Multimorbidity and mortality among older patients with coronary heart disease in Shenzhen,China
Fu-Rong LI,Shuang WANG,Xia LI,Zhi-Yuan CHENG,Cheng JIN,Chun-Bao MO,Jing ZHENG,✉,Feng-Chao LIANG,✉,Dong-Feng GU,4,✉
1. Shenzhen Key Laboratory of Cardiovascular Health and Precision Medicine,Southern University of Science and Technology,Shenzhen,Guangdong,China;2. School of Public Health and Emergency Management,Southern University of Science and Technology,Shenzhen,Guangdong,China;3. Shenzhen Health Development Research and Data Management Center,Shenzhen,China;4. School of Medicine,Southern University of Science and Technology,Shenzhen,Guangdong,China
ABSTRACT BACKGROUND The current understanding of the magnitude and consequences of multimorbidity in Chinese older adults with coronary heart disease (CHD) is insufficient.We aimed to assess the association and population-attributable fractions (PAFs)between multimorbidity and mortality among hospitalized older patients who were diagnosed with CHD in Shenzhen,China.METHODS We conducted a retrospective cohort study of older Chinese patients (aged ≥ 65 years) who were diagnosed with CHD.Cox proportional hazards models were used to estimate the associations between multimorbidity and all-cause and cardiovascular disease (CVD) mortality.We also calculated the PAFs.RESULTS The study comprised 76,455 older hospitalized patients who were diagnosed with CHD between January 1,2016,and August 31,2022.Among them,70,217 (91.9%) had multimorbidity,defined as the presence of at least one of the predefined 14 chronic conditions.Those with cancer,hemorrhagic stroke and chronic liver disease had the worst overall death risk,with adjusted HRs (95% CIs) of 4.05 (3.77,4.38),2.22 (1.94,2.53),and 1.85 (1.63,2.11),respectively.For CVD mortality,the highest risk was observed for hemorrhagic stroke,ischemic stroke,and chronic kidney disease;the corresponding adjusted HRs (95% CIs) were 3.24 (2.77,3.79),1.91 (1.79,2.04),and 1.81 (1.64,1.99),respectively.All-cause mortality was mostly attributable to cancer,heart failure and ischemic stroke,with PAFs of 11.8,10.2,and 9.1,respectively.As for CVD mortality,the leading PAFs were heart failure,ischemic stroke and diabetes;the corresponding PAFs were 18.0,15.7,and 6.1,respectively.CONCLUSIONS Multimorbidity was common and had a significant impact on mortality among older patients with CHD in Shenzhen,China.Cancer,heart failure,ischemic stroke and diabetes are the primary contributors to PAFs.Therefore,prioritizing improved treatment and management of these comorbidities is essential for the survival prognosis of CHD patients from a holistic public health perspective.
Cardiovascular disease (CVD),specifically coronary heart disease (CHD),continues to hold the highest position in terms of recorded fatalities on a global scale.In 2019,approximately 17.9 million deaths,which was equivalent to 32% of all global deaths,were attributed to CVD.[1]This figure is expected to surpass 23 million by the year 2030,leading to substantial financial burdens in terms of healthcare costs and reduced productivity.[2]With the prevalence of CHD and the accumulation of comorbidities both rising as individuals grow older,a substantial proportion of CHD patients are older adults who present with multiple concurrent chronic conditions,namely multimorbidity.In fact,older patients hospitalized with CHD face an increased risk of mortality when they have accompanying cardiovascular and or non-cardiovascular comorbidities such as hypertension,diabetes,heart failure,and stroke,among others.[3]
A comprehensive investigation on comorbidities would help inform the development of tailored secondary prevention strategies for the CHD population.Several prior studies of western populations have examined the occurrence of multimorbidity among individuals with CHD and have found that the presence of different comorbidities,either independently or in combination,was linked to an increased risk of mortality.[4-6]However,given the disparities in disease susceptibility among ethnic groups,socioeconomic disparities,and lifestyle variations,it is imperative to thoroughly investigate the comorbidities associated with CHD in mainland China.Also,few studies have focused on Chinese older adults and the impact of clustering multiple chronic conditions,both cardiovascular and non-cardiovascular,on long-term survival remains insufficiently understood.Therefore,there is a pressing need to gain a comprehensive understanding of the collective burden of comorbidities and its influence on mortality among older patients with CHD in China.
In this study,we analyzed data from hospitalized Chinese patients aged 65 or older diagnosed with CHD to investigate the following aspects: (1) the associations of specific comorbidities,their combined impact,and patterns of clustering,with the risk of mortality from all cause and CVD cause;(2) the adjusted population-attributable fractions (PAFs) indicating the proportion of mortality attributed to different comorbidity status.[7,8]
METHODS
Study Population
Shenzhen,an urban agglomeration of significant industrial and economic importance located in the southern Guangdong province of China,is inhabited by a migrant population surpassing 20 million.To address the challenge of enhancing the quality and efficiency of healthcare services for this population,the municipal government launched the Population Health Informatization Project in 2016.The project's objective was to standardize the collection and integration of all health-related data,encompassing primary care,hospital records,and chronic disease management systems.
In this study,the data were subjected to rigorous quality assurance procedures overseen by expertly trained data engineers,and subsequently,the data was securely stored at the National Supercomputing Center located in Shenzhen.Specifically,for the purpose of our investigation,we obtained data from the inpatient information platform,which included comprehensive diagnostic information classified according to the International Classification of Diseases 10threvision (ICD-10),as well as demographic and vital information from resident health records and death registration,respectively.Our research focused on older patients (aged ≥ 65 years)with diagnosed CHD who were admitted to hospitals between January 1,2016,and August 31,2022.CHD was identified using the ICD-10 codes I20-I25,encompassing angina,acute myocardial infarction,chronic ischemic heart disease,and other related conditions.To maximize the follow-up time,only the initial admission with CHD was considered in case multiple admissions were recorded.Multimorbidity was defined as a history of one or more of predefined chronic conditions.Participants’ mortality status was tracked until a censoring date of September 1,2022,using data from the Chinese Center for Disease Control and Prevention (CDC).This allowed for a maximum observed follow-up period of 6.7 years(with a median of 2.7 years and an interquartile range of 1.1-4.3 years).ICD-10 codes were also used to identify the causes of death,and CVD mortality was defined as ICD-10 codes I00-I99.
Definition of Chronic Condition
The following chronic conditions were used as the comorbidity in the present study: atrial fibrillation,cardiomyopathy,heart failure,hypertension,hemorrhagic stroke,ischemic stroke,pulmonary heart disease,valvular heart disease,chronic kidney disease,chronic liver disease,chronic obstructive pulmonary disease (COPD),emphysema or chronic bronchitis,cancer,diabetes,and inflammatory arthropathies.Detailed ICD-10 codes for the abovementioned chronic conditions are provided in Supplementary Table S1.
Statistical Analysis
The baseline characteristics were summarized according to vital status using percentages and numbers for categorical data,and medians with interquartile ranges for continuous variables.To compare differences in baseline characteristics among predefined groups,appropriate statistical tests,such as the chi-squared test,the Mann-WhitneyUtest,or the Kruskal-Wallis test,were employed based on the specific characteristics of the analyzed data.
Cox proportional hazard models were utilized to assess the hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause mortality and CVDcause mortality associated with predefined chronic condition(s).The proportionality assumption was checked using Schoenfeld residual methods,and there was no obvious evidence of the violation of the proportionality assumption.In this study,the Cox models were adjusted for age,sex,marital status (not married,married and divorced/other),year of admission,and further adjusted for remaining individual chronic condition,where appropriate.We also explored the association by grouping the studied sample according to the accumulation of chronic conditions (grouped into 0,1-3,and ≥ 4).Furthermore,we calculated the adjusted PAFs to determine the percentage of mortality that could be prevented if each specific chronic condition or condition group was eliminated.The PAFs provide an estimate of the proportion of disease cases (in this case,death)that could be avoided by addressing the risk factors.[7,8]Specifically,the PAF was calculated using the formula as follows:×100%,wherePerepresents the proportion of the specific exposure (i.e.,the comorbidity status).
We also utilized latent class analysis to consolidate multiple chronic conditions into multimorbidity phenotype.The latent class analysis focused solely on the probability distributions of the chronic conditions and did not incorporate outcomes.This approach was preferred over simpler methods,such as creating a cumulative score for the health conditions,as it allowed for a more detailed examination of specific combinations of conditions.[9]Analyzing all possible combinations of conditions was avoided due to the increased risk of false positive findings(type I errors) and decreased statistical power.As such,in the present study,we used a multimorbidity phenotype resulted in 3 classes based on the model fit statistics for latent class solutions (Supplementary Table S2).Specifically,the first group,labeled as class 1,demonstrated a low level of multimorbidity,with the most common conditions being cancer,chronic liver disease,and COPD,etc.The second group,class 2,exhibited a moderate level of multimorbidity,characterized by chronic kidney disease,diabetes,and both hemorrhagic and ischemic strokes as the most prevalent conditions.Finally,the third group,class 3,displayed a high level of multimorbidity,with atrial fibrillation,valvular heart disease,pulmonary heart disease,and cardiomyopathy as the predominant conditions in this cluster(Supplementary Figure S2).
We also conducted additional analyses specifically focusing on individuals diagnosed with acute coronary syndrome (ACS),encompassing unstable angina (I20.0),ST-segment elevation myocardial infarction (STEMI,I21.0-I21.3),and non-ST-segment elevation myocardial infarction (NSTEMI,I21.4).[10]This was undertaken due to ACS representing the acute manifestation of CHD,which is anticipated to result in less favorable prognoses compared to other forms of chronic ischemic heart disease.
All statistical tests were conducted using a twosided approach,and a significance level ofP< 0.05 was utilized to determine statistical significance.The statistical analyses were performed using the following software packages: Stata MP version 14(http://www.stata.com/),R version 4.1.2 (https://cran.r-project.org/),and Mplus version 7.3 (https://www.statmodel.com/).
RESULTS
Prevalence of Chronic Conditions and Participants’ Characteristics
Included were 76,455 hospitalized older patients with diagnosed CHD through Jan 1,2016 and August 31,2022.The majority of patients (91.9%) had multimorbidity,with a maximum of 8 conditions.Hypertension (n=52,426,68.6%),heart failure (n=29,804,39.0%),and diabetes (n=25,713,33.6%) emerged as the most prevalent conditions.It is also noteworthy that a considerable percentage of patients diagnosed with chronic kidney disease,hemorrhagic stroke and pulmonary heart disease had additional comorbidities (98.16%,96.66%,and 96.38%,respectively).Chronic liver disease,hemorrhagic stroke and cardiomyopathy were the least prevalent (Table 2).
Compared with participants who were alive during follow-up,those who died tended to be older,male sex,and are generally more likely to have heavier burden of chronic conditions (Table 1).Characteristics of included participants by multimorbidity phenotype are also summarized in Supplementary Table S3.Overall,participants appeared to be older from class 1 to class 2 and 3.
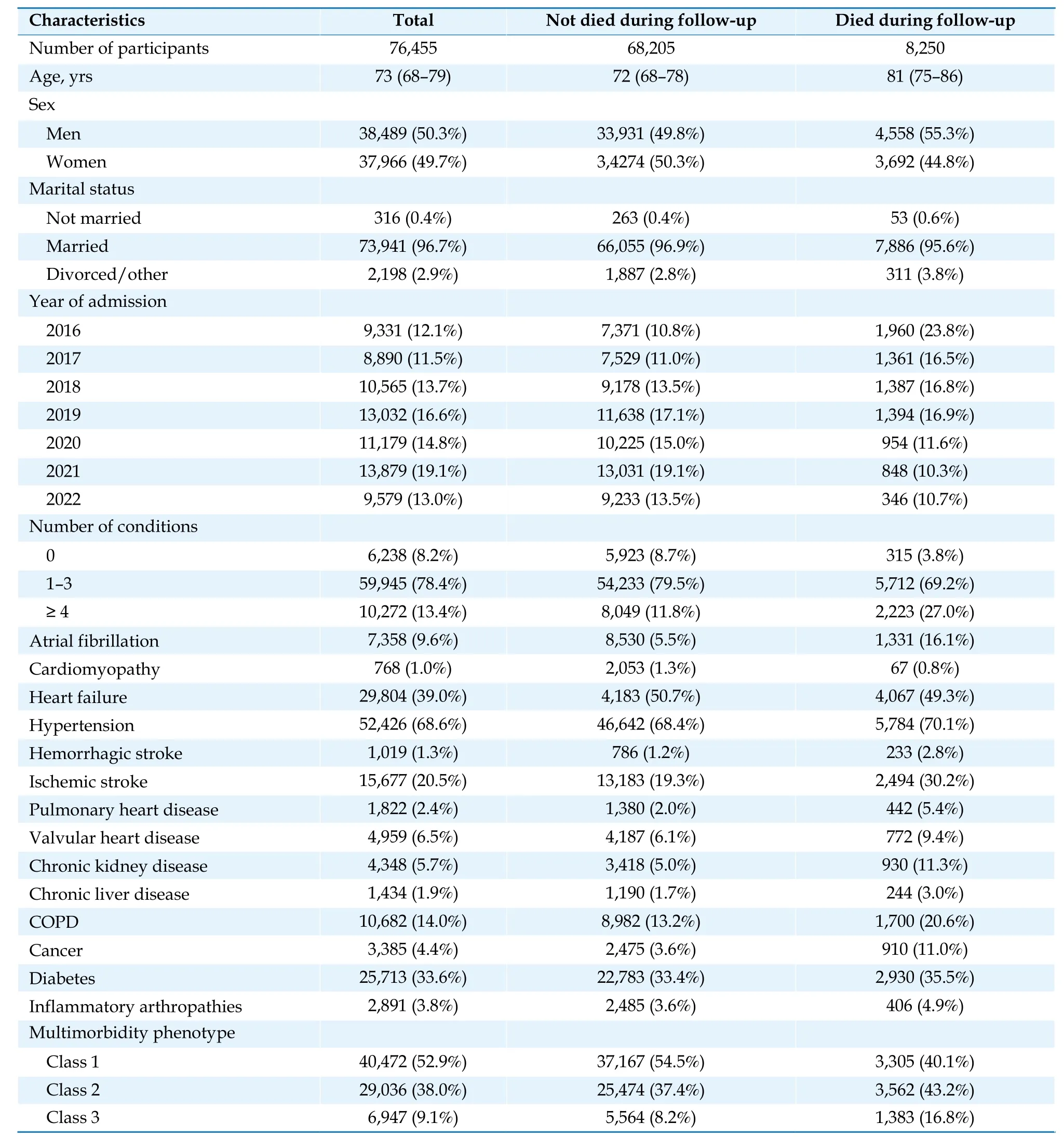
Table 1 Baseline characteristics between participants who survived and those who died during follow-up.

Table 2 Percentage of difference diseases by comorbidity status*.
Association of Chronic Conditions with Mortality
During a median follow-up of 2.7 years,a total of 8,250 participants died,of whom 3,989 (48.4%) were died from CVD cause.The number of participants with individual chronic condition,mortality rates and time to death are presented in Supplementary Table S4.
Cancer,hemorrhagic stroke,and chronic liver disease had the worst overall death risk,with adjusted HRs (95% CIs) of 4.05 (3.77-4.38),2.22 (1.94-2.53) and 1.85 (1.63-2.11),respectively,followed by chronic kidney disease (HR=1.76;95% CI: 1.64-1.89),and pulmonary heart disease (HR=1.67;95% CI: 1.51-1.84).For CVD mortality,the highest risk was observed for hemorrhagic stroke,ischemic stroke,and chronic kidney disease;the corresponding adjusted HRs (95% CIs) were 3.24 (2.77-3.79),1.91 (1.79-2.04),and 1.81 (1.64-1.99),respectively.
With each additional chronic condition,the risk of all-cause mortality increased by 29% (HR=1.29;95% CI: 1.27-1.32),and the risk of CVD-cause mortality increased by 41% (HR=1.41;95% CI: 1.38-1.44).Compared with those without multimorbidity,those with 1-3 conditions and ≥ 4 conditions had adjusted HRs (95% CIs) of 1.49 (1.33-1.67) and 2.79(2.48-3.15),respectively;the corresponding HRs(95% CIs) were relatively higher for CVD-cause mortality,specifically 2.22 (1.81-2.72) and 4.82 (3.92-5.93),respectively.With regard to multimorbidity phenotype,compared with class 1,those with class 2 and class 3 respectively had adjusted HRs (95% CIs) of 1.37 (1.30-1.44) and 1.82 (1.71-1.94) for allcause mortality;for CVD-cause mortality,the corresponding HRs (95% CIs) were 2.12 (1.98-2.28) and 2.86 (2.61-3.13),respectively (Figure 1).
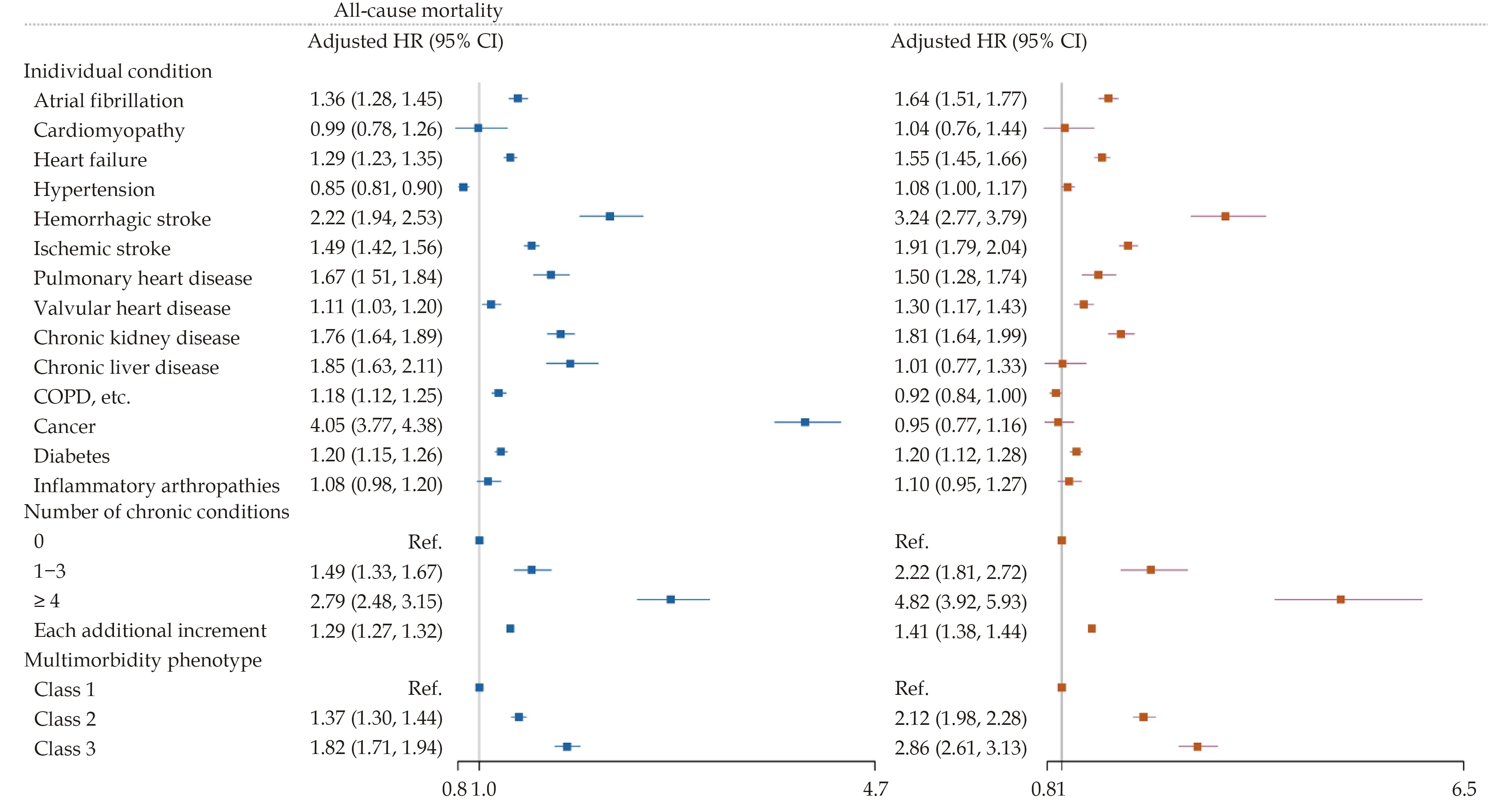
Figure 1 Adjusted HRs for all-cause mortality and CVD-cause mortality associated with different chronic conditions and multimorbidity phenotype among older Chinese patients who were admitted with CHD between January 1,2016,and August 31,2022 in Shenzhen,China. CHD: coronary heart disease;COPD: chronic obstructive pulmonary disease;CVD: cardiovascular disease.Models were adjusted for age,sex,marital status,year of admission,and further adjusted for remaining individual chronic condition,where appropriate.Class 1 showed low multimorbidity,with prevalent chronic conditions like cancer,chronic liver disease,and COPD et al.Class 2 had moderate multimorbidity,with chronic kidney disease,diabetes,and both hemorrhagic and ischemic strokes.Class 3 had high multimorbidity,primarily with atrial fibrillation,valvular heart disease,pulmonary heart disease,and cardiomyopathy.
PAFs for Chronic Conditions and Mortality
All-cause mortality was mostly attributable to cancer,heart failure,and ischemic stroke,with PAFs of 11.8,10.2,and 9.1,respectively.As for CVDcause mortality,however,the leading PAFs were heart failure,ischemic stroke,and diabetes;the corresponding PAFs were 18.0,15.7,and 6.1,respectively.In the overall status of chronic conditions,compared with those without predefined chronic condition,those with 1-3 chronic conditions had a PAF of 28.5 for all-cause mortality and 49.4 for CVDcause mortality;however,those with ≥ 4 chronic conditions had lower levels of PAF,with PAF of 19.8 for all-cause mortality and 34.0 for CVD-cause mortality.For multimorbidity phenotype,those who were categorized as class 2 had a PAF of 12.4 for overall death and 29.5 for CVD death,while the corresponding values for class 3 were respectively 6.9 and 14.2,in comparison to class 1 (Figure 2).
Supplementary Analysis
In a supplementary analysis,we limited the study sample to individuals who received a diagnosis of ACS (n=16,022).Our findings revealed that the associations between comorbidities and both all-cause and CVD-cause mortality were consistent with the results observed within the broader CHD cohort (Supplementary Figure S3).Furthermore,among those with ACS,the PAFs for each comorbidity status in relation to mortality remained largely similar to those observed in CHD patients (Supplementary Figure S4).
DISCUSSION
In this study involving older Chinese patients(aged ≥ 65 years) who were hospitalized with CHD,it was found that nearly 91.9% of them had multimorbidity,with hypertension,heart failure,and diabetes being the most common.The presence of one additional chronic condition increased the likelihood of overall death by 29% over the follow-up period of 6.7 years.Through latent class analysis,three distinct patient groups were identified based on their probability of having comorbidities,each exhibiting different survival outcomes.Restricting the study sample to those with ACS yielded similar results to the original analyses.
Given the aging population and the improvement of cardiovascular healthcare,the global population's demographic landscape has undergone significant changes,resulting in a large number of older patients with CHD who also have multiple coexisting chronic conditions.[11]In China and the United States,there are respectively approximately 94 million and 86 million individuals living with CVD,primarily among older adults with multimorbidity.[12,13]As a consequence,healthcare utilization and associated costs are substantial and increase as the number of co-existing conditions rises.[14,15]Therefore,one of the primary global healthcare priorities is to decrease adverse health outcomes associated with multimorbidity and enhance long-term survival.However,previous studies addressing multimorbidity have either focused on individual conditions or have predominantly utilized relatively small sample data with short-term outcomes.[6,16-20]Our study provides a comprehensive understanding of the burden of multimorbidity,individually or in combination,among a large sample of Chinese older patients with CHD within a modern healthcare system with a relatively long-term follow-up.
We observed that patients who experienced CHD and had a history of cancer (for overall death only)had the most unfavorable survival prognosis.To our knowledge,very few studies have identified the death outcome resulting from cancer in combination with other co-existing health conditions among CHD patients.Over recent years,cardio-oncology has garnered significant attention due to the potential association between cancer diagnosis and increased risk of CVD,and vice versa.[21]Our study revealed that,however,the presence of cancer was linked to a higher risk of all-cause mortality,but it did not significantly contribute to mortality attributed to CVD.These findings suggest that cancer itself may serve primarily as a prognostic indicator for overall survival,rather than a key factor impacting the clinical prioritization of cancer-CVD-related deaths.We also found that patients with cerebrovascular disease,chronic liver disease,and chronic kidney disease also experienced notably poor survival.In China,chronic liver disease,including chronic hepatitis B virus infection and nonalcoholic fatty liver disease is one of the major cause of morbidity and mortality.[22]The poor survival prognosis regarding chronic liver disease in our cohort study underscores the importance of considering this disease within the clinical framework,even among patients with CHD.The magnitudes of the associations of cerebrovascular disease and chronic kidney disease with mortality were comparable with those in previous studies.For example,in a study of about 600,000 patients with acute myocardial infarction in England and Wales,researchers found cerebrovascular disease and chronic renal failure to be associated with an approximately 70% higher risk of overall death.[4]However,this study did not focus on older patients and only included a limited number of individual comorbidities (n=7) and did not investigate the results for CVD-cause mortality.
In our study,we additionally calculated the PAFs to estimate the proportion of preventable deaths that could be attributed to avoiding the specific comorbidities,assuming a causal relationship based on the observed associations.Generally,heart failure,ischemic stroke,and diabetes demonstrated the greatest impact for both overall death and CVD related death.Meanwhile,the presence of multimorbidity was found to contribute to an overall PAF of> 48.3%.The observed high PAFs in our study can be attributed not only to the strength of the associations but also to the prevalence of the chronic condition(s).Indeed,in our study,the prevalence of heart failure,ischemic stroke,and diabetes were respectively 39.0%,20.6% and 33.6%;which partly explained the high PAFs for these conditions.It is well documented that CHD is one of the most frequent causes of heart failure,[23]while ischemic stroke and diabetes are one of the most common cardiometabolic comorbidities in Chinese.[24]Our study may indicate that,from the perspective of the whole population,clinical and community healthcare professionals should continuously enhance their efforts in the prevention and treatment/management of these three important comorbidities in older Chinese patients with CHD.
It is also noteworthy that,to explore all possible combinations of chronic conditions and determine if distinct multimorbidity phenotypes exist,we also utilized latent class analysis,a data-driven technique.This approach revealed three distinct prognostic groups,referred to as “computational phenotypes”,which were significantly different based on the diseases present.[9]Understanding the characteristics of these multimorbidity phenotypes may offer potential directions for future investigations into the development of novel pharmaceutical interventions and healthcare services tailored to the needs of those at the highest risk.
Limitations and Strengths
Our study has some strengths,which include the prospective study design and the uniquely large sample size of older patients with CHD.The linkage with death registers also minimized the number of patients who were lost to long-term followup.The utilization of PAFs can portray the proportion of deaths that could have been prevented or delayed through the modification and management of comorbidities.Despite these strengths,there were some limitations in our study.Firstly,our study was observational in nature,limiting our ability to establish causation.Secondly,certain essential patient-related variables among older adults,such as functional status and cognitive impairment,were not available.This could have introduced confounding influencing the observed associations.
Conclusions
The presence of multimorbidity was common and had a significant impact on mortality among older patients with CHD in Shenzhen,China.Cancer,heart failure,ischemic stroke and diabetes are the primary contributors to PAFs.Therefore,prioritizing improved treatment and management of these comorbidities is essential for the survival prognosis of CHD patients from a holistic public health perspective.
DISCLOSURE
Fundings
This study was supported by the National Natural Science Foundation of China (Grants 12126602),the R&D project of Pazhou Lab (Huangpu) under Grant 2023K0610,the National Natural Science Foundation of China (Grants 82030102),the Shenzhen Medical Academy of Research and Translation(Grants C2302001),the Shenzhen Science and Technology Innovation Committee (No.ZDSYS20200810 171403013),the Chinese Postdoctoral Science Foundation (No.2022M721463),the SUSTech Presidential Postdoctoral Fellowship,and the Ministry of Science and Technology of China (Grants 2022YFC 3702703).The funders had no role in the study design,management,analysis,interpretation,manuscript preparation,review,and approval.The funders had no role in the study design,management,analysis,interpretation,manuscript preparation,review,and approval.
Conflict of Interest
None.
Author contributions
Dongfeng Gu and Jing Zheng directed the study.Furong Li analyzed the data and wrote the manuscript.Shuang Wang,Fengchao Liang,Xia Li,Zhiyuan Cheng,Cheng Jin,and Chunbao Mo contributed to the discussion and reviewed/edited the manuscript.All authors contributed to the article and approved the submitted version.
 Journal of Geriatric Cardiology2024年1期
Journal of Geriatric Cardiology2024年1期
- Journal of Geriatric Cardiology的其它文章
- Relationship between mitochondrial respiratory dysfunction of blood mononuclear cells and heart failure severity
- Diagnostic performance of intravascular ultrasound-based fractional flow reserve in evaluating of intermediate left main stenosis
- Effect of cytochrome P450 2C19 (CYP2C19) gene polymorphism and clopidogrel reactivity on long term prognosis of patients with coronary heart disease after PCI
- Influencing Factors on Cardiovascular Health in China
- Development and validation of a model integrating clinical and coronary lesion-based functional assessment for longterm risk prediction in PCI patients
- Interaction between systemic iron parameters and left ventricular structure and function in the preserved ejection fraction population: a two-sample bidirectional Mendelian randomization study
