等渗剂量7.5%高渗盐水和20%甘露醇降低颅内压的效果比较
霍生杰 张文岐 金道 王江峰 陈琛李 浩 董 涛

[摘要] 目的 比較等渗剂量7.5%高渗盐水和20%甘露醇降低颅内压(ICP)的效果。 方法 回顾性分析陕西中医药大学第二附属医院2015年1月~2018年6月收治的重型颅脑创伤致颅内高压患者的病例资料。其中收集符合纳入标准的病例共30例,根据高渗治疗方法分为7.5%高渗盐水组(15例)和20%甘露醇组(15例)。比较两组患者治疗后ICP降低降幅、起效时间、有效持续时间、ICP最低值所需时间、脑灌注压(CPP)、平均动脉压(MAP)、中心静脉压(CVP)。分析两组患者治疗前及治疗后1、3 h血钠浓度和血浆渗透压。 结果 7.5%高渗盐水组治疗后ICP降低幅度高于20%甘露醇组,起效时间、有效持续时间均长于20%甘露醇组,ICP最低值所需时间短于20%甘露醇组,差异均有统计学意义(均P < 0.05)。7.5%高渗盐水组治疗后CPP及MAP高于20%甘露醇组,差异有统计学意义(P < 0.05);两组治疗后的CVP比较差异无统计学意义(均P > 0.05)。两组治疗前及治疗后1、3 h血浆渗透压、血钠浓度组内比较,差异均有统计学意义(均P < 0.05);两组治疗后1、3 h的血浆渗透压、血钠浓度组间比较,差异均有统计学意义(均P < 0.05)。 结论 7.5%高渗盐水降ICP效果优于20%甘露醇。
[关键词] 高渗盐水;甘露醇;颅内压;重型颅脑创伤
[中图分类号] R742 [文献标识码] A [文章编号] 1673-7210(2019)09(b)-0141-04
Effect comparation of isosmotic dose of 7.5% hypertonic saline and 20% mannitol on intracranial pressure reduction
HUO Shengjie ZHANG Wenqi LIU Jindao WANG Jiangfeng CHEN Chen LI Hao DONG Tao▲
Department of Neurosurgery, the Second Affiliated Hospital of Shaanxi University of Traditional Chinese Medicine, Shaanxi Province, Xianyang 712000, China
[Abstract] Objective To compare the effect of isosmotic dose of 7.5% hypertonic saline and 20% mannitol on intracranial pressure (ICP) reduction. Methods The data of patients with intracranial hypertension caused by severe traumatic brain injury admitted to the Second Affiliated Hospital of Shaanxi University of Traditional Chinese Medicine from January 2015 to June 2018 were retrospectively analyzed. Among them, 30 cases met the inclusion criteria were collected and divided into 7.5% hypertonic saline group (15 cases) and 20% mannitol group (15 cases) according to hypertonic therapy. The reduction of ICP, onset time, effective duration, minimum ICP time, cerebral perfusion pressure (CPP), mean arterial pressure (MAP) and central venous pressure (CVP) were compared between two groups. Serum sodium concentration and plasma osmotic pressure were analyzed before treatment and 1 and 3 hours after treatment between two groups. Results After treatment, ICP in 7.5% hypertonic saline group decreased more than that in 20% mannitol group, the onset time and effective duration in 7.5% hypertonic saline group were longer than that in 20% mannitol group, and the minimum ICP time in 7.5% hypertonic saline group was shorter than that in 20% mannitol group, the differences were statistically significant (all P < 0.05). CPP and MAP of 7.5% hypertonic saline group after treatment were higher than those of 20% mannitol group, the differences were statistically significant (P < 0.05). There was no significant difference in CVP between two groups after treatment (P > 0.05). There were statistically significant differences in plasma osmotic pressure and sodium concentration between two groups before treatment and 1 and 3 hours after treatment (all P < 0.05). There were statistically significant differences in plasma osmotic pressure and sodium concentration between two groups 1 and 3 hours after treatment (all P < 0.05). Conclusion ICP reduction effect of 7.5% hypertonic saline is better than that of 20% mannitol.
[Key words] Hypertonic saline; Mannitol; Intracranial pressure; Severe traumatic brain injury
颅内压(ICP)增高是颅脑创伤后最常见临床症状,而ICP升高与预后直接相关[1]。根据指南[2],当ICP超过20 mmHg(1 mmHg = 0.133 kPa)时就应该给予降ICP治疗。高渗盐水与甘露醇是临床最常用的降ICP药物[2],然而目前对两者的疗效认识及首选推荐存在争议。甘露醇降ICP效果被认可,起效快,但不良反应多。而高渗盐水,被广泛推荐应用,研究表明高渗盐水比甘露醇的降ICP效果好[3-4],副作用少。本研究对接受等渗剂量的7.5%高渗盐水和20%甘露醇治疗患者的病例资料进行回顾性分析,比较两者降ICP的效果,现报道如下:
1 资料与方法
1.1 一般资料
收集陕西中医药大学第二附属医院神经外科2015年1月~2018年6月收治的重型颅脑创伤致颅内高压患者,符合标准病例共30例(男20例,女10例)。纳入标准:①年龄20~70岁;②ICP > 20 mmHg持续 5 min以上;③所有患者ICP传感器均为脑室型;④格拉斯哥昏迷评分(GCS)5~8分。排除标准:①烦躁、吸痰、翻身等颅外因素引起ICP的升高;②严重的复合伤、脑死亡、脑疝或休克;③严重水电解质及酸碱平衡紊乱难以纠正;④合并严重心肺功能和凝血功能障碍。7.5%高渗盐水组男9例,女6例;年龄20~70岁,平均(38.4±8.0)岁;20%甘露醇组男11例,女4例;年龄22~67岁,平均(36.1±15.7)岁。两组患者性别、年龄比较差异无统计学意义(P > 0.05),具有可比性。
1.2 常规治疗
依照神经外科指南[5],收住神经外科重症监护室治疗,给予置入脑室型颅内压探测仪,持续监测ICP,常规术后1周内拔除;保持脑灌注压> 60 mmHg;给予相应的镇静镇痛治疗、床头抬高30°、维持正常体温、保持血压平稳及血糖浓度,不使用激素;部分患者行锁骨下深静脉置管;多功能监测仪监测生命体征;根据病情,部分患者行开颅手术治疗;加强呼吸道管理,并给予呼吸支持。通过计算,4 mL/kg的7.5 %高渗盐水与0.5 g/kg的20%甘露醇的渗透剂量基本相等,药物在30 min内快速滴注完成。
1.3 观察指标
监测并记录患者治疗后ICP降低降幅、起效时间、有效持续时间及ICP最低值所需时间;记录患者治疗后脑灌流压(CPP)、平均动脉压(MAP)、中心静脉压(CVP)及治疗前和治疗后1、3 h的血浆渗透压及血钠浓度。
1.4 统计学方法
所有数据采用SPSS 19.0软件进行分析,计量资料以均数±标准差(x±s)表示,两组间比较采用t检验,两因素重复测量资料采用重复测量资料的方差分析。以 P < 0.05为差异有统计学意义。
2 结果
2.1 两组患者治疗后ICP相关指标比较
7.5%高渗盐水组治疗后的ICP降低幅度高于20%甘露醇组,起效时间、有效持續时间均长于20%甘露醇组,ICP最低值所需时间短于20%甘露醇组,差异均有统计学意义(P < 0.05)。见表1。
表1 两组患者治疗后ICP相关指标比较(x±s)
注:ICP:颅内压;1 mmHg = 0.133 kPa
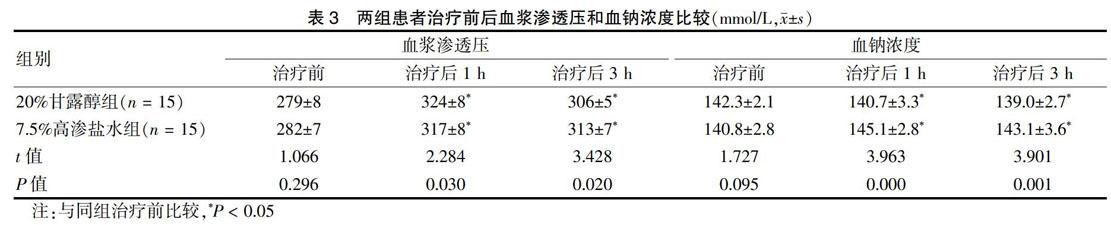
2.2 两组患者治疗后MAP、CPP和CVP比较
7.5%高渗盐水组治疗后CPP及MAP高于20%甘露醇组,差异有统计学意义(P < 0.05);两组治疗后的CVP比较差异无统计学意义(P > 0.05)。见表2。
表2 两组患者治疗后MAP、CPP和CVP比较(x±s)
注:CPP:脑灌流压;MAP:平均动脉压;CVP:中心静脉压;1 mmHg = 0.133 kPa;1 mmH2O = 9.8 Pa
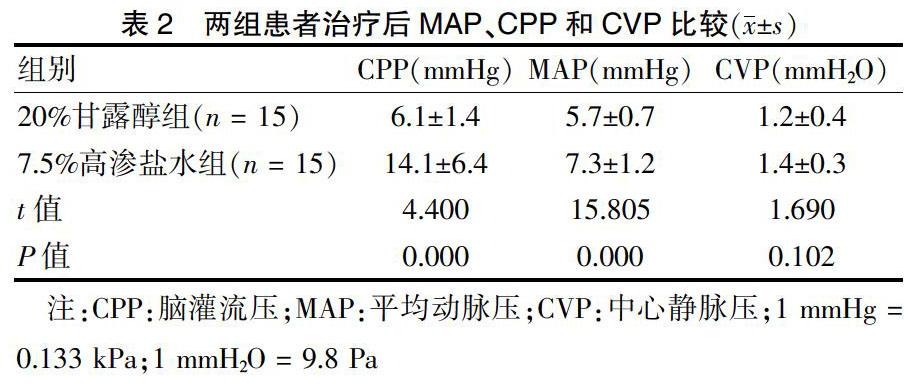
2.3 两组患者治疗前后血浆渗透压和血钠浓度比较
两组治疗前及治疗后1、3 h的血浆渗透压、血钠浓度组内比较,差异均有统计学意义(P < 0.05);两组治疗后1、3 h的血浆渗透压、血钠浓度组间比较,差异均有统计学意义(P < 0.05)。见表3。
3 讨论
颅脑创伤是现代社会严重影响人类健康的疾病,临床救治中充满巨大挑战[6]。近年来,神经外科快速发展,推出了规范化内科及外科治疗指南,接受先进的治疗理念(如隆德理念)指导,致使显著提高颅脑创伤患者的生存率,治疗过程中维持ICP稳定尤为重要[7]。而高渗脱水剂是治疗颅内高压的重要方法[8-9],美国最新的《重型颅脑创伤救治指南(第四版)》[10]认为高渗药物对颅脑创伤治疗有效。
甘露醇是临床最常用的降ICP药物,除利尿作用外,主要通过提高血液渗透压使脑组织的水分吸入血液,并通过肾脏排出体外,从而降低ICP[11]。甘露醇只能对正常脑组织水分有脱水作用,当血-脑积液屏障被破坏时,甘露醇可从破裂血管进入脑组织挫伤病灶区,造成病灶区脑水肿加重。对于脑缺血患者,因血管通透性增加,可导致逆向渗透。此外,甘露醇还可引起利尿相关性低血压、急性肾功能衰竭、电解质紊乱、ICP反跳以及早期出血增加等并发症,使用甘露醇应更加谨慎[12]。相反,高渗盐水逐渐被国内外学者推荐应用[13],通过直接提高细胞外液钠离子浓度、增加血浆渗透压脱水来降低ICP,对内环境平衡的影响小,不会导致利尿性低血压[14]。高渗盐水不仅可以为细胞内环境提供必需的钠离子,有利于钠钾泵功能正常,可保持细胞体积及维持细胞静息电位,也可以升高CPP和增加脑组织氧合[15]。对于颅高压危象、恶性颅高压及肾功能不全的患者,使用高渗盐水效果更好;尤其儿童患者,高渗盐水被唯一推荐使用[16]。虽然高渗盐水疗效被认可,特别是用于难治性ICP升高,但缺乏最有效浓度或剂量的证据,并存在相关并发症,如低血钾、一过性酸中毒、高钠血症等。偶有引起肾功能衰竭,当在纠正低钠血症过快时可引起脑桥中央髓鞘溶解,临床少见[17]。
[11] Tang SC,Lin RJ,Shieh JS,et al. Effect of mannitol oncerebrovascular pressure reactivity in patients with intracranialhypertension [J]. J Formos Med Assoc,2015, 114(9):842-848. doi:10.1016/j.jfma.2013.09.002.
[12] Mangat HS,Hrtl R. Hypertonic saline for the management of raised intracranial pressure after severe traumatic brain injury [J]. Ann NY Acad SCI,2015(1345):83-88.
[13] Stewart R,Ghamande S,White H,et al. Protocol for administration of hypertonic saline in medical intensive care patients with severe stroke [J]. Chest,2016,150(4):230A.
[14] Ali A,Tetik A,Sabanci PA,et al. Comparison of 3% hypertonic saline and 20% mannitol for reducing intracranial pressure in patients undergoing supratentorial brain tumor surgery:a randomized,double-blind clinical trial [J]. J Neurosurg Anesthesiol,2018,30(2):171-178.
[15] Prabhakar H,Singh GP,Anand V,et al. Mannitol versushypertonic saline for brain relaxation in patients undergoing craniotomy [J]. Sao Paulo Med J,2015,133(2):166-167.
[16] Ockswold GL,Solid CA,Paredes-Andrade E,et al. Hypertonic saline and its effect on intracranial pressure,cerebral perfusion pressure,and brain tissue oxygen [J]. Neurosurgery,2009,65(6):1035-1041.
[17] Lazaridis C,Neyens R,Bodle J,et al. High oasmolarity saline in neurocritical care:systematic review and meta-analysis [J]. J Neurosury,2012,116(1):210-221.
[18] 楊细平,张馨予,涂悦,等.不同浓度高渗盐水对颅脑创伤后颅内高压患者的疗效观察[J].天津医药,2017,45(8):810-814.
[19] Kochanek PM,Carney N,Adelson PD,et al. Guidelines for the acute medical management of severe traumatic brain injury ininfants,children,and adolescents-second edition [J]. Pediatr Crit Care Med,2012,13(Suppl 1):S1-S82.
[20] 柴磊,杨彦龙,孙红星,等.等渗透剂量的7.5%高渗盐水和20%甘露醇治疗颅内高压疗效的对比研究[J].现代生物医学进展,2015,15(29):5728-5731.
[21] Ichai C,Armando G,Orban JC,et al. Sodium lactate versus mannitol in the treatment of intracranial hypertensive episodesin severe traumatic brain-injured patients [J]. Intensive Care Med,2009,35(3):471-479.
(收稿日期:2019-01-15 本文编辑:李亚聪)