Relationship between mitochondrial respiratory dysfunction of blood mononuclear cells and heart failure severity
Viacheslav A. Korepanov,Tariel A. Atabekov,Tatiana Yu. Rebrova,Roman E. Batalov,Sergey A. Afanasiev
Cardiology Research Institute,Tomsk National Research Medical Center,Russian Academy of Sciences,Tomsk,Russia
Chronic heart failure (CHF) is a clinical syndrome manifested by reduced pumping ability of the heart,increased pressure in heart chambers in both physical activity and at rest.The symptoms of this syndrome are dyspnea,undue fatigability,peripheral edema,which follow structural and functional changes of the myocardium.[1]The growing incidence of CHF,especially among elderly people,is an urgent problem for medicine in the vast majority of industrialized countries.For instance,in Russian Federation,CHF is diagnosed in about 7% of cardiovascular patients.At the same time,this indicator varies from 0.3% in young people(20-29 years old) to 70% in the older age group.[2,3]A similar trend has been observed in other countries.[4]A wide range of factors influence the development,course,and severity of CHF: systolic function of the heart ventricles,the intensity of myocardial remodeling,the level of biochemical markers of heart failure (NT-proBNP,galectins,matrix metalloproteinases etc.).[5,6]
It is established that intracellular mechanisms involved in the process of electromechnical coupling of cardiomyocyte are highly energy depended,[7]and CHF is characterized by a disturbance of intracellular energy metabolism.[8]Mitochondrial dysfunction is known as one of the key mechanisms mediating myocardial dysfunction at the cellular level in CHF.It is manifested by both reduced ATP synthesis and increased reactive oxygen species production.[9]However,the opportunity of direct study of cardiac mitochondria is not always possible,since the material can only be obtained by biopsy.Increasingly,peripheral blood mononuclear cells (PBMC) are used to study mitochondrial function.[10]It has been shown that respiratory function of PBMC mitochondria significantly decreased with the development of heart failure.[11]However,there is no data on the severity of mitochondrial dysfunction of PBMC in CHF and its impact on the prognosis of the underlying disease.
The aim of this study was to assess the state of the respiratory function of PBMC mitochondria in patients with CHF of ischemic origin.A total of 37 patients (27 men (72.9%) and 10 women (27.1%)) diagnosed with I-III CHF NYHA functional class (FC)were included in the study (Table 1).Ischemic etiology of CHF was confirmed by a diagnosis of coronary artery disease (stenosis of one or more coronary arteries ≥ 50%) and/or a history of myocardial infarction or revascularization.Exclusion criteria were followed: age under 18 years,a history of myocardial infarction earlier than 3 months ago,CHF of 0 and IV NYHA FC,severe comorbidity,indications for heart transplantation,cognitive disturbances.The study protocol was approved by the local ethical committee of the Cardiology Research Institute,Tomsk National Research Medical Center (protocol No.219 of 10.26.2021).All patients signed an informed consent prior to the enrollment in the study.
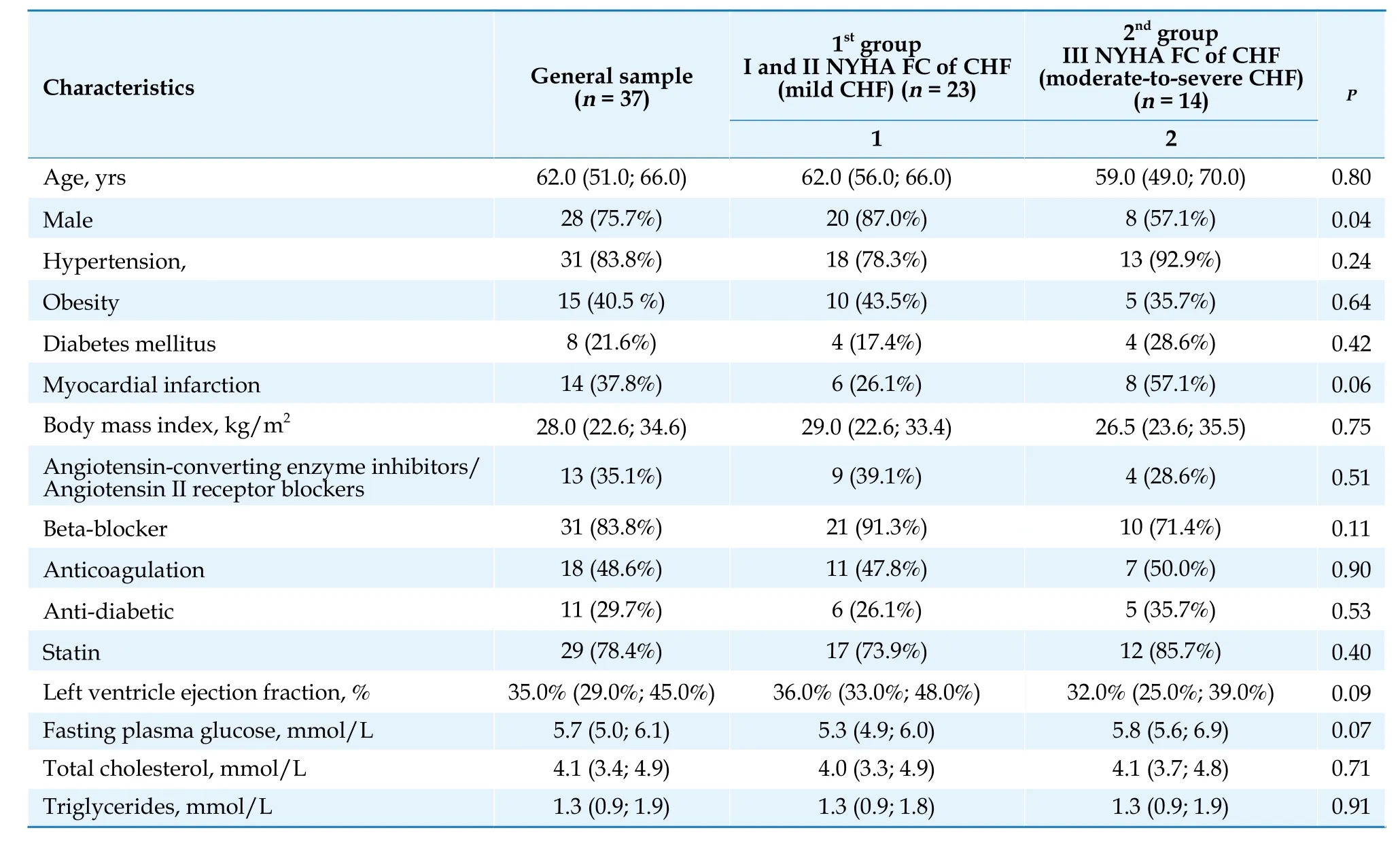
Table 1 Baseline characteristics of patients with chronic heart failure by NYHA functional class.
To obtain PBMC for the study of mitochondrial function,all patients were taken 9 mL of venous blood into a vacutainer with EDTA anticoagulant.PBMC fraction was isolated on a Histopaque -1077 density gradient (Sigma).Resulting cell ring was washed in PBS solution (Sigma).The cell pellet was lysed in hyposmolar sucrose medium (0.25 mol/L sucrose with EDTA) by soft pipetting.Mitochondria released into solution were isolated by differential centrifugation in sucrose medium.[12]The resulting mitochondria pellet was resuspended in the minimum volume of 0.25 mol/L sucrose medium for further analysis.
Respiratory function of isolated mitochondria was assessed according following parameters: V3-phosphorylating respiration,oxygen consumption rate (OCR) in a medium containing of oxidation substate(s) (pyruvate+malate;succinate),phosphorylation substrate (200 µmol/L of ADP),and oxygen;V4-non-phosphorylating respiration,OCR in a medium after ADP is depleted;RCC -respiratory control coefficient,which is the ratio of phosphorylating and non-phosphorylating rates -V3/V4.[12]
The activity of oxygen consumption by mitochondria was measured in pre-oxygenated incubation medium of the following composition (in mmol/L):sucrose -250.0;KCl -10.0;KH2PO4-5.0;MgCl2-1.25;HEPES -5.0;pyruvate -6.0+malate -8.0;succinate -5.0;pH=7.35-7.40.The measurements were carried out in a thermostated cell (25-27 °С)with a volume of 1 mL with constant stirring with a magnetic stirrer.The oxygen concentration in the medium was determined by a Clark electrode connected to an Expert -001 liquid analyzer (Ekoniks,Moscow).Oxygen consumption rates (V3and V4) are presented as nmol O2/min/mg of mitochondrial protein (MP).
All statistical analysis was performed with Statistica 10.0 software package,StatSoft (USA).The Shapiro-Wilk test was used to assess the normality of continuous variables.Quantitative data,the distribution of which was not normal,are presented as median (Me),upper (Q1) and lower (Q3) quartiles.Frequencies are presented as counts (n) and percentages(%).Pearson’s chi-squared test was used to compare the difference of frequencies between studied group.Mann-WhitneyU-test was used to compare the intergroup difference of continuous variables.Pvalue < 0.05 was considered statistically significant.
When calculating the parameters of mitochondrial respiration in the whole cohort of patients,it was found that V3OCR in pyruvate-malate and succinate incubation media was,respectively,136.0 (82.5;173.9) and 117.2 (68.7;178.3) nmol O2/min/mg MP.In V4metabolic state,OCR was 47.6 (30.3;68.0) and 41.6 (21.9;69.8) nmol O2/min/mg MP for pyruvatemalate and succinate incubation media,respectively.When used pyruvate and malate as oxidation substrates,the median value of RCC was 2.48 (2.09;2.69) relative units (RU).The similar values were obtained for succinate incubation medium -RCC was 2.59 (2.14;2.95) RU.
It is obvious,from the presented data,that the dispersion of parameters,especially for OCR in V3metabolic state,is quite wide.So that,the total sample was dividing into two groups according to the NYHA FC of CHF.The 1stgroup included patents with I and II NYHA FC of CHF (n=23) (mild CHF),and the 2ndgroup included patients with III NYHA FC of CHF (n=14) (moderate-to-severe CHF).
After dividing total sample into groups,it was revealed,that OCR in V3metabolic state in the 1stgroup was 141.3 (105.7;187.5) nmol O2/min/mg MP when using pyruvate-malate incubation medium.This value was 1.5 times (P=0.027) higher than in 2ndgroup where this parameter was 89.2 (26.8;138.4) nmol O2/min/mg MP.In V4metabolic state,when using pyruvate-malate incubation medium,OCR in the 1stgroup was 54.4 (36.1;87.0) nmol O2/min/mg MP,when in the 2nd-33.4 (14.7;47.4) (P=0.01) nmol O2/min/mg MP.
When using succinate incubation medium,mitochondrial OCR in both metabolic states also had significant intergroup differences.In V3metabolic state,it was 131.1 (74.2;196.2)vs.70.5 (36.1;119.0) nmol O2/min/mg MP (P=0.029) for 1stand 2ndgroup,respectively.In V4metabolic state,OCR was 44.3 (33.6;74.3) nmol O2/min/mg MP in the 1stgroup,and 26.5(17.8;41.9) nmol O2/min/mg MP in the 2ndgroup(P=0.014).
There were no intergroup differences in RCC.When using pyruvate-malate incubation medium,this parameter was 2.34 (2.00;2.65) and 2.53 (2.44;2.70) (Р=0.189) for the 1stand the 2ndgroup,respectively.Median values of RCC in succinate medium were 2.63 (2.14;2.95)vs.2.55 (2.00;3.38) (P=0.907)for the 1stand the 2ndgroup,respectively.
According to the results of the study,it was found that the conjugation of the processes of oxidation and phosphorylation in the mitochondria of PBMC in both groups of patients is below the accepted reference interval (3-5 relative units).[13]Also the obtained results indicate the relationship of PBMC mitochondria dysfunction with an increase in the NYHA functional class of CHF and worsening of the course of the disease.Thus,patients of the 2ndgroup with higher NYHA FC of CHF were characterized by a significant lower level of respiratory function of PBMC mitochondria than patients of the 1stgroup.
As shown in previous studies,a decrease in the respiratory function of mitochondria from cardiomyocyte and PBMC occurs simultaneously in patients with cardiovascular diseases,such as in ischemic heart disease,[14]which may result in CHF.[15]It is also known that in CHF (including ischemic genesis) the heart undergoes aseptic inflammation with the involvement of T-leukocytes and subsequent myocardial infiltration.[16]During the process of aseptic inflammation,damage and destruction of cardiomyocytes occur with the subsequent release of factors which can activate and increase the number of neutrophils passing through the bloodstream through the heart chambers[17]with progressive relative lymphocytopenia associated with both inflammation and down-regulation of the immune system.[18]Such the change in the number of peripheral blood leukocytes leads to a shift of the neutrophillymphocyte ratio towards neutrophils with a simultaneous decrease in the overall level of mitochondrial respiration of peripheral blood leukocytes.In the previous studies,it was revealed that neutrophil mitochondria contribute less to oxygen consumption compared to blood lymphocytes and monocytes.[19,20]
PBMC mitochondrial dysfunction could also be caused by circulating mitoDAMPs (mitochondrial damage-associated molecular patterns) such as mitochondrial DNA,IL-1b,NRLP3 which are released in general circulation from damaged cardiomyocytes.In initiate vicious circle: cardiomyocyte damage -> mitoDAMPs relese -> PBMC activation -> alteration of PBMC mitochondria respiration and parallel myocardial infiltration driving by chemoattractants from damaged cardiomyocytes -> further myocardial damage and remodeling.[21-23]
Simultaneously with the alteration of the respiratory function of mitochondria,in both myocardial cells and PBMC the level of reactive oxygen species increases due to disruption of the electron transport chain and electron leakage into the cytoplasm.[24,25]An increase in the level of reactive species is also associated with alteration of the antioxidant system.According to Li,et al.,[25]in HF patients with preserved ejection fraction,the activity of superoxide dismutase,the main antioxidant enzyme,was significantly lower compared to heathy individuals.It was also shown that the level of production of reactive oxygen species is significantly higher in patients with NYHA III FC of CHF than in individuals with NYHA I and II FC of CHF.[26]
The possible role of mitochondrial DNA polymorphisms in the development of mitochondrial dysfunction today remains under discussion.In the study of Golubenko,et al.,[27]it was shown that haplogroup H carriage may be a possible risk factor for severe CHF in individuals diagnosed with ischemic heart disease and a history of myocardial infarction.The carriage of substitutions that determine the mitochondrial DNA Haplogroup H mediates such changes in the encoded proteins of mitochondrial electron transport chain,leading to increased production of not only ATP,but also reactive oxygen species.[28,29]
The results of the study demonstrate that the conjugation of oxidative phosphorylation in PBMC mitochondria of patients with CHF of ischemic origin is below reference values independently the NYHA FC of CHF.At the same time,in patients with III NYHA FC of CHF,OCR of PBMC mitochondria is significantly almost two times lower than in patients with I and II NYHA FC of CHF.Based on these results,it could be concluded that the NYHA FC of CHF in patients with ischemic heart disease is directly related to the activity of mitochondrial respiration.The obtained data could also be interpreted for cardiomyocyte mitochondria,since even if PBMC mitochondria incubated without hypoxia condition and in the presence of a sufficient amount of oxidation substrates have reduced respiratory parameters,then the respiratory parameters of myocardial mitochondria are expected to be reduced.Therefore,we could expect that patients with worse respiratory function of mitochondria will have a greater risk of the development of complications of CHF course(decompensation,life-threatening arrhythmias).The study of the respiratory function of PBMC mitochondria,together with generally accepted diagnostic criteria,may be a promising approach for assessing and stratifying the adverse development of CHF of ischemic origin.
Conflict of interests
None.
 Journal of Geriatric Cardiology2024年1期
Journal of Geriatric Cardiology2024年1期
- Journal of Geriatric Cardiology的其它文章
- Diagnostic performance of intravascular ultrasound-based fractional flow reserve in evaluating of intermediate left main stenosis
- Multimorbidity and mortality among older patients with coronary heart disease in Shenzhen,China
- Effect of cytochrome P450 2C19 (CYP2C19) gene polymorphism and clopidogrel reactivity on long term prognosis of patients with coronary heart disease after PCI
- Influencing Factors on Cardiovascular Health in China
- Development and validation of a model integrating clinical and coronary lesion-based functional assessment for longterm risk prediction in PCI patients
- Interaction between systemic iron parameters and left ventricular structure and function in the preserved ejection fraction population: a two-sample bidirectional Mendelian randomization study
