地尔硫和硝普钠改善急性冠脉综合征患者经皮冠状动脉介入治疗中无复流现象的效果评价
·论著·

陈章强,戴军,姚民,洪浪,王洪
作者单位:330006江西省南昌市,江西省人民医院心内科(陈章强,洪浪,王洪);中国医学科学院阜外心血管病医院(戴军,姚民)
通信作者:陈章强,330006江西省南昌市,江西省人民医院心内科;E-mail:chenzq888@163.com
【摘要】目的比较地尔硫和硝普钠在改善急性冠脉综合征(ACS)患者经皮冠状动脉介入(PCI)治疗中无复流现象的效果。方法选取2008年1月—2014年6月于江西省人民医院接受PCI治疗且术中出现无复流现象的ACS患者80例为研究对象,采用随机数字表法将患者分为地尔硫组(40例)和硝普钠组(40例)。两组于PCI术中经微导管冠状动脉靶病变远端2 s内“弹丸式”快速分别给予地尔硫、硝普钠200~600 μg,分别于给药后10、20 min后复查冠状动脉造影,评价心肌梗死溶栓治疗(TIMI)血流分级和校正的TIMI血流帧数(CTFC),同时记录给药前及给药后10、20 min有创血压及心率的变化。分别于PCI术前及术后7、30 d记录左心室收缩末内径(LVESD)、左心室舒张末内径(LVEDD)及左心室射血分数(LVEF)。于PCI术前及术后7、30 d测定N末端B型脑钠肽前体(NT-proBNP)及细胞因子超敏C反应蛋白(hs-CRP)、白介素6(IL-6)及细胞间黏附分子-1(ICAM-1)水平。记录两组术后30 d内主要心血管事件(再发心绞痛、再发急性心肌梗死及心力衰竭发作)和其他心血管事件(恶性心律失常及猝死)的发生情况。结果不同药物对TIMI血流分级、CTFC、收缩压、舒张压及心率的影响比较,差异无统计学意义(P>0.05)。两组用药后10、20 min TIMI血流分级、CTFC与用药前比较,差异有统计学意义(P<0.05)。不同药物对LVESD、LVEDD、LVEF的影响比较,差异无统计学意义(P>0.05)。两组术后30 d LVESD、LVEDD及LVEF与术前比较,差异有统计学意义(P<0.05)。不同药物对NT-proBNP、hs-CRP、IL-6及ICAM-1的影响比较,差异无统计学意义(P>0.05)。两组术后7、30 d NT-proBNP、hs-CRP、IL-6、ICAM-1水平均低于术前,差异有统计学意义(P<0.01)。两组术后30 d内主要心血管事件及其他心血管事件发生率比较,差异均无统计学意义(P>0.05)。结论地尔硫和硝普钠均能够有效改善PCI术中TIMI血流分级及CTFC,降低炎性因子和NT-proBNP水平,改善心功能,两者改善无复流现象的效果相当。
【关键词】急性冠脉综合征;经皮冠状动脉介入治疗;无复流现象;地尔硫;硝普钠;疗效比较研究
【中图分类号】R 542.2
收稿日期:(2015-05-07;修回日期:2015-11-08)
Chen ZQ, Dai J, Yao M,et al.Effects of diltiazem and sodium nitroprusside on alleviating no-reflow phenomenon in patients with acute coronary syndrome during percutaneous coronary intervention[J].Chinese General Practice,2015,18(35):4283-4287.
Effects of Diltiazem and Sodium Nitroprusside on Alleviating No-reflow Phenomenon in Patients With Acute Coronary Syndrome During Percutaneous Coronary InterventionCHENZhang-qiang,DAIJun,YAOMin,etal.DepartmentofCardiology,JiangxiProvincialPeople′sHospital,Nanchang330006,China
Abstract【】ObjectiveTo make a comparison between diltiazem and sodium nitroprusside in alleviating no-flow phenomenon in patients with acute coronary syndrome (ACS) during percutaneous coronary intervention (PCI).MethodsWe enrolled 80 ACS patients who had no-flow phenomenon during PCI undertaken in Jiangxi Provincial People′s Hospital from January 2008 to June 2014.Using random number table method,the patients were divided into two groups:diltiazem group (group A,n=40) and sodium nitroprusside group (group B,n=40).Group A was given diltiazem 200-600 μg by pellet injection from microcatheter selective coronary to far-end target lesions in two seconds,group B was given sodium nitroprusside 200-600 μg in the same way.Coronary arteriography was retaken 10 minutes and 20 minutes after administration.Thrombolysis in Myocardial Infarction (TIMI) flow grade and corrected TIMI frame count (CTFC) were evaluated.Invasive blood pressure and heart rate were recorded before administration and 10 minutes and 20 minutes after administration.LVESD,LVEDD and LVEF were recorded before PCI and 7 days and 30 days after PCI.The levels of NT-proBNP,hs-CRP,IL-6 and ICAM-1 were recorded before PCI and 7 days and 30 days after PCI.The incidence rates of major cardiovascular events (re-angina,re-myocardial infarction and heart failure) and other cardiovascular events (malignant arrhythmia and sudden death) were recorded.ResultsThe two medicines were not significantly different (P>0.05) in the influence on TIMI flow grade,CTFC,systolic pressure,diastolic pressure and heart rate.TIMI flow grade and CTFC of the two groups at 10 minutes and 20 minutes after administration were significantly different from those before administration (P<0.05).The two medicines were not significantly different (P>0.05) in the influence on LVESD,LVEDD and LVEF.The levels of LVESD,LVEDD and LVEF of the two groups on 30 days after administration were significantly different from those before administration (P<0.05).The two medicines were not significantly different (P>0.05) in the influence on NT-proBNP,hs-CRP,IL-6 and ICAM-1.The levels of NT-proBNP,hs-CRP,IL-6 and ICAM-1 of the two groups on 7 days and 30 days after administration were significantly different from those before administration (P<0.05).The two groups were not significantly(P>0.05) different in the incidence rates of major cardiovascular events and other cardiovascular events.ConclusionDiltiazem and sodium nitroprusside can effectively improve TIMI flow grade and CTFC,reduce the levels of inflammatory factor and NT-proBNP and improve cardiac function.The two medicines have equally good effect on alleviating on-flow pheonmenon.
【Key words】Acute coronary syndrome;Percutaneous coronary intervention;No-reflow phenomenon;Diltiazem;Nitroprusside;Comparative effectiveness research

1资料与方法

1.2方法
1.2.1基线资料包括患者性别、年龄、吸烟史、合并糖尿病、ACS类型及入院时血压、血脂水平〔三酰甘油(TG)、总胆固醇(TC)、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)〕。
1.2.3心功能测定分别于PCI术前及术后7、30 d复查心脏彩超(美国惠利普公司Agilent 5500型),记录左心室收缩末内径(LVESD)、左心室舒张末内径(LVEDD)及左心室射血分数(LVEF)。
1.2.4N末端B型脑钠肽前体(NT-proBNP)及细胞因子水平的测定分别于PCI术前及术后7、30 d测定NT-proBNP及细胞因子超敏C反应蛋白(hs-CRP)、白介素6(IL-6)及细胞间黏附分子-1(ICAM-1)水平。NT-proBNP的测定采用胶体金标法,试剂盒购自丹麦Radiometer Medical ApS公司,变异系数为0.5%;hs-CRP的测定采用免疫散射比浊法,试剂盒购自美国德灵公司,按照试剂盒说明书严格进行操作,变异系数为1.5%;IL-6和ICAM-1的测定采用酶联免疫吸附试验(ELISA),按试剂盒说明书严格进行操作,变异系数为1.2%。
1.2.5预后记录两组术后30 d内主要心血管事件(再发心绞痛、再发急性心肌梗死及心力衰竭发作)和其他心血管事件(恶性心律失常及猝死)的发生情况。

2结果
2.1基线资料比较两组性别、年龄、吸烟、糖尿病、ACS类型、收缩压、舒张压、TG、TC、HDL-C及LDL-C比较,差异均无统计学意义(P>0.05,见表1)。
2.2两组用药前后TIMI血流、血压及心率变化不同药物与时间对TIMI血流分级、CTFC、收缩压、舒张压及心率的影响无交互作用(P>0.05)。不同药物对TIMI血流分级、CTFC、收缩压、舒张压及心率的影响比较,差异无统计学意义(P>0.05)。两组用药后10、20 min TIMI血流分级、CTFC与用药前比较,差异有统计学意义(P<0.05,见表2)。
2.3两组患者心脏结构及心功能比较不同药物与时间对LVESD、LVEDD、LVEF的影响无交互作用(P>0.05)。不同药物对LVESD、LVEDD、LVEF的影响比较,差异无统计学意义(P>0.05)。两组术后30 d LVESD、LVEDD及LVEF与术前比较,差异有统计学意义(P<0.05,见表3)。
2.4两组NT-proBNP、细胞因子水平比较不同药物与时间对NT-proBNP、hs-CRP、IL-6及ICAM-1的影响无交互作用(P>0.05)。不同药物对NT-proBNP、hs-CRP、IL-6及ICAM-1的影响比较,差异无统计学意义(P>0.05)。两组术后7、30 d NT-proBNP、hs-CRP、IL-6、ICAM-1水平均低于术前,差异有统计学意义(P<0.01,见表4)。
2.5预后两组术后30 d内主要心血管事件及其他心血管事件发生率比较,差异均无统计学意义(P>0.05,见表5)。
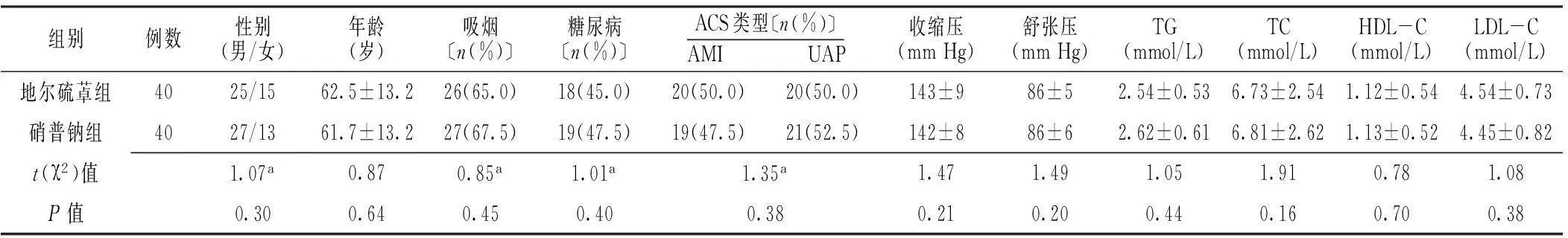
表1 两组患者一般资料比较
注:ACS=急性冠脉综合征,AMI=急性心肌梗死,UAP=不稳定型心绞痛,TG=三酰甘油,TC=总胆固醇,HDL-C=高密度脂蛋白胆固醇,LDL-C=低密度脂蛋白胆固醇;a为χ2值

表2 两组患者血流、血压及心率比较 ±s)
注:TIMI=心肌梗死溶栓治疗,CTFC=校正的TIMI血流帧数;与同组用药前比较,aP<0.05

表3 两组患者心脏结构及心功能比较 ±s)
注:LVESD=左心室收缩末内径,LVEDD=左心室舒张末内径,LVEF=左心室射血分数;与同组术前比较,aP<0.05

表4 两组NT-proBNP和细胞因子水平比较 ±s)
注:NT-proBNP=N末端B型脑钠肽前体,hs-CRP=超敏C反应蛋白,IL-6=白介素6,ICAM-1=细胞间黏附分子-1;与同组术前比较,aP<0.05
表5两组术后30 d心血管事件发生率比较〔n(%)〕
Table 5Comparison of the incidence rates of cardiovascular events between the two groups

组别例数主要心血管事件其他心血管事件地尔硫卓艹组404(10.0)1(2.5)硝普钠组404(10.0)1(2.5)χ2值<0.01<0.01P值>0.05>0.05
3讨论
1972年,Tambe等[18]首次报道急性心肌梗死(AMI)患者急诊PCI术中出现慢血流现象,此后随着冠心病患病率的升高及PCI的广泛推广,该现象已被介入医生所熟悉。由于无复流现象不能实现心肌组织的有效灌注,成为PCI术后近期和远期预后不良的危险因素[3]。无复流现象发生机制复杂,尚未完全阐明,有学者提出可能与微血管损伤、微血管栓塞、血管痉挛、氧化应激、血小板激活及白细胞聚集等有关[8,19]。炎性反应是介导动脉斑块破裂导致AMI的重要原因,也是导致无复流现象的重要机制之一[20]。本研究结果发现,两组患者PCI术后7、30 d,与炎性反应有关的细胞因子hs-CRP、IL-6、ICAM-1表达水平均低于术前。血清NT-proBNP是主要由心室肌细胞合成的心源性神经激素,具有拮抗肾素-血管紧张素-醛固酮系统、利尿排钠、扩张血管等作用,其水平升高常见于心室容量负荷、室壁压力增高及心肌细胞受损等。本研究显示,两组患者术前NT-proBNP水平明显增高,可能与交感神经和肾素-血管紧张素-醛固酮系统激活,心室肌细胞的应激及室壁张力增高有关。

参考文献
[1]郭文怡,张东伟,赵志敬.急性冠状动脉综合征患者再灌注策略的选择[J].中国介入心脏病学杂志,2014,22(5):333-335.
[2]Yu LT,Zhu J,Rebecca M,et al.The Chinese registry on reperfusion strategies and outcomes in ST-elevation myocardial infarction[J].Chinese Journal of Cardiology,2006,34(7):593-597.(in Chinese)
于丽天,朱俊,Rebecca Mister,等.我国部分医院ST段抬高急性冠状动脉综合征再灌注治疗登记研究[J].中华心血管病杂志,2006,34(7):593-597.
[3]Resnic FS,Wainstein M,Lee MK,et al.No-reflow is an independent predictor of death and myocardial infarction after percutaneous coronary intervention[J].Am Heart J,2003,145(1):42-46.
[4]Ozdogru I,Zencir C,Dogan A,et al.Acute effects of intracoronary nitroglycerin and diltiazem in coronary slow flow phenomenon[J].J Investig Med,2013,61(1):45-49.
[5]Fugit MD,Rubal BJ,Donovan DJ.Effects of intracoronary nicardipine,diltiazem and verapamil on coronary blood flow[J].J Invasive Cardiol,2000,12(2):80-85.
[6]Zheng ZF,Pu XQ,Yang TL,et al.Effects of intracoronary diltiazem on no-reflow phenomenon after emergent percutaneous coronary intervention in patients with acute myocardial infarction[J].Journal of Central South University(Medical Sciences),2006,31(6):917-920.
[7]Tang O,Wu J,Qin F,et al.Relationship between methylenetetrahydrofolate reductase gene polymorphism and the coronary slow flow phenomenon[J].Coron Artery Dis,2014,25(8):653-657.
[8]Huang D,Qian J,Ge L,et al.Restoration of Coronary flow in patients with no-reflow after primary coronary intervention of acute myocardial infarction (RECOVER)[J].Am Heart J,2012,164(3):394-401.
[9]Tesic MB,Stankovic G,Vukcevic V,et al.The use of intracoronary sodium nitroprusside to treat no-reflow after primary percutaneous coronary intervention in acute myocardial infarction[J].Herz,2010,35(2):114-118.
[10]Shinozaki N,Ichinose H,Yahikozawa K,et al.Selective intracoronary administration of nitroprusside before balloon dilatation prevents slow reflow during percutaneous coronary intervention in patients with acute myocardial infarction[J].Int Heart J,2007,48(4):423-433.
[11]Amit G,Cafri C,Yaroslavtsev S,et al.Intracoronary nitroprusside for the prevention of the no-reflow phenomenon after primary percutaneous coronary intervention in acute myocardial infarction.A randomized,double-blind,placebo-controlled clinical trial[J].Am Heart J,2006,152(5):887.
[12]Niccoli G,D′amario D,Spaziani C,et al.Randomized evaluation of intracoronary nitroprusside vs.adenosine after thrombus aspiration during primary percutaneous coronary intervention for the prevention of no-reflow in acute myocardial infarction:the REOPEN-AMI study protocol[J].J Cardiovasc Med (Hagerstown),2009,10(7):585-592.
[13]Niccoli G,Rigattieri S,De Vita MR,et al.Open-label,randomized,placebo-controlled evaluation of intracoronary adenosine or nitroprusside after thrombus aspiration during primary percutaneous coronary intervention for the prevention of microvascular obstruction in acute myocardial infarction:the REOPEN-AMI study (Intracoronary Nitroprusside Versus Adenosine in Acute Myocardial Infarction)[J].JACC Cardiovasc Interv,2013,6(6):580-589.
[14]Hillegass WB,Dean NA,Liao L,et al.Treatment of no-reflow and impaired flow with the nitric oxide donor nitroprusside following percutaneous coronary interventions:initial human clinical experience[J].J Am Coll Cardiol,2001,37(5):1335-1343.
[15]Wang JW,Zhou ZQ,Chen YD,et al.A risk score for no reflow in patients with ST-segment elevation myocardial infarction after primary percutaneous coronary intervention[J].Clin Cardiol,2015,38(4):208-215.
[16]Bertrand ME,Simoons ML,Fox KA,et al.Management of acute coronary syndromes:acute coronary syndromes without persistent ST segment elevation:recommendation of the Task Force of the European Society of Cardiology[J].Eur Heart J,2000,21(17):1406-1432.
[17]Gibson CM,Schomi A.Coronary and myocardial angiography:angiographic assessment of both epicardial and myocardial perfusion[J].Circulation,2004,109(25):3096-3105.
[18]Tambe AA,Demany MA,Zimmerman HA,et al.Angina pectoris and slow flow velocity of dye in coronary arteries-a new angiographic finding[J].Am Heart J,1972,84(1):66-71.
[19]Niccoli G,Cosentino N,Spaziani C,et al.New strategies for the management of no-reflow after primary percutaneous coronary intervention[J].Expert Rev Cardiovasc Ther,2011,9(5):615-630.
[20]Zakroysky P,Thai WE,Deano RC,et al.Steroid exposure,acute coronary syndrome,and inflammatory bowel disease:insights into the inflammatory milieu[J].Am J Med,2015,128(3):303-311.
[21]Rognoni A,Lupi A,Cavallino C,et al.Intracoronary injection of drugs to treat no-reflow phenomenon and microcirculatory dysfunction[J].Cardiovasc Hematol Agents Med Chem,2013,11(2):84-88.
[22]Maluenda G,Ben-Dor I,Delhaye C,et al.Clinical experience with a novel intracoronary perfusion catheter to treat no-reflow phenomenon in acute coronary syndromes[J].J Interv Cardiol,2010,23(2):109-113.
(本文编辑:吴立波)

