Subsequent pregnancy outcomes and fertility rates in the case series that underwent bilateral hypogastric artery ligation (BHGAL) due to severe postpartum hemorrhage
OKUTUCU Gulcan ,EVSEN Mehmet S ,PEKER Nurullah ,YAMAN TUNC Senem ,ICEN Mehmet S
1Department of Obstetrics and Gynecology,Division of Perinatology,Turkish Ministry of Health Ankara City Hospital,Ankara,Turkey
2Department of Obstetrics and Gynecology,Dicle University,School of Medicine,Diyarbakir,Turkey
ABSTRACT Objective: To evaluate the effect of bilateral hypogastric artery ligation (BHGAL) on women's pregnancy outcomes and fertility rates in cases with severe postpartum hemorrhage.Methods: Patients hospitalized in a tertiary care center between 2007 and 2018 were included in the study.The records of cases were obtained from the hospital database,retrospectively.Maternal demographic data,morbidities or complications associated with BHGAL surgery,any additional haemostatic interventional or surgical procedures,preoperative admission and lowest postoperative haematocrit-hemoglobin values,blood products given,type of anaesthesia,intensive care unit (ICU) and length of hospital stay were recorded.In cases without surgical sterilization,future fertility and subsequent pregnancy outcomes were assessed for at least two years after operation.Information was obtained through face-to-face or telephone interviews with patients whose long-term fertility and subsequent pregnancy outcomes were assessed.Results: Sixty-eight patients with BHGAL surgery history were included in the study.26 Of 37 cases (70%) that did not undergo surgical sterilization had a desire for pregnancy after the surgery.Six of these cases (23%) were diagnosed with secondary infertility.The fertility rate of these cases was 77%,and subsequent pregnancy was detected in 20 women.A total of 25 pregnancies,including first and second pregnancies,developed,and 15 of these pregnancies resulted in term delivery,six preterm births,one stillbirth,and three abortions.Conclusions: The postoperative pregnancy rate was found to be higher than the rate of women with infertility problems,and this surgery does not seem to adversely affect pregnancy outcomes.This is a tertiary center experience and cohort studies with large patient series are needed.
KEYWORDS: Fertility;Iliac artery;Ligations;Postpartum hemorrhage;Pregnancy outcomes
1.Introduction
Postpartum hemorrhage (PPH) is a common and challenging clinical emergency and may result in maternal mortality if not intervened promptly.It complicates 1%-5% of all deliveries and accounts for 25% of all maternal deaths worldwide.The expected blood losses for vaginal delivery and cesarean section are 500 and 1 000 mL,respectively[1,2].Severe PPH can be defined as postpartum blood loss of 1000 mL or more in the first 24 h after birth,regardless of the mode of delivery.Symptoms or signs of hypovolemia may be observed in cases with PPH[3,4].Uterine atony is the most common cause of PPH and accounts for 80% of the cases[1].
Significance
Hypogastric artery ligation probably does not affect the subsequent fertility and pregnancy outcomes.The loss of reproductive function caused by hysterectomy has led to the need for alternative surgical methods in cases of severe postpartum bleeding.At this point,hypogastric artery ligation remains the pelvic surgical procedure of choice for obstetricians in young or low parity women experiencing severe postpartum hemorrhage.This study revealed that bilateral hypogastric artery ligation surgery does not seem to adversely affect pregnancy outcomes.
Intervention options for postpartum bleeding may differ between patients.Etiological factors,surgeons' experience,and hospital conditions shape these differences[5].Surgical intervention should be considered without delay in bleeding that does not stop despite uterotonic treatment or bimanual uterine massage[1].Traditionally,hysterectomy has been applied in life-threatening cases due to severe PPH refractory to conservative treatment methods and still has a place in obstetric surgery[6].The fact that hysterectomy causes loss of reproductive function has led to the need for alternative surgical methods.At this point,bilateral hypogastric artery ligation (BHGAL)may be one of these procedures.
In studies evaluating the long-term fertility results of BHGAL surgery in the literature,the results point to higher pregnancy rates and no adverse effect on future fertility[7,8].This study is a retrospective case series and aims to evaluate the impact of the BHGAL for severe PPH on women's future fertility and subsequent pregnancy outcomes.
2.Materials and methods
2.1.Participant’s numbers and characteristics
Patients who were operated on in the Gynecology and Obstetrics Service of Dicle University Medical Faculty Hospital between 2007 and 2018 were included in the study.Cases with done laparotomy due to severe PPH that did not respond to conservative treatment during or after cesarean or after vaginal delivery were evaluated.Pregnancies terminated before the 20th gestational week,patients who underwent BHGAL with a gynecological indication or occurred maternal death were excluded from the study.
There were 22 339 births in the date range of the study,and BHGAL was performed in one of 243 live births.This procedure was applied to 135 cases (97.8%) for obstetric reasons.Uterinesparing surgery was performed in 54.1% (n=73) of these cases.Four cases could not be reached because of incomplete data in the hospital database,and one patient refused to participate.Thus,68 cases were included in the study.The flowchart of information about the number of cases is given in Figure 1.
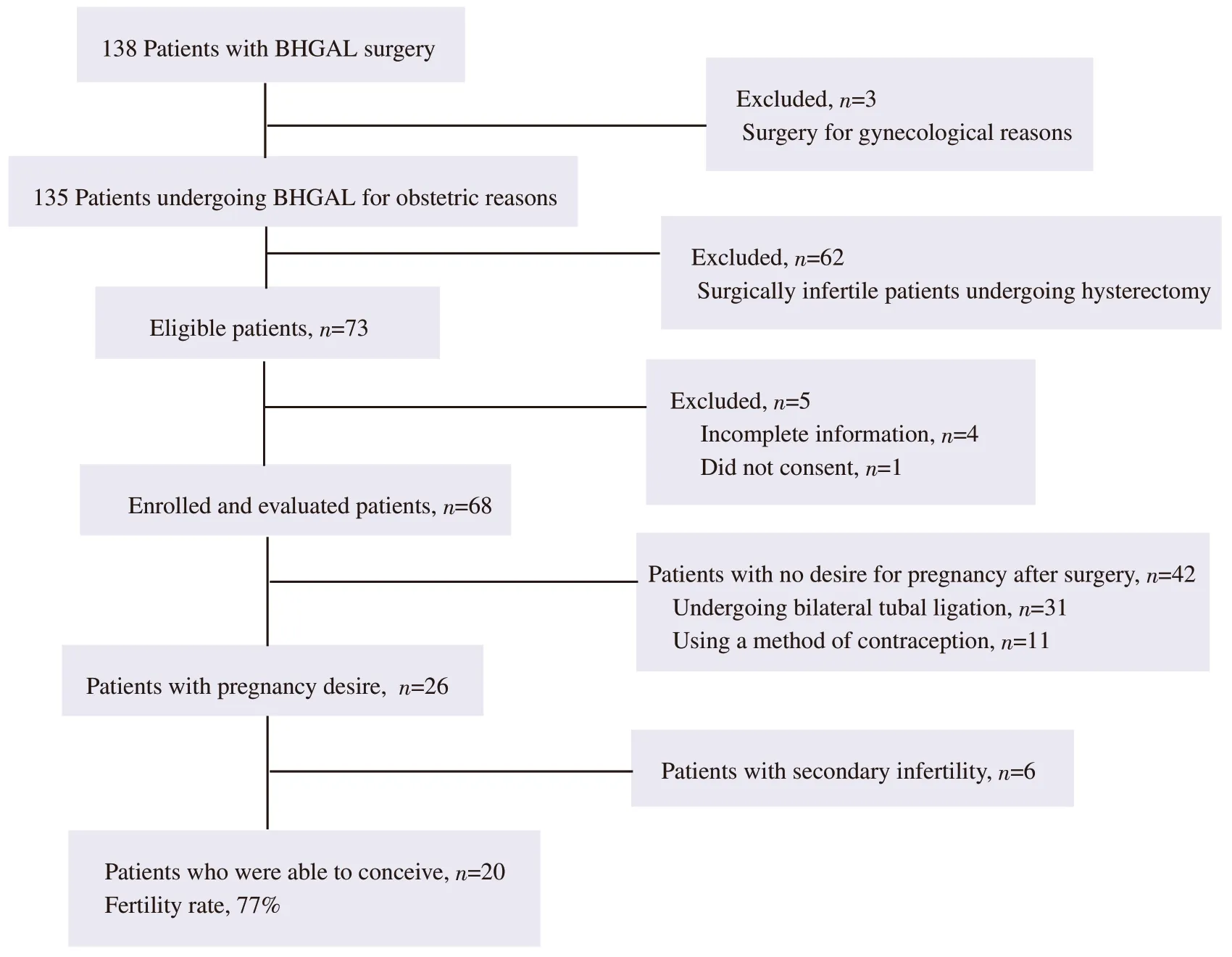
Figure 1. The flowchart of the number of participants and the cases with reproductive outcomes.BHGAL: bilateral hypogastric artery ligation.
The participants were given detailed information about the study to be carried out,and they were asked whether they would like to participate in the study,either face-to-face orviatelephone.Faceto-face interviews were conducted with 28 patients in the outpatient clinic.Then,the informed consent form was read and signed by each of them.However,after the coronavirus disease (COVID-19)pandemic began to affect our country on March 2020[9],40 patients were not called to the hospital to prevent a possible viral contagion,and instead of meeting face to face,the participants were interviewed by phone.Verbal informed consent was obtained from the women who wanted to participate in the study.
2.2.Information on the assessed data
The records of the patients in the hospital archive was analyzed retrospectively from the database.The relevant data obtained were maternal age,gravidity,parity,previous cesarean history,presence of chronic disease,gestational week,mode of delivery,causes of PPH,whether an interventional or surgical additional method is used to provide hemostasis (uterine compression sutures,uterine and/or ovarian artery ligation,uterine Bakri®postpartum balloon or foley catheter application,etc.),surgery-related morbidities and complications,preoperative initial and postoperative lowest hematocrit (Hct)-hemoglobin (Hgb) values,type of anesthesia,length of stay in the intensive care unit (ICU) and clinic.
Unit (U) of transfused blood products was calculated during the hospitalization period.If 10 U of red blood cells (RBCs) were given within 24 h or 3 U or more of RBCs were given within 1 h,or if any type of blood components were transfused at an amount of 4 U or more within 30 min,the patient was defined as a case with massive blood transfusion[10].
2.3.Surgical procedure of BHGAL
The ligation procedure was performed bilaterally in all cases.The surgical technique was the standard.It has been seen by examining the operation notes in the electronic data system of the hospital that the procedure was applied to patients with similar methods.The hypogastric artery was ligated approximately 4 cm distal to the bifurcation point of the common iliac artery using an absorbable suture [United States Pharmacopeia (USP) size 0 or 1].
2.4.Long-term assessments
Future fertility and pregnancy outcomes in cases without surgical sterilization were assessed until March 2021.This period refers to at least two years of life after the surgery.The time interval between the BHGAL surgery and the first pregnancy,the type of pregnancy (normal,miscarriage,abortion,or ectopic),the outcome of pregnancy,and complications of the third stage of labor were examined.Cases who could not get pregnant even though they had unprotected coitus with their partner for one year or more were considered secondary infertile.In women aged 35 and over,the limit time for unprotected coitus time was accepted as six months[11].
2.5.Statistical analysis
All data were analyzed using Statistical Package for Social Sciences(SPSS version 23.0,Chicago,IL,USA).The data distribution was analysed using either the Kolmogorov-Smirnov or Shapiro-Wilk test.Continuous variables are presented as mean±standard deviation (SD)or median [interquartile range (IQR)] depending on their normality.Categorical variables are presented as numbers and percentage (%).
2.6.Ethics approval
This is an observational study that was approved by the Dicle University Medical Faculty Ethics Committee for Non-interventional Studies (Approval No:34).Written or verbal consent was obtained from all participants in the study.
3.Results
3.1.Demographic and laboratory data analysis
The cases had a mean age of (30.7±6.0) years,with median gravidity and parity values of 5(4) and 3(2),respectively.Demographic and laboratory characteristics of the cases are listed in Table 1.
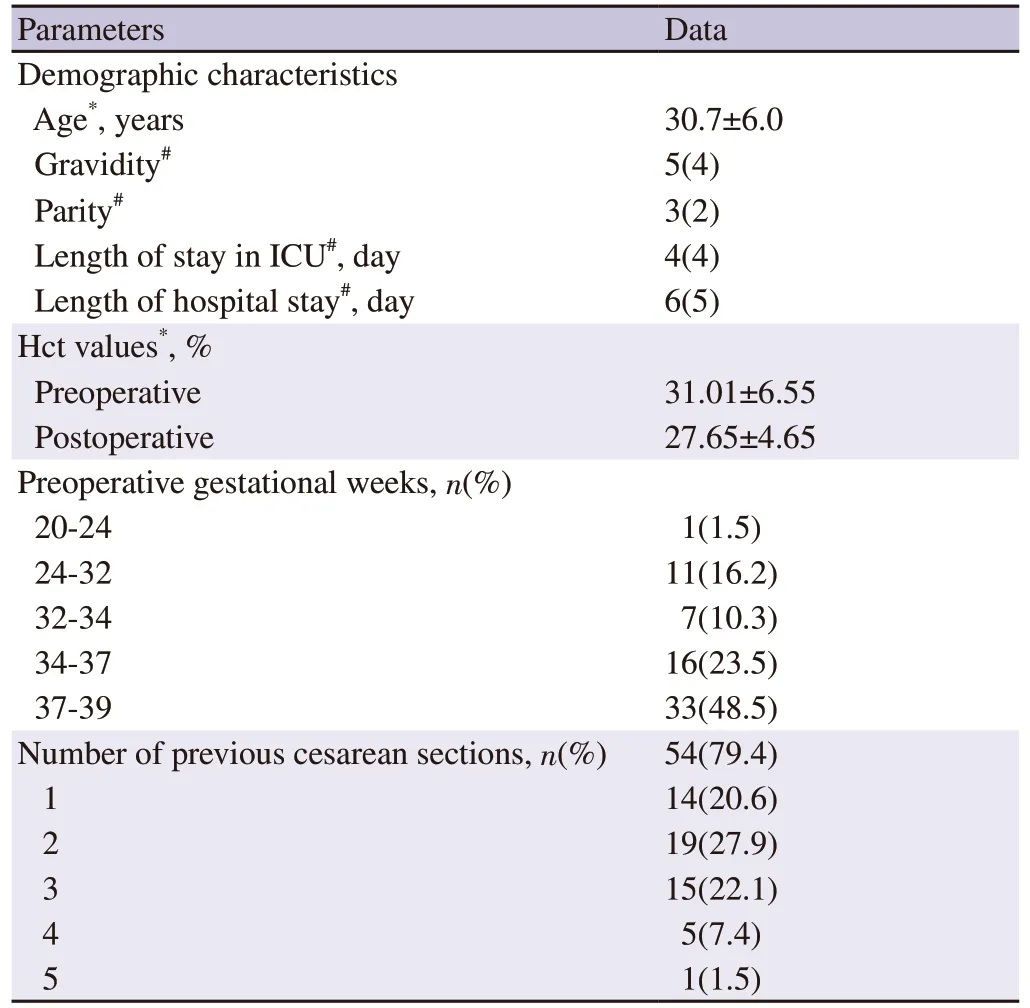
Table 1.Demographic and laboratory characteristics of the cases.
3.2.Analysis of clinical data
The BHGAL was performed in 61 patients (89.7%) during or after cesarean and in seven patients (10.3%) after vaginal delivery.The procedure was performed most frequently (69.1% andn=47)due to peripartum hemorrhage associated with the placenta accreta spectrum (PAS).Uterine artery ligation (64% andn=32)was the most preferred additional method to provide hemostasis.Disseminated intravascular coagulation and incision site infection were the most common postoperative complications,with equal rates of 31.3% (n=5).Massive blood transfusion (42.6% andn=29)was the most common surgery-related morbidity.General anesthesia was applied before the operation in half of the cases included in the study,while spinal anesthesia was applied in the other half.The clinical features of the cases are shown in Table 2.
3.3.Long-term fertility and pregnancy outcomes
Bilateral tubal ligation was applied to 31 cases (45.6%).Of 37 women who did not undergo surgical sterilization,70% (n=26)desired subsequent pregnancy.Six of these patients (23%) were diagnosed with secondary infertility.On the other hand,the fertility rate of the cases was found as 77% (n=20).The flowchart of the information about the analyzed data is given in Figure 1.
Five women had two pregnancy experiences.Postoperative pregnancies resulted in 15 term births,six preterm births,one stillbirth,and three abortions.The data of the first pregnancy after the operation and the second pregnancy,if any,of the patients are shown in Table 3.
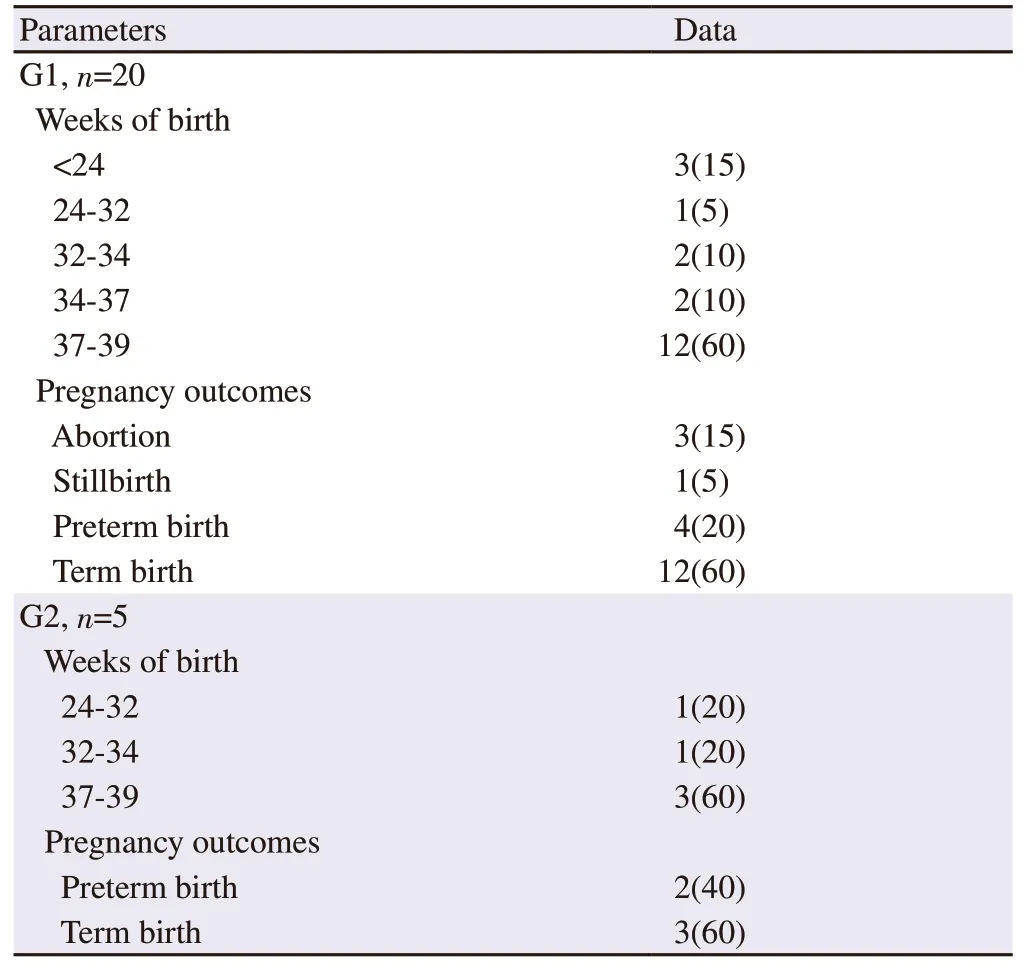
Table 3.Subsequent pregnancy outcomes of the cases.
4.Discussion
Obstetricians should follow the algorithms for hemostatic management during critical obstetric hemorrhages and use appropriate intervention strategies.Surgical intervention should be considered in cases with severe PPH in which medical treatments and conservative methods cannot be successful[1,12].At this point,the effectiveness of pelvic vascular ligation procedures in bleeding control should not be underestimated.Although it is a good option for PPH control,it remains unclear whether this surgery can be safely performed in young and low-parity women who demand fertility preservation or whose fertility will need to be preserved.The rate of cases with secondary infertility in our study was found to be higher than the studies in the literature.However,the fertility rate is consistent with the studies,and the rate of women who can become pregnant after surgery is higher than in cases with secondary infertility[7,8].
In a series,it was stated that 23 women had a desire for pregnancy in the following years after the surgery,and 20 of these women(86.9% fertility rate) were able to get pregnant[7].A total of 45 live-term births were reported.Nizardet al[6] also evaluated women who underwent BHGAL for severe PPH between 1989 and 2001.According to their data,all the women who had a desire for pregnancy were able to get pregnant within the first year after the operation.Secondary infertility was not detected in any of the cases.Thirteen of the pregnancies resulted in term delivery,two of them resulted in ectopic pregnancy,three of them with spontaneous abortion,and three of them with medical abortion,and they stated that a total of 21 pregnancies.Pappet al[13] evaluated 37 patients who underwent therapeutic or prophylactic BHGAL for obstetric indication and detected pregnancy in four of 13 cases.All these pregnancies healthily had reached the term,and the deliveries happened without any problems.No complications also were encountered in the subsequent term deliveries of the cases in our study.
Gizzoet al[8] evaluated the effects of hemostatic surgical techniques applied in PPH on fertility rates and pregnancy outcomes in women by examining the 15-year literature (9 studies) in their systematic review.According to the results,fertility rates vary between 50%-100%.
In this study,only 38.2% of the women had the desire to conceive after the operation,and there were no women who had experienced more than two pregnancies.This situation is probably due to the adverse psychological effects of intensive care and heavy treatment process,and severe obstetric hemorrhage on patients.As a matter of fact,in the study of Tanet al[14],the fear of being pregnant again in the future was found to be higher in those with a history of complicated pregnancy or birth.Providing psychological support to patients may be beneficial,but more research is needed on this subject.
The most common cause of PPH is uterine atony,which progresses with failure of myometrial contractions.Today,5% of deliveries are complicated by uterine atony[15].In many of the previous studies,the most common obstetric indication for BHGAL was uterine atony bleeding[4,8].With the rate of cesarean section reaching from 15%to 50% in the last 20 years in Turkey,it seems that PAS will replace uterine atony,which has a critical role in the etiology of obstetric hemorrhages.Most of our cases (79.4%) had a history of previous cesareans.Hypogastric artery ligation was performed in 69.1% of the cases due to PAS-related bleeding and 17.6% of uterine atony bleeding,and these data associated with the rising ratio of cesareans in our country.Icenet altouched upon this issue in a study they conducted and stated that PAS had become the leading cause of BHGAL[5].Furthermore,it may be advantageous to use pelvic devascularization surgeries such as BHGAL in PAS cases to reduce perioperative blood loss[16].
There are some limitations of the study.The fact that the study was conducted during the COVID-19 outbreak prompted us to change the study's methodology to prevent viral contamination.Due to the use of retrospective data,the phone numbers of some cases in the hospital records could not be reached.Fertility can be affected by many factors (age,previous surgeries,ovarian reserve,co-morbidities,etc.),which may have changed the result of the study.Cases with secondary infertility could not be evaluated in this respect.
In conclusion,due to the relatively high fertility rates after surgery,BHGAL is still the preferred pelvic vascular ligation procedure for young or low-parity women with severe PPH.We think this surgery does not affect fertility and pregnancy outcomes,but cohort studies with more significant numbers of patients are needed.
Conflict of interest statement
All authors declare no conflicts of interest.
Funding
The study received no extramural funding.
Authors’ contributions
Gulcan OKUTUCU performed manuscript writing,data collection,and data analysis.Mehmet Siddik EVSEN carried out project development,visualization,reviewing,and editing.Nurullah PEKER performed literature search,reviewing,and editing.Senem YAMAN TUNC was responsible for literature search,and project development.Mehmet Sait ICEN performed literature search,data collection,and project development.
 Asian Pacific Journal of Reproduction2024年1期
Asian Pacific Journal of Reproduction2024年1期
- Asian Pacific Journal of Reproduction的其它文章
- Engineering of ovarian tissue for ovarian dysfunctions: A review
- Exploring the relationship between ambient sulfur dioxide and semen quality parameters: A systematic review and meta-analysis
- The relationship between DNA fragmentation and the intensity of morphologically abnormal human spermatozoa
- Pro-fertility effect of Ficus carica fruit extract in streptozotocin-induced male rats
- Adding chitosan nanoparticles of green tea extract in diluent and thawing temperatures ameliorate the post-thawed quality of Boer buck semen
