Successful hepatic resection for recurrent hepatocellular carcinoma after lenvatinib treatment: A case report
Hideki Yokoo, Hiroyuki Takahashi, Masahiro Hagiwara, Hiroyoshi Iwata, Koji Imai, Yoshinori Saito, Naoto Matsuno, Hiroyuki Furukawa
Hideki Yokoo, Hiroyuki Takahashi, Masahiro Hagiwara, Hiroyoshi Iwata, Koji Imai, Naoto Matsuno, Hiroyuki Furukawa, Division of Hepato-Biliary-Pancreatic Surgery and Transplant Surgery, Department of Surgery, Asahikawa Medical University, Asahikawa 078-8510, Hokkaido, Japan
Yoshinori Saito, Department of Gastroenterology, Asahikawa-Kosei General Hospital, Asahikawa 078-8211, Hokkaido, Japan
Abstract
Key Words: Conversion to surgery; Lenvatinib; Recurrent hepatocellular carcinoma; Case report; Neoadjuvant therapy; Molecular targeted therapy
INTRODUCTION
The treatment strategy for hepatocellular carcinoma (HCC) has been established in various guidelines, including the Clinical Practice Guidelines for Hepatocellular Carcinoma in Japan[1], Barcelona Clinic Liver Cancer Guidelines[2], American Association for the Study of the Liver Diseases Guidelines[3], and European Association for the Study of the Liver European Organization for Research and Treatment of Cancer Guidelines[4].Hepatectomy is a potential curative treatment for early-stage HCC.However, the indications for liver resection are limited by tumor progression and liver function, and many cases are not eligible for resection.Transarterial chemoembolization(TACE) is commonly used for these unresectable cases, but the outcomes, especially of chemotherapy, have not been satisfactory compared with liver resection until recently[5,6].
Against this background, the systemic chemotherapy landscape for HCC changed more than a decade ago, with sorafenib demonstrating a survival benefit in the firstline setting and becoming the first systemic therapy to receive approval for HCC.More recently, regorafenib and ramucirumab have been approved in the second-line setting after sorafenib, and lenvatinib has emerged in the first-line setting after a positive phase 3 study[7-11].The advent of these effective molecular targeted agents has allowed multidisciplinary treatments combined with chemotherapy and liver resection for HCC.
Regarding colorectal cancer, there are many reports on postoperative adjuvant therapy to prevent recurrence after resection and preoperative neoadjuvant chemotherapy for colorectal cancer and its liver metastases[12-15].Thus, conversion therapy in colorectal cancer has become a routine practice.Although conversion therapy for HCC has not yet been established, lenvatinib is expected to be a possible candidate agent because it exhibited a tumor-reducing effect in 40% of cases in the REFLECT study[14].There is a possibility that patients with unresectable or recurrent HCC can be converted to surgery after lenvatinib treatment.In the present case, lenvatinib induced a partial response (PR) for rapid growth of recurrent HCC with bone metastases, and conversion to surgery was successfully achieved for the purpose of controlling the intrahepatic lesion.
CASE PRESENTATION
Chief complaints
The patient complained of general malaise.
History of present illness
A 69-year-old man was referred to our facility with a diagnosis of recurrent HCC.He had undergone right anterior sectionectomy for two tumors in segment 8 at another hospital 10 mo previously.The pathological diagnosis of the two tumors was moderately differentiated HCC and poorly differentiated HCC, respectively, without vascular invasion.The pathological stage was stage III according to the Union for International Cancer Control 8thedition.
History of past illness
The patient had undergone appendectomy for appendicitis at 27 years of age.
Personal and family history
The patient’s father had experienced lung cancer, and his sister had suffered from breast cancer.
我国西南边疆民族地区就是典型的“老少边山穷”地区,这里贫困面广、贫困程度深,要打赢这场扶贫攻坚战,党的正确领导是坚实的后盾,边疆民族地区群众对党的扶贫政策的了解和认可是前提,边疆民族地区脱贫攻坚的意识和决心是保障。因此,除了物质、资金、技术上的扶持,还需加大思想宣传和文化建设力度,增强边疆民族地区群众对扶贫政策的了解和认可,提高他们的思想文化素质和脱贫攻坚意识,从而才能凝心聚力,团结边疆民族群众打赢这场扶贫攻坚战。
Physical examination
On physical examination, the patient had a temperature of 36.6 °C, heart rate of 76 bpm, respiratory rate of 16 breaths/min, blood pressure of 143/86 mmHg, and oxygen saturation in room air of 98%.The patient’s weight was 59 kg.He had no jaundice or anemia in the bulbar conjunctiva.There was an operative scar for an inverted Lshaped incision on the abdomen from the previous liver resection.No ascites and encephalopathy were detected.
Laboratory examinations
The preoperative liver functional reserve was good.Laboratory data revealed serum albumin of 3.5 g/dL, total bilirubin of 0.9 mg/dL, prothrombin time of 93%, and indocyanine green retention rate at 15 min of 5.2%.The Child–Pugh score/ classification was 5/A and the albumin-bilirubin (ALBI) score/modified ALBI grade was -2.19/2b.The alpha fetoprotein value was within the normal range, while the protein-induced vitamin K absence or antagonist II value was elevated at 998 mAU/mL.
Imaging examinations
A computed tomography scan of the abdomen demonstrated a heterogeneous contrast-enhanced mass of 10 cm in size in segment 7, which had rapidly increased in 5 mo (Figure 1A and 1B).The magnetic resonance imaging (MRI) images at 5 mo before the second operation are shown in Figure 2 (A: T1 image; B: T2 image).There was no evidence of the recurrent tumor on these MRI images.A positron emission tomography examination showed elevated standardized uptake volume in the sternum and slight uptake in the liver (Figure 3A and 3B).The patient was diagnosed as recurrent HCC in segment 7 of the liver with metastasis in the sternum.
MULTIDISCIPLINARY EXPERT CONSULTATION
Yoshinori Saito, MD, PhD, Chief, Department of Gastroenterology, Asahikawa-Kosei General Hospital
As a treatment strategy, we should administer lenvatinib at a dose of 8 mg because the patient weighed less than 60 kg to suppress the rapidly increasing intrahepatic lesion, and if the intrahepatic lesion exhibited shrinkage, we should surgically remove the lesion.The reason for choosing lenvatinib was that in addition to the intrahepatic recurrence, there was a sternal metastasis.Therefore, we considered that systemic therapy would be better than transcatheter therapy, such as B-TACE.The reason for not choosing surgical resection without prior lenvatinib was that the site of recurrence was rapidly increasing, and it was thought that new lesions might appear in other parts of the liver immediately after surgical resection.In addition, after surgical treatment, we should perform postoperative radiation therapy and treatment using molecular targeted drugs for the metastatic bone lesions.
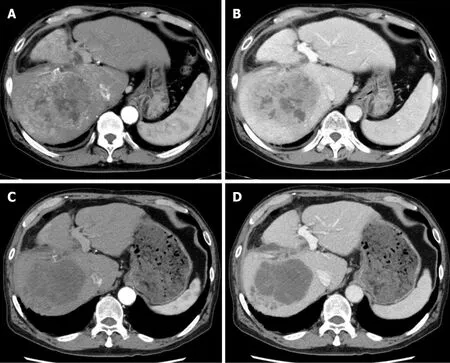
Figure 1 Preoperative computed tomography findings.
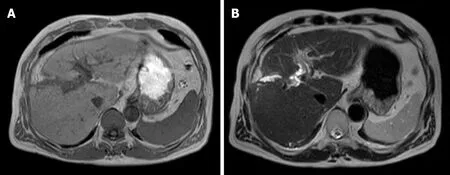
Figure 2 Magnetic resonance imaging findings at 5 mo before the second operation.
FINAL DIAGNOSIS
Computed tomography imaging after 1 mo of lenvatinib administration revealed that 90% of the tumor had lost the contrast effect.The response evaluation was PR, though close to complete response by the modified Response Evaluation Criteria in Solid Tumors[16](Figure 1C and 1D).Protein-induced vitamin K absence or antagonist II decreased to 434 mAU/mL at 2 mo after the treatment (Figure 4).
TREATMENT
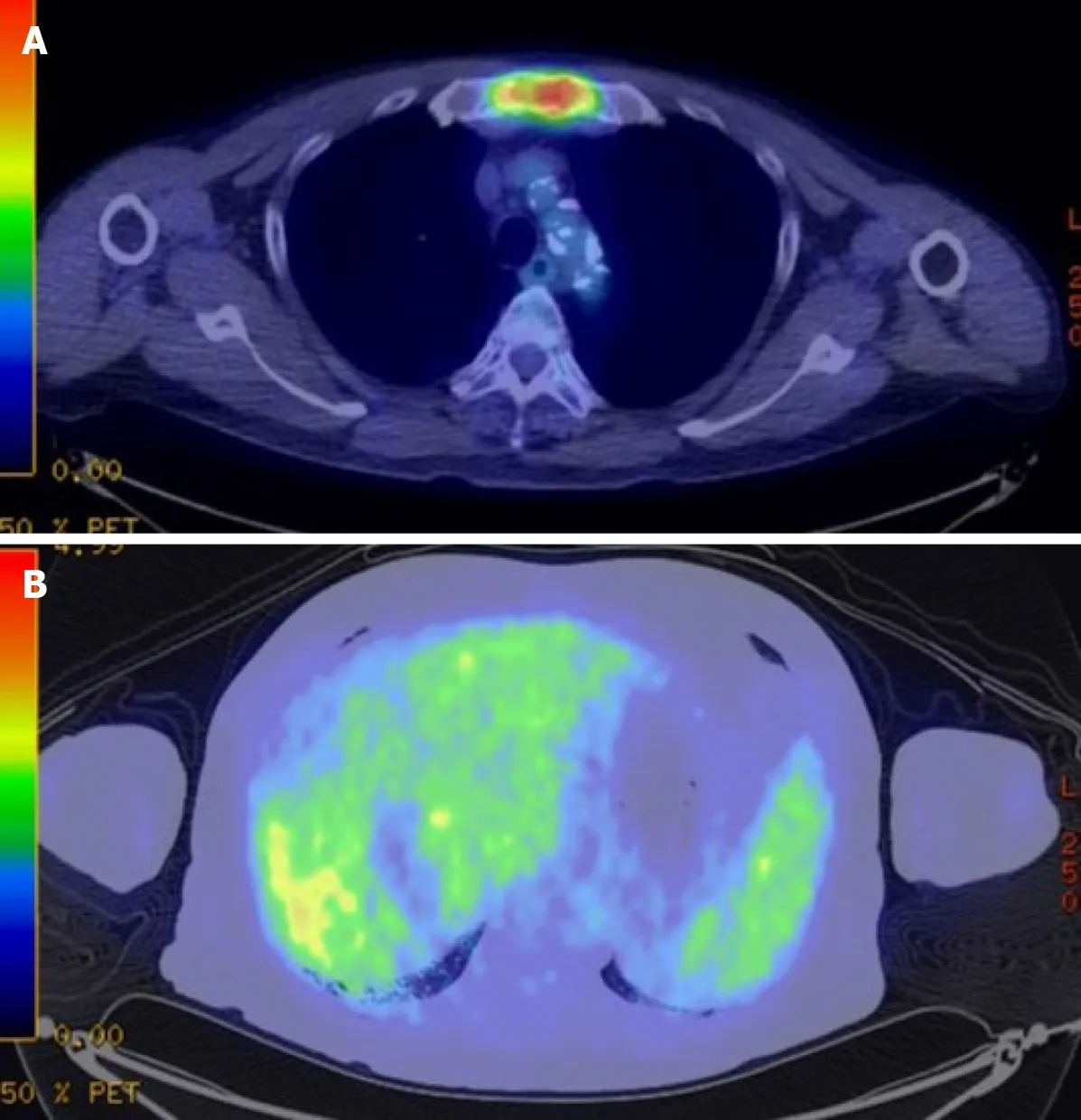
Figure 3 Preoperative fluorodeoxyglucose-positron emission tomography-computed tomography.
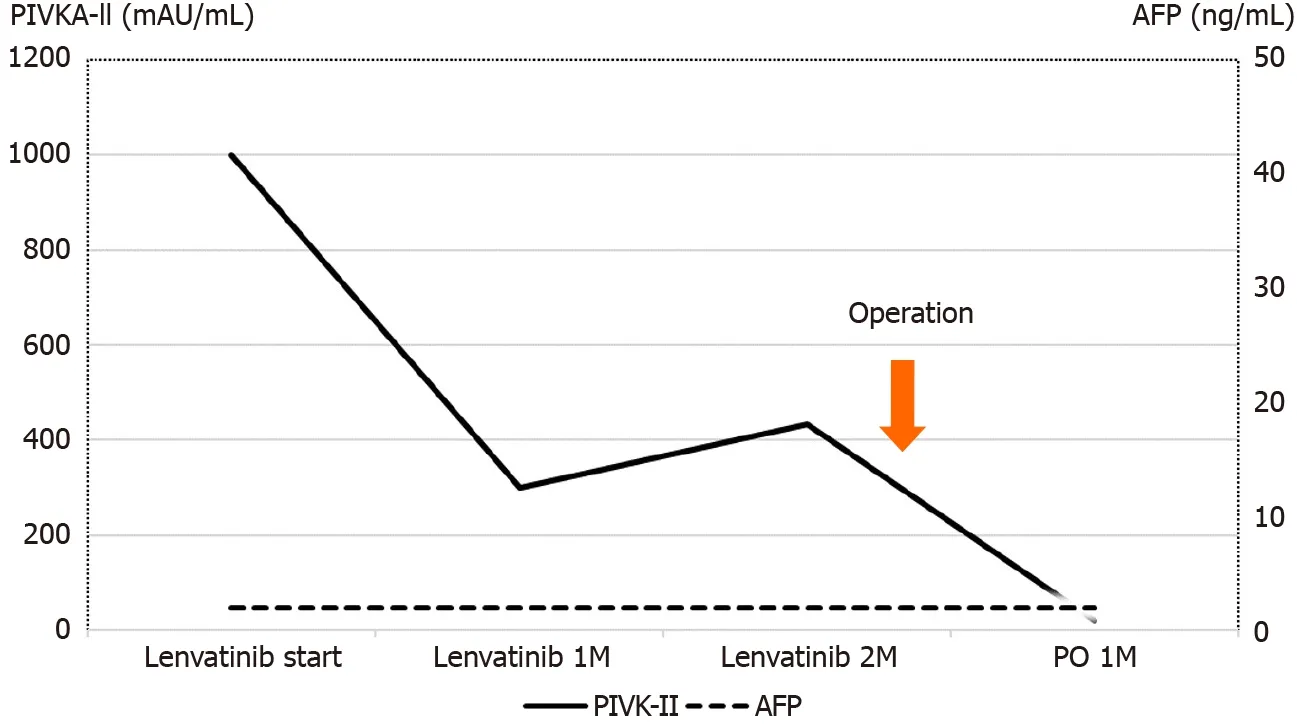
Figure 4 Perioperative tumor marker changes.
Because the intrahepatic recurrent tumor was reduced by administration of lenvatinib, hepatectomy of segment 7 was performed, with blood loss of 3913 mL and operation time of 545 min.Segments 5 and 6 were successfully preserved without bile duct injury (Figure 5).Histopathological findings showed that 80% of the tumor was necrotic, and the resected margin of the liver had no cancer component (Figure 6).The reason for choosing surgical resection after lenvatinib was that long-term administration of lenvatinib may result in decreased liver function such as decreased albumin, which can make surgery impossible.Early surgery was selected because it was unknown whether lenvatinib would result in a complete response, and it was better to aim for complete removal of the tumor by surgery.
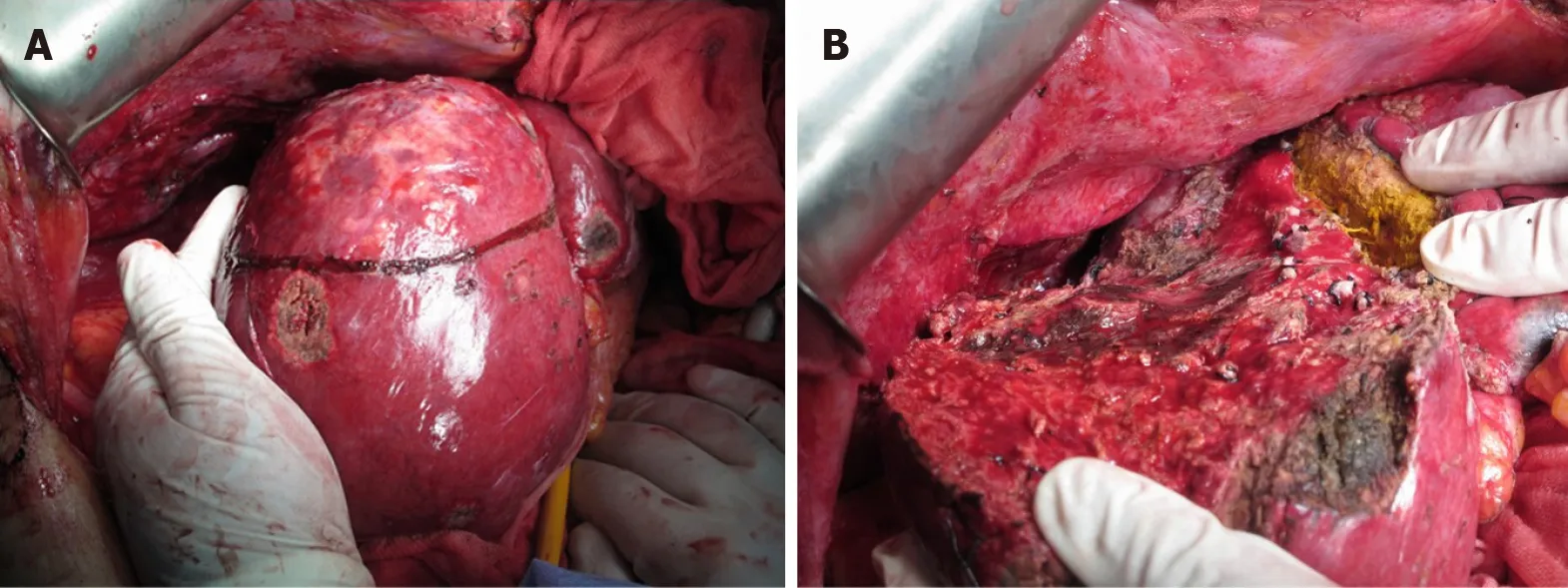
Figure 5 Surgical findings.
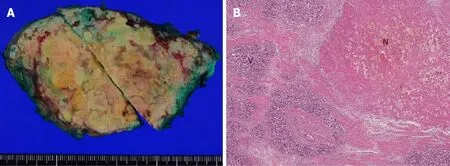
Figure 6 Macroscopic and pathological findings of the resected specimen.
OUTCOME AND FOLLOW-UP
No serious complications, such as bile leakage, were observed.The protein-induced vitamin K absence or antagonist II level decreased to the normal range after surgery (Figure 3).The patient was discharged on day 25 after the operation.Radiation therapy for bone metastases was performed by dividing 30 Gy irradiation into ten applications.At 1 mo after the end of radiotherapy, there was a small intrahepatic recurrence, and lenvatinib was immediately administered.PR was obtained, and the patient has remained alive on administration for 1 year after the second hepatectomy.
DISCUSSION
Here, we report a case in which lenvatinib was administered to a rapidly growing recurrent HCC, and conversion to hepatectomy was achieved after PR was obtained.There are previous case reports describing conversion to surgery for HCC after molecular targeted drug therapy with sorafenib and regorafenib[17,18].The present case report describing conversion to surgery for recurrent HCC after lenvatinib treatment appears to be the first case.
Numerous papers have been published on conversion to surgery for colorectal liver metastases[19,20].However, conversion therapy for HCC has not been established.Lenvatinib is expected to be a possible candidate agent and provides a new treatment perspective for recurrent HCC.To date, most reports have described cases of unresectable or recurrent HCC that were converted after local treatment, such as TACE and hepatic arterial infusion chemotherapy (HAIC), or after conventional anticancer drug treatment[21,22].For example, in a report from the MD Anderson Cancer Center[23], the chemotherapy regimen was cisplatin, interferon α-1b, doxorubicin, and 5-fluorouracil, but the doses and administration schedules had two types (conventional and modified).The study compared and examined the resection rate (conversion rate to curative surgery) and survival rate between the two regimens.In the results, the 3-yr survival rates were 70% for modified chemotherapy plus surgery (n= 11) compared with 20% for modified chemotherapy alone (n= 22) and 60% for conventional chemotherapy plus surgery (n= 8) compared with 5% for conventional chemotherapy alone (n= 76).Therefore, the cases with conversion to surgery showed better survival rates for both the conventional and modified regimens.There are various other reports on conversion to surgery.Hamaokaet al[22]investigated the safety of hepatectomy and overall survival (OS) in 52 patients with unresectable advanced HCC treated with HAIC combined with three-dimensional chemoradiation therapy for portal vein tumor thrombus and compared the resection group with the nonresection group.As a result, OS was significantly higher in the resection group than in the nonresection group.A multivariate analysis identified conversion to surgery as an independent factor influencing OS.
A recent report described a case of HCC with hepatic vein tumor thrombosis protruding into the inferior vena cava that was successfully treated by surgery after second-line chemotherapy with regorafenib[24].Administration of sorafenib was initially started for this case, but 5 wk later the lesion had increased in size.Therefore, regorafenib was subsequently given as second-line therapy and administered for 12 mo.After shrinkage of the inferior vena cava-hepatic vein tumor thrombus, conversion to surgery was successful and a better prognosis was achieved.Meanwhile, Satoet al[25]described a patient with initially unresectable HCC and an arterioportal shunt who underwent conversion hepatectomy after multidisciplinary treatment including lenvatinib[25].
Thus, it is expected that the number of conversion cases will increase with the advent of molecular targeted drugs thereby contributing to improvement in the prognosis of HCC.Similar to previous reports, our patient obtained PR for recurrent HCC after lenvatinib administration and conversion to surgery was achieved.Therefore, it is anticipated that survival can be prolonged by continuing treatment with lenvatinib for bone metastases only.
The limitation is that the administration period for the molecular targeted drug before surgery and the timing of conversion to surgery are unknown.Therefore, it is necessary to collect more cases and perform further studies to clarify these points.
CONCLUSION
In conclusion, we have reported a case of recurrent HCC in which PR was obtained and conversion to surgery was achieved after lenvatinib administration.We believe that even for unresectable advanced and recurrent HCC, hepatectomy can be performed after administration of molecular targeted therapeutic drugs such as lenvatinib and can thus contribute to improvement of the prognosis.
 World Journal of Hepatology2020年12期
World Journal of Hepatology2020年12期
- World Journal of Hepatology的其它文章
- Autophagy related protein 9A increase in hepatitis B virusassociated hepatocellular carcinoma and the role in apoptosis
- Spontaneous bacterial peritonitis due to carbapenemase-producing Enterobacteriaceae: Etiology and antibiotic treatment
- Molecular heterogeneity in intrahepatic cholangiocarcinoma
- Metabolic associated fatty liver disease: Addressing a new era in liver transplantation
- Liver injury in COVID-19: The hepatic aspect of the respiratory syndrome — what we know so far
- Cyclin-dependent kinase inhibitors p21 and p27 function as critical regulators of liver regeneration following 90% hepatectomy in the rat
