using the emulsion evaporation method and evaluated the antitumor efficacy in an advanced mouse HT-29 tumor model [77].In this study,the tumors in mice treated with the dual drug nanodrug delivery system had a slower rate of development than the group that was administered only one drug,which showed that PTX might be delivered to tumors in a brand-new,synergistic method to increase HT-29 colorectal cancer apoptosis and have greater accumulation in the tumor siteinvivo.Schmidetal.reported on PEGylated polymeric nanoparticles designed with optimal ratios for the coencapsulation of the topoisomerase I inhibitor CPT and the BH3-mimetic ABT 737.This system also allowed CPT and/or ABT 737 to be contained within the hydrophobic PLGA core,making this system an optimized chemotherapeutic nanoformulation that can overcome its clinical limitations [78].Wangetal.produced an OXA (IV)prodrug with anti-inflammatory properties and GSH-depleting cyclodextrinpseudo-polyrotaxane carriers and further self-assembled into nanoparticles (designated DNPt@PPRI) to enhance the sensitivity of OXA [79].Generally,nanoparticles as carriers delivering PTX to improve its water solubility and limit its side effects have been widely studied [80].
2.4. Inorganic nanoparticles
The imaging and treatment of inorganic nanoparticles in colorectal cancer have received increased focus in recent years [81].One of the most common types of inorganic nanoparticles is gold nanoparticles (AuNPs) with the characteristics of simple preparation,easy surface functionalization,and various product forms,including gold nanospheres,gold nanorods,gold nanoshells,and gold nanoclusters [82,83].AuNPs can form several types of dendrimers with different sizes,which can directly wrap around or covalently link to lipophilic antineoplastics [84-86].Francoisetal.developed functional pegylated AuNPs for delivery of the chemotherapeutic drug DOC to treat colorectal cancer [87].Invitro,this system showed remarkable toxicity to human colon carcinoma (HCT15)cells and a lower half maximal inhibitory concentration (IC50)value compared with intravenously injected free DOC.Another research tested against colorectal cancer cells is CPT which has been silica-installed and encapsulated.For instance,CPT-loaded siRNP(CPT@siRNP) for delivery to colorectal cancer was successfully prepared by dissolving PEG-b-siPMNT (60 mg/mL) and CPT (3 mg) in dimethylformamide (DMF) [88].The drug loading capacity and encapsulation efficiency were 2.5% and 51.1%,respectively,and the solubility of CPT was significantly improved.Silica nanoparticles carrying CPT (SNP-CPT) were designed by Botellaetal.with extremely small silica nanoparticles,and the medication was joined by an ester linkage at the 20-OH moiety to avoid nonspecific release of the drug.This system showed good stability under physiological conditions and at pH values lower than 8 [89].According to findingsinvivo,SNP-CPT treatment dramatically decreased the systemic toxicity linked to CPT in HT-29 colorectal cancer xenograft mice while delaying the formation of subcutaneous tumors.Recently,it was discovered that CPT combined with cyclodextrin and iron nanoparticles (Fe3O4) and then cross-linked with ethylenediaminetetraacetic acid (EDTA) might effectively cause apoptosis in the human colon cancer cell line [90].
3.Drug delivery systems for targeted delivery
Although pegylation can prolong the stay of nanoparticles in the bloodstream,the number of drug particles reaching disease targets such as tumors is still very limited.By taking advantage of the receptors overexpressed in colorectal cancer tumor cells or tumor vessels,specific ligands can be used to modify the surface of the nanodrug carrier to improve the proportion of the nanodrug that reaches the target site [91-93].On the other hand,guiding the drug carrier to the tumor tissue by an environmental stimulus can trigger drug release from the nanomaterial drug carrier[94,95].Table 1 summarizes some representative studies on targeted DDS.Here,we also divided the active targeting strategies of colorectal cancer into the ligand-receptor binding type,environmental stimulus-responsive type,and bifunctional type,which described the research status of colorectal drug delivery systems for targeted drug delivery.

Table 1Different types of actively targeted nanoparticles for the treatment of colorectal cancer.
3.1. Ligand-receptor binding DDS
Modification with different types of ligands on the surface of a carrier,including peptides,growth factors,folic acid (FA),etc.,can allow specific recognition of the receptors on cancer cells and promote the delivery of drugs to the target site [111,112].In many cases,liposomes and nanoparticles are modified with peptides to improve the targeted efficiency of the drug [113].Leptin is a 16 kDa glycopeptide and hormone secreted by adipose tissue that is crucial in regulating the behavior and metabolism of adipose tissue and can bind to leptin receptor (Ob-R) which is overexpressed in colorectal cancer [114-116].For instance,Shahrakiet al.used a leptin-derived peptide (Lp31) to modify PEGylated liposomal doxorubicin (PLD,CaelyxR○) as the carrier to deliver doxorubicin (DOX) [117].Interestingly,Lp31-Caelyx had more potent cytotoxicity in and cell uptake by CT26 colon cancer cells than Caelyx,which greatly slowed tumor growth and increased mouse survival.Many principles have also been studied for combination chemotherapy.Wuetal.designed targeting peptide pHCT74-conjugated liposomal DOX formulation (pHCT74-LD) and targeting peptide pHCT74-conjugated liposomal vinorelbine formulation(pHCT74-sLV) targeting theα-enolase protein that had the potential for targeted delivery in colorectal cancer chemotherapy [118].At 24 h,tumor accumulation in the mice in the pHCT74-LD group was 1.95 times higher than that in the LD group,while the tumor DOX AUC0-72(0-72 h area under the plasma concentrationtime curve) in pHCT74-LD mice was 1.85 times higher than that in the LD AUC0-72group.
Similar to liposomes modified by peptides,peptide-modified nanoparticles have also been widely reported over the years.cRGD-decorated biodegradable polytyrosine nanoparticles (cRGDPTN) were studied by Guetal.and were found to have several advantages over conventional nanoparticles [119].As shown in Fig.3,the authors concluded that there was a cRGD-PTN with an ultrahigh DOX content and drug loading values between 18.5 wt%and 54.1 wt%,contributing to anti-colorectal cancer activity that was several times higher than that of the nontargeted DOX-loaded polytyrosine nanoparticle (PTNDOX) and clinically used adriamycin liposomes.Tumor cell drug resistance has always been a significant obstacle in colorectal cancer treatment,as it results in poor efficacy.Due to the rapid increase in angiogenesis in tumor cells and the curling and dilation of blood vessels,antiangiogenesis strategies have become essential in treating cancer and can potentially reduce tumor drug resistance significantly [120,121].Two reports on peptide-modified nanoparticles showed how effective the nanoparticles were in overcoming the problem of drug resistance in colorectal cancer tumor cells.As shown in Fig.4,the TCP1-CDQD nanocarrier (adamantane (ADA)-modified TCP1 peptide binding toβ-cyclodextrin (CD),which was used to modify the surface of quantum dots (QDs) loaded with microRNA-34a mimics (miR-34a(m)) and 5-fluorouracil (5-FU) slowed the development of tumors in xenograft tumor models derived from colorectal cancer cells [122].The other nanocarrier was composed of K237 peptideconjugated PTX-loaded nanoparticles (K237-PTX-NPs) with anticancer efficacy and antiangiogenic effects that targeted the highly expressed kinase insert domain receptors (KDRs) in tumor blood vessels [123].In this study,K237-PTX-NPs increased drug accumulation in HCT15 tumor cells,and the anticancer efficacy was closely related to improved antiangiogenesis effects.

Fig.3.Schematic diagram of cRGD-decorated polytyrosine nanoparticles (cRGDPTN) for effective delivery of DOX to a mouse model of HCT-116 colorectal carcinoma.Copied with permission [119].Copyright 2019,Elsevier.

Fig.4.Host-guest self-assembled nanocarriers designed for the synergistic treatment of colorectal cancer using CD-functionalized QDs (CD-QDs) and the ADAfunctionalized targeting peptide (TCP1 peptide-PEG-ADA) in conjunction with chemotherapy drugs (5-FU),as well as nucleotide therapeutics (miRNA-34a mimics).Copied with permission [122].Copyright 2021,Ivyspring International Publisher.
In addition to modifying a carrier with peptides,growth factors have also been exploited as excellent ligands.Chenetal.designed hollow mesoporous silica nanoparticles (HMSNs) with an average particle size of 120 nm and a surface modified by grafting epidermal growth factor (EGF) [124].The 5-FU-loaded EGF-grafted HMSNs (EGF-HMSNS-5-FU) restored the sensitivity of highly epidermal growth factor receptor-expressing (EGFR-expressing) drug-resistant colorectal cancer cells to 5-FU,and the use of this nanomaterial is expected to become a new strategy for reversing colorectal cancer resistanceinvivo.Additionally,research on PLGA nanoparticles modified with EGF and loaded with 5-FU and perfluorocarbon(PFC) was reported by Wuetal.[125].To explore the targeting capacity of EGF-PLGA@5Fu/PFC nanoparticles,SW620 colorectal cancer cells pretreated with a high concentration of EGF (100 μg/mL)were incubated with EGF-PLGA@5Fu/PFC nanoparticles for 1 day.Analysis of the results indicated that EGF-PLGA@5Fu/PFC nanoparticles effectively enhanced cellular uptake through endocytosis mediated by the EGF receptor,and their binding efficiency was associated with higher levels of EGFR expression.
Finally,several other ligands can be used to improve the targeting of drugs,including FA,β-galactosidase (β-gal),and oligonucleotides with an aptamer (Apt) sequence.Hashemzadehetal.developed an oxaliplatin (OXA) delivery system based on FA coordination to treat colorectal cancer [126].They carried out MTT and cell migration assays to explore the ability of FA-functionalized UIO-66-NH2metal-organic framework (MOF) materials against colorectal cancer cells as an active drug transport system for OXA.This OXA delivery system showed good receptor-specific targeting to restrain the growth of CT-26 spheroids.β-Galactase can target asialoglycoprotein (ASGP) receptors,helping to deliver chemotherapy drugs to tumor cells [127].Forβ-galactosidase (β-gal),new research from Sharmaetal.reported on Gal-DOX with significant tumor-specific targeting to treat colorectal cancer.Gal-DOX might deliver DOX to the site of the tumor and be a potential therapeutic system for colorectal cancer [128].For oligonucleotides with an PrPCaptamer (PrPC-Apt) sequence,the first drug delivery system targeting the cellular prion protein (PrPC)viaApt was recently reported [129].These authors synthesized PrPC-Apt-functionalized doxorubicin-oligomer-AuNPs (PrPC-Apt DOA) with an average diameter of 20 nm that decreased the capacity of colorectal cancer cells to form spheres by inhibiting mitochondrial function.These ligand-mediated targeted drugs can accelerate the distribution and penetration of nanomedicines into tumor tissue,serving as effective drugs for treating colorectal cancer due to their specificity.
3.2. Environmental stimulus-responsive
Currently,a nanodrug delivery system combined with changes in the environment can achieve accurate tumor targeting [130,131].According to the different stimuli that trigger a response,DDS can be divided into those that are responsive to intrinsic and extrinsic stimuli (Fig.5).Intrinsic stimulation mainly refers to factors such as the pH value,redox potential,enzyme concentration,and GSH concentration in the environment inside tumor cells,while extrinsic stimulation mainly includes changes in temperature,magnetic field,and light.The tumor microenvironment (TME) significantly impacts the development and metastasis of tumors.Many inflammatory-related factors,such as interleukin-6 (IL-6),IL-10,and transforming growth factor-β(TGF-β) promote the occurrence and development of malignant tumor cells [132,133].Because the TME is so complicated,drugs mainly stay in the matrix near the tumor blood vessels after arriving at the tumor site,which makes it challenging to access the deep region of the tumor,resulting in poor therapeutic effects.The TME and intracellular signals from tumor cells can activate nanocarriers that release the delivered drugs into the tumor site.However,many studies have been devoted to constructing a variety of stimulus-responsive by using the characteristic signals of the TME as stimuli,which can achieve targeted drug delivery at the tumor site [134-136].This section primarily discusses the progress of stimulus-responsive DDS for colorectal cancer chemotherapy.

Fig.5.Schematic illustration of different environmental stimulus-responsive DDS,including intrinsic stimuli response and extrinsic stimuli response.
3.2.1.pHresponsive
The main reason for the difference in pH between tumor cells and normal cells is the unlimited proliferation of tumor cells,in which irregular angiogenesis leads to a rapid lack of nutrients and oxygen at the tumor site [137-139].Therefore,tumor tissue often undergoes anaerobic respiration under hypoxic or anaerobic conditions;thus,acid metabolites accumulate in the tumor interstitium,and the pH of the tumor extracellular environment is reduced to 6.5 to 7.0 [140].Because the pH in cancer tissue varies significantly compared to that in normal tissue,the slightly acidic nature of tumors is often used as a stimulus source for responsive DDS.Hossainetal.were the first to fabricate a novel pH-sensitive carbonate apatite material that responds to the instability in pH in the TME that was used for the responsive delivery of DOX to colorectal cancer cells [141].After the pH-sensitive carbonate apatite-DOX complex arrived at the tumor siteviapassive targeting,the apatite carbonate dissolved in the cell body in response to the acidic environment of the lysosomal body,thereby rapidly releasing DOX into the cytoplasm.The results demonstrated that carbonate apatite-DOX had more potent antitumor activity than free DOX in an HCT116 colorectal tumor-bearing BALB/c nude mouse mode.
3.2.2.Enzymeresponsive
Many enzymes in the tumor tissue microenvironment play an essential role in tumor growth,invasion and metastasis,of which the concentration and activity of the enzymes are significantly greater than those in healthy tissues.Using these upregulated enzymes at tumor sites as targets for tumor therapy to develop enzyme-responsive nanodrug carrier systems for anticancer drug delivery is a new research direction for DDS [142].Matrix metalloproteinases (MMP) belong to the family of zinc-dependent endopeptidases,which are the most common significantly expressed enzymes in the TME.In particular,MMP-2 and MMP-9 are positively associated with colorectal cancer metastasis,invasion,and angiogenesis [143,144].A novel MMP-2-responsive nanocarrier was constructed by encapsulating hydrophobic agents (CPT and sorafenib) into a polyethylene glycol-peptide diblock copolymer(PPDC) [145].The researchers found that the peptides of the drugcontaining nanoparticles could be digested by overexpressed MMP-2 after exposure to the colorectal cancer microenvironment,enabling controlled release of the payload at the tumor site.In addition,high concentrations of certain enzymes in tumor tissues,such as esterase,can also be used to design enzyme-responsive polymer nanosystems.Wangetal.designed an intracellular esteraseactivatable nanoparticle for stable drug delivery,which acted as a practical and effective platform against colorectal cancer [146].Overall,these results demonstrated that the nanoparticles slowly released the drug under the action of esterases,resulting in persistent tumor regression in various mouse models of colorectal cancer.
3.2.3.ROSresponsive
ROS is a general term for oxygen and oxygenated and active substances produced by organisms during aerobic processes,including oxygen ions,peroxides,and oxygen-containing free radicals [147].Under normal physiological conditions,the level of ROS within the cell is balanced,but in tumor cells,the level of ROS in the mitochondria is much higher than that in normal cells[148].Many researchers have constructed ROS-responsive by exploiting this difference in ROS contents,which can control intracellular drug release [149,150].One such nanoparticle (OCD NP)that responds to ROS and eliminates hydrogen peroxide was described by Zhang and coworkers,who built an effective oral delivery method for treating colorectal cancer [151].It involved adding the anticancer medication camptothecin-11 (CPT-11) into the OCD NP.The system selectively released CPT-11 from CPT-11/OCD NP in the cells with high intestinal ROS levels,which reduced inflammation and oxidative stress in the diseased colon of colitisassociated colon cancer mice and showed the safety of oral drug administration (Fig.6).Therefore,normalizing the inflammatory tumor microenvironment is expected to be used for targeted therapy of inflammation-related tumors.Ferrocene is an insoluble organic compound that is also considered a potential ROS-reactive drug carrier material because it can undergo oxidation under high ROS conditions and become hydrophilic cations,thereby releasing drugs [152-154].In a separate study,Naetal.generated carboxylated ferrocene nanocapsules (CFNCs),whose size and sensitivity to reactive oxygen species could be controlled by different polar solvents [155].In this study,CFNCs exposed to H2O2showed a significant increase in the response to ROS with an increasing ethanol ratio from CFNC1 to CFNC5 with an increase in diameter to more than 5000 nm,indicating the strong ROS responsiveness of these CFNCs.
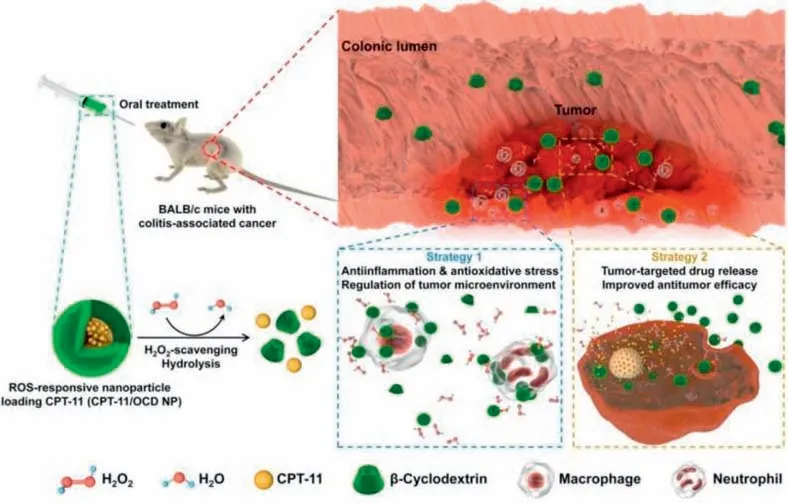
Fig.6.Descriptive research design for a functional targeting nanovehicle that normalizes the inflammatory microenvironment to treat colon cancer linked with colitis.Copied with permission [151].Copyright 2019,Ivyspring International Publisher.
3.2.4.GSHresponsive
In the human body,the amount of GSH is responsible for the difference in intracellular redox potential between tumor tissue and normal tissue.In addition,GSH levels are at least five times greater in tumor tissue than in healthy tissue.Nanocarriers with redox properties can be designed according to the large redox potential difference between the intracellular and extracellular environments and between normal and tumor tissues.Lietal.synthesized HCPT-loaded nanoparticles (HCPT@PT/PHF and HCPT@PT/PSF) using the shell stripping strategy that were triggered by GSH to shield the triphenylphosphonium (TPP)-modified hydroxyl CPT-loaded core [156].These responsive nanoparticles delivered more 10-hydroxycamptothecin to the nuclei and mitochondria of colorectal cancer tumor cells,which had been shown to enhance caspase-3 cleavage activityinvivo.It has been reported that self-assembled BI@PEG-SN38 nanoparticles respond to intratumoral GSH with significantly and specifically increased sensitivity to 7-ethyl-10-hydroxy-camptothecin (SN38) in breast cancer resistance protein (BCRP)-overexpressing human colorectal cancer cells compared to CPT-11 [157].
3.2.5.Magneticfieldresponsive
Using magnetic nanomaterials as drug carriers directed by an external magnetic field causes drugs to reach specific parts of the body to exert efficacy and treat cancer.Magnetic targeting drug delivery systems (MTDDS) for targeted drug delivery to the tumor or diseased tissue under the external stimulation of magnetic fields[158].Invitrocontrol of the magnetic field intensity and targeted transport can improve the concentration of drugs near the targeted lesion,reduce the medication dosage,and decrease the harmful effects of the drug and its side effects on the body’s normal tissues[159].Magnetic field-sensitive nanoparticles often contain iron oxide (IO) nanoparticles,which cause apoptosis of cancer cells under the influence of an applied magnetic field [160,161].The magnetic field and GSH-responsive nanocomposite ChitoPEG/DOX/IO was constructed using methoxypoly(ethylene glycol)-grafted chitosan copolymer (ChitoPEG),which encapsulated drugs such as a DOX prodrug as an example [162].The nanocomposite was an excellent anticancer drug candidate with a particle size of approximately 150 nm and preferentially targeted CT26 colon cancer tissues under the action of an applied magnetic field.
3.3. Dual-functioning DDS
In addition to DDS with a single targeting modality,such as ligand-receptor binding or an environmental response,researchers have also reported some dual-targeted DDS that can bind specifically and respond to environmental stimuli.
First,a drug delivery system that simultaneously responds to the weakly acidic tumor microenvironment and actively targets colorectal cancer cells was introduced.For example,with a particle size of 50 nm and TME pH-responsiveness,Zhangetal.presented PEGylated hyaluronic acid (HA-mPEG2k-DOX) nanoparticle drug delivery system that actively targeted CD44-positive CT26 cells[163].In the mildly acidic environment of tumors,HA-mPEG2k-DOX nanoparticles efficiently removed the PEG hydration layer,promoted the cell uptake of HA-DOX nanoparticles,and helped the nanoparticles escape the lysosomes.The results showed that HAmPEG2k-DOX nanoparticles might greatly lengthen the DOX circulation time by 12.5-fold compared with DOX·HCl,have high tumor resistance and greatly improve the toxic side effects of DOX.
Moreover,a series of redox-responsive DDS based on specific ligand-receptor binding has been studied.Since the amount of GSH present in tumors is higher than that in blood and normal tissues,the disulfide bonds in these redox drug delivery systems are efficiently cleaved by GSH for complete intracellular drug release[164].As shown in Fig.7,Chenetal.created redox-responsive PTX prodrug polymeric micelles that could codeliver PTX and adjudin(ADD) to effectively overcome multidrug resistance in colon cancer patients [165].This combined drug delivery system increased the accumulation of PTX in colorectal cancer cells and exhibited significant inhibition of multidrug-resistant tumors.
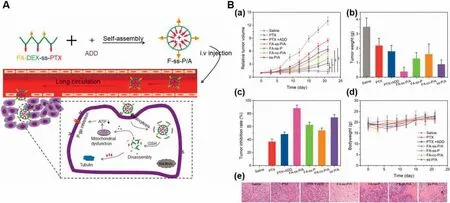
Fig.7.(A) Diagram demonstrating the self-assembly of FA-ss-P/A micelles,intracellular GSH-responsive drug release,colon cancer cell targeting,and overcoming of the multidrug-resistance process.(B) (a) Tumor volumes.(b) Tumor weights when the animals were sacrificed.(c) Rates of tumor inhibition after treatment with various formulations.(d) Body weight changes during therapy.(e) Images of tumor tissues from various drug treatment groups stained with hematoxylin and eosin.Reproduced with permission [165].Copyright 2020,Taylor & Francis.
Finally,except for the dual-targeted drug delivery system based on intrinsic stimulus responses,dual-targeted DDS based on extrinsic stimulus responses,such as ultrasound and magnetic fields,can be designed for colorectal cancer chemotherapy.Microbubbles(MBS) can deliver drugsvialiposomes attached to the shell and be stimulated to control drug release by ultrasound [166,167].Ingrametal.created therapeutic vascular endothelial growth factor receptor 2 (VEGFR2)-targeted microbubbles (thMBs) triggered by ultrasound to extend drug residence in tumor sites in a mouse model of colorectal cancer [168].Their dual-targeted drug delivery system increased the targeting efficiency of irinotecan and SN38 at the tumor site compared with VEGFR2-targeted SN38 liposomes.Graphene is currently considered to be the thinnest material,with a large specific surface area for achieving higher drug loading after being converted into graphene oxide (GO) [169,170].Magnetic graphene oxide (MGO) was designed by chemical coprecipitation and modified with PEG and cetuximab (CET) (MGO-PEG-CET) for DOX delivery in CT-26 tumor-bearing mice [171].The results of confocal imaging and live/dead cell viability staining showed that CT-26 cells had more intracellular uptake of MGO-PEG-CET than MGO-PEG.
4.Drug delivery systems for local drug delivery
An unfortunate problem with systemic chemotherapy is that it produces more toxic side effects,and the concentration of the chemotherapeutic that reaches the tumor location is lower.Compared with systemic administration,local drug administration has many advantages: (1) It can improve the local concentration of the drug and remove residual tumor cells more effectively;(2) The use of specific sustained release preparation technologies can endow the drug with a long-term local effect,reduce the number of drug administrations,and improve patient compliance;(3) It greatly reduces the content of antitumor drugs in the blood circulation and reduces their systemic toxicity;(4) It reaches the patient without passing through a biological barrier [172,173].Numerous local DDS have been developed for colorectal cancer,such as hydrogels,hydrogel/nanoparticle composites,and microspheres,as summarized here.
4.1. Hydrogels
Hydrogels are three-dimensional network structures with swelling properties formed by the covalent cross-linking of natural or synthetic polymers and noncovalent interactions [174,175].The pores formed when the polymers are crosslinked enable both hydrophilic and hydrophobic drugs to be loaded efficiently and stably.Hydrogels can form a drug storage depot in tumor tissues for local drug transport and have a long local retention time to sustain drug release [176,177].This section summarized the research progress of hydrogel-based DDS for colorectal cancer chemotherapy,categorized by polymer classification.
4.1.1.Hydrogelsbasedonnaturalpolymers
Local DDS based on hydrogels can continuously release drugs at the tumor site and have attracted considerable interest in recent years owing to their advantages of good biocompatibility,controllability,strong drug loading capacity and low invasiveness[178,37].Natural polymers benefit from better biocompatibility,environmental sensitivity,low price,and a wide range of sources,among which chitosan,alginate andβ-cyclodextrins are commonly used.Studies have shown that cyclodextrin can be used as a bioactive molecule-functionalized hydrogel that slowly releases the active drug molecule through hydrophobic interactions [179].Fioricaetal.lengthened the release time of loaded DOX by exploiting the azo-type Michael reaction betweenβ-cyclodextrins complexing DOX to form an injectableinsituhydrogel [180].Theinvivotest results revealed that this strategy could boost the expression of caspase 3 (an apoptosis marker) in residual colorectal cancer tumor cells,which holds outstanding promise for the treatment of inoperable solid tumors or the removal of recalcitrant tumor micromasses.
4.1.2.Hydrogelsbasedonsyntheticpolymers
Synthetic polymer hydrogels have good stability,a wide range of synthetic material precursors,and easy functionalization.Schiffbase cross-linked injectable hydrogels were synthesized based on the Schiff base reaction and are biodegradable and self-repairing[181].Wuetal.successfully formulated a Schiff base injectable hydrogel (PFA/PPLL) by a simple condensation reaction for the local and continuous delivery of metformin (ME) and 5-FU for colorectal cancer treatment [178].The tumor suppression rate (TIR) reached a maximum of 95.1% 21 days after injection of the ME/5FU-PFA/PPLL hydrogel into mice with colorectal cancer while reducing side effects (Fig.8).

Fig.8.(A) Schematic representation of the combined anticancer effects of ME and 5FU released from PFA/PPLL hydrogels.(B) C26-inoculated BALB/c mice treated with various formulations in a tumor regression trial.(a) Photos of tumors from mice treated with different formulations after 21 days.(b) Changes in mouse tumor volume over time.(c) Tumor weights at the conclusion of the assessment.(d) Body weight changes of the mice treated with different formulations.Reproduced with permission [178].Copyright 2016,Elsevier.
Peritoneal carcinomatosis (PC) is a common abdominal cancer disease that is mainly caused by the spread of residual tumors in the abdominal cavity during or after surgery [182].Intraperitoneal chemotherapy is effective for colorectal peritoneal carcinomatosis(CRPC),but needs to be enhanced further [183].In one study,a hydrogel (HACPN-DOX) made of poly(N-isopropylacrylamide) rapidly released DOX in phosphate buffer solution (PBS) at pH 7.4 for the first 8 h after preparation [184].As a result,HACPN-DOX nearly doubled the survival rate of mice with CRPC tumors compared to the control and HACPN groups and decreased the possibility of postoperative peritoneal adhesions.Likewise,a biodegradable temperature-sensitive hydrogel made of PEG-PCL-PEG (PECE) triblock copolymer loaded with 5-FU as the chemotherapeutic was prepared [185].The release rate of 5-FU from the PECE hydrogels was 26.2% within 1 h and 82.9% within 1 day,which decreased with increasing initial drug load.Significant delays occurred in the release of methylene blue,which was observed in the bladder for more than 48 h after intraperitoneal injection of methylene blueloaded PECE hydrogels into mice.
4.1.3.Hybridhydrogelsbasedonsyntheticandnaturalpolymers
In addition to natural or synthetic polymer hydrogels,some hydrogels are formed with both synthetic and natural polymers,called hybrid hydrogels.A multipurpose thermosensitive hydrogel was made of poloxamers P407/P188/alginate loaded with 5-FU that can release 5-FU in the area of the tumor for a minimum of three days [186].Simulating drug release from drug-loaded hydrogels in tissue regions by a flow cytometry model found that 50% of the 5-FU in 5-FU-loaded P407/P188 20/2% w/v hydrogels was released within 2.8 h,while 50% was released after 6.6 h in 1% w/v alginate,showing a twofold delay in release.This hydrogel preparation significantly inhibited tumor growth and prevented local recurrence in mice with CT26-luc colorectal cancer subcutaneous tumors and subcutaneous resected tumors.Hydrogels made up of natural and synthetic polymers have a three-dimensional polymer network structure with strong water absorption and high viscosity,which can be used to prevent adhesion after surgery.In a similar study,OXA was loaded into cross-linked hydrogels based on hyaluronic acid and carboxymethyl cellulose sodium (CMCNa),named HC hydrogels,to assess its potential for treating colorectal cancer and preventing postoperative abdominal adhesions [187].The research results demonstrated that the HC hydrogels degraded slowlyinvitroand exhibited a better anti-adhesion effect than the control group.
4.2. Nanocomposite hydrogels
Nanomaterials have unique micro-scale structures and properties,showing great potential in electronics,optics,mechanics,biology,and other fields.To enhance the efficiency of hydrogels,all kinds of new hydrogels have been developed,among which nanocomposite hydrogels have better mechanical properties and biocompatibility [188,189].This section reviewed the applications of nanocomposite hydrogels in colorectal cancer chemotherapy by introducing different nanounits into hydrogels.
4.2.1.Micelle/hydrogelcomposites
Notably,researchers have found that hydrogel composite systems can encapsulate micelles into a temperature-sensitive hydrogel that combines thermosensitive and sustained-release characteristics,significantly improving the effect of chemotherapy in CRPC mouse models.PTX micelles were loaded with a 5-FU-loaded thermosensitive poly(ε-caprolactone)-poly(ethylene glycol)-poly(ε-caprolactone) (PCEC) hydrogel,which was proven to improve the antimetastatic effects of colorectal peritoneal carcinomatosisinvivoand displayed exceptional cooperation [190].Additionally,invivostudies of mice with CT26 colorectal peritoneal carcinomatosis showed that the PTX-micelle-Fu-hydrogel could significantly increase the duration of action and levels of PTX and 5-FU in the peritoneal fluids in contrast to the other groups,demonstrating the great effectiveness and value of combination therapy in clinical care.
Another novel dual drug delivery system combining a 5-FU polymeric micelle (PECE) with cisplatin (DDP) in biodegradable thermosensitive chitosan hydrogels was designed for the inhibition of colorectal peritoneal carcinomatosis [191].Compared with free 5-FU and 5-FU micelles,the cumulative release rate of 5-FU from the chitosan hydrogel was lower,indicating the potential applicability for delayed drug release.In addition,the CRPC mice in the chitosan hydrogel group had a considerably longer median survival time (43 days) than the mice in the control group(25 days).
4.2.2.Polymernanoparticle/hydrogelcomposites
Hydrogels made from natural or synthetic polymers can embed nanoparticles to form nanocomposite hydrogels,which can improve upon the properties of traditional hydrogels and expand their applications to biomedical disciplines such as drug delivery,tumor therapy,and tissue engineering [192].Moreover,local administration of the hydrogel can also provide more formulations for nanoparticles and improve the administration limitations of nanoparticles.
To enhance the effectiveness of colorectal cancer treatment by codelivering OXA and tannic acid (TA),aninsituthermosensitive hydrogel (OXA/TA NPs-h) was developed by physically incorporating OXA and TA coloaded nanoparticles (OXA/TA NPs) into a poly(ε-caprolactone) (PCL)-10R5-PCL (PCLR) thermosensitive hydrogel (Fig.9) [193].OXA and TA were released from the hydrogel in a sustained manner,demonstrating that the hydrogel could delay the release of the drugs and continuously maintain effective drug concentrations in colorectal cancer cells.This research also indicated that the median survival (38 days) in the OXA/TA NPsh group was significantly longer than that in the other groups.In addition,Fanetal.coembedded DOC and LL37 peptide polymeric nanoparticles (DOC+LL37 NPs) into a PLA-L64-PLA hydrogel to make DOC+LL37 NP-hydrogel composites [194].The number of tumor nodules and sizes of the tumors in mice with peritoneal carcinomatosis showed the higher cancer-killing efficiency and longer survival of the DOC+LL37 NP-hydrogel-treated mice than the mice in the other groups.
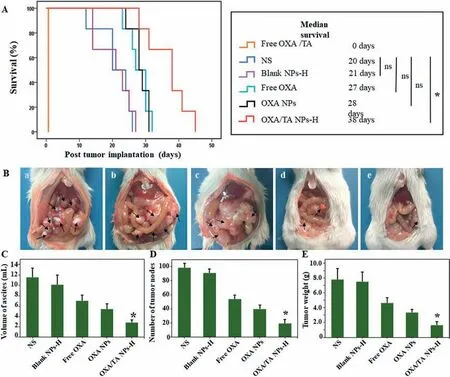
Fig.9.Antitumor effect of OXA/TA NPs-H on CT26 colorectal cancer mice.(A) Survival curves of mice administered different treatments.(B) Typical images of tumors from various groups.(a) NS.(b) Blank NPs-H.(c) Free OXA.(d) OXA NPs (e) OXA/TA NPs-H.(C-E) Volumes of ascites,numbers of tumor nodules and weights of the tumors in mice treated with different formulations at the conclusion of the assessment.Copied with permission [193].Copyright 2019,Elsevier.
4.2.3.Inorganicnanoparticle/hydrogelcomposites
Researchers have tried to composite inorganic nanoparticles into the polymer network structure of hydrogel to improve the mechanical properties and other properties of the hydrogels[195-197].One-dimensional nanostructured materials with high aspect ratios,such as nanotubes and cellulose nanocrystals,have excellent properties.To improve the efficacy of cyclic dinucleotides(CDNs),Wangetal.created a self-assembled hydrogel by complexing the negatively charged STING agonist c-di-AMP (CDA) and supramolecular nanotubes (NTs) loaded with CPT and the hydrophilic polypeptide iRGD [198].This study demonstrated that the CDA-NT hydrogel enabled colorectal cancer model mice to have long immune memory and prevented tumor recurrence and metastasis.Although the polyacrylic acid (PAA) in synthetic adhesion hydrogels was easily washed away by biological fluids,studies showed that cellulose nanocrystals (CNC) could enhance their mechanical stability and improve their adhesion capacity [199].In one study,a mucoadhesive hydrogel with excellent performance was prepared to load cisplatin (CDDP).PAA at different ratios was grafted onto the CNC surface,which was used to load CDDP for the local treatment of colorectal cancer [200].It was found that the PAA/CNC ratio was inversely correlated with CDDP release,because CDDP tended to bind to the PAA chain rather than to the CNC.
In addition to one-dimensional tubular nanomaterials,spherical inorganic nanomaterials are another type of nanomaterial with a relatively mature preparation process [201-203].Among them,potent AuNPs may increase secondary radiation emission under X-ray irradiation,so they are very suitable for use as a reinforcing material for hydrogels.Mirrahimietal.developed a nanocomplex,abbreviated as ACA,for colorectal cancer chemoradiotherapy,which was fabricated by coloading cisplatin and AuNPs into an alginate hydrogel system [204].The transmission electron microscopy images of the ACA nanocomplexes with hydrodynamic diameters of 20-80 nm showed that they were spherical in shape and that the alginate hydrogel evenly covered the AuNPs,which could also increase the anticancer activity to 95% compared to the control group (P<0.001) by the combination of chemotherapyradiotherapy in CT26 colorectal cancer tumor-bearing mice.
4.3. Microspheres
One of the advantages of microsphere formulations is that the drug can be dispersed more evenly in the polymer matrix,which plays a significant role in treating various diseases [205].Surprisingly,local injection of drug-loaded microspheres can prolong drug retention at the colorectal cancer tumor site,thereby improving the effectiveness of drug treatment.
PCL-PEG-PCL (PCEC) copolymers can be assembled into hydrogels or microspheres.Daietal.designed an effective local delivery system based on PCEC microspheres by the oil-in-water emulsion solvent evaporation method to prolong the release of CPT [206].Compared with the 80% sudden release of free CPT,the initial release of CPT from the PCEC microspheres (CPT-PCEC MSs) was only 18%,and the drug was continuously released for 15 days.Moreover,the CPT-PCEC MSs group showed increased tumor growth inhibition compared to the control groups.The survival rate in the CPT-PCEC MS group was 40%,while that in the free CPT group was 20% in the CT26 colon carcinoma peritoneal carcinomatosis mode.In another work,Fanetal.synthesized DOC-loaded PLLAL121-PLLA porous microspheres (DOC-MS) for local drug delivery for peritoneal colon cancer therapy [207].The immunohistochemical staining images showed that the immune response to Ki-67 in the DOC-MS treatment group was weaker than that in the free DOC group,blank MS group,and saline group.
Polyvinyl alcohol (PVA) microspheres loaded with DOX and MoS2(PVA/MoS2/DOX microspheres) had a superior light-to-heat conversion of 23.2% and were bifunctional microspheres for combination photothermal therapy and chemotherapy [208].After the administration of PVA/MoS2/DOX microspheres to the tumor site in HT29 colorectal cancer-bearing mice,30 s of irradiation with nearinfrared light at a wavelength of 808 nm was performed,and the temperature of the tumor site increased by 9.5 °C.In this study,the particle size and drug loading of the cross-linked PVA/MoS2/DOX microspheres were 744.0±261.1 nm and 5.13%,respectively,and the microspheres showed slow drug release and were sensitive to changes in temperature and pH.
5.Conclusion and outlook
Colorectal cancer is the third most common cancer and the second leading cause of cancer deaths worldwide,posing a severe threat to human health.The poor water solubility of some chemotherapeutics and the nontargeted delivery and severe toxic side effects of many conventional treatments affect the efficacy of colorectal cancer chemotherapy.Therefore,numerous DDS have been developed to enhance the efficacy of chemotherapeutics while reducing systemic toxicity [209].Here,we described several nanocarriers that have been used to improve the water solubility of chemotherapeutics,including liposomes,micelles,and nanoparticles,which can also deliver two or more chemotherapeutics more efficiently.Next,we summarized targeted DDS based on specific ligand-receptor recognition and TME stimulus-response.It can be seen that through the interaction between surface-coupled antibodies or ligands and target cell membrane receptors,DDS for colorectal cancer can increase the concentration of drugs in the target cells and reduce adverse drug reactions.Moreover,DDS triggered by hypoxia,weak acidity,abnormally expressed proteases in the TME and external environmental stimuli leads to the release of drugs at specific sites in a more controlled way;namely,to achieve activation by environmental stimuli,self-regulation,comprehensive perception and monitoring.Finally,we reviewed local DDS based on hydrogels and microspheres to increase local drug concentrations,prolong the drug residence time,and reduce systemic toxicity compared with systemic administration.These new technologies and therapies have essential clinical implications for improving the prognosis of colorectal cancer patients.
Nonetheless,the clinical application of emerging DDS is still limited to some extent.First,due to the complex internal environment of the human body and the heterogeneity of different tumor cell lines,the colorectal cancer tumor cell lines used in the abovementioned models generate an incomplete comparison of varying research results.In addition,since DDS are still in the stage of research as an emerging research field and their safety,specificity,targeting,and many other issues have not yet been clarified,there are very few nanodrugs used in clinical practice.
Overall,colorectal cancer drug delivery strategies may significantly improve the clinical efficacy of colorectal cancer chemotherapy.This trend suggests that future work should also strive for developing advanced DDS and trialing new formulations in the clinic.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We gratefully acknowledge financial support from the National Natural Science Foundation of China (Nos.U21A20417,31930067,and 31800797),the Sichuan Science and Technology Program(Nos.2022YFS0333 and 2022YFS0203),the 1·3·5 project for disciplines of excellence,West China Hospital,Sichuan University (No.ZYGD18002),and the Post-Doctor Research Project,West China Hospital,Sichuan University (No.2018HXBH066).We also acknowledge BioRender for contributing to the creation of Figs.1 and 5 (BioRender.com).
 Chinese Chemical Letters2024年2期
Chinese Chemical Letters2024年2期
- Chinese Chemical Letters的其它文章
- The 3rd Xihua Chemistry and Biomedicine Forum
- Professor Hualiang Jiang: A tribute to an esteemed visionary chemist and pharmacist
- Recent advances in visible light-mediated chemical transformations of enaminones
- Development of porphyrin-based fluorescent sensors and sensor arrays for saccharide recognition
- Recent advances of versatile reagents as controllable building blocks in organic synthesis
- Synthetic host-guest pairs as novel bioorthogonal tools for pre-targeting☆
