Short and long term corneal biomechanical analysis after overnight orthokeratology
INTRODUCTION
Several studies have been conducted to evaluate the clinical outcomes and microstructural changes occurring after overnight orthokeratology (OK)
. This scientific evidence shows the efficacy and safety of this type of corneal refractive treatment
. However, the scientific evidence of changes occurring in the mechanical properties of the cornea with OK is still limited and showing even contradictory outcomes
. Whereas some authors have concluded in different studies that OK alters some corneal biomechanical properties
, other authors have reported just the opposite
.Chen
concluded in a case series that short term OK(STOK) treatment induced a reduction of corneal hysteresis(CH) parameters measured with the Ocular Response Analyzer(ORA) from Reichert. In contrast, Lam
concluded in another randomized study that STOK had no significant effect on corneal tangent modulus, with changes in CH and corneal resistance factor (CRF) measured with the ORA device being related to their intrinsic measurement variability.
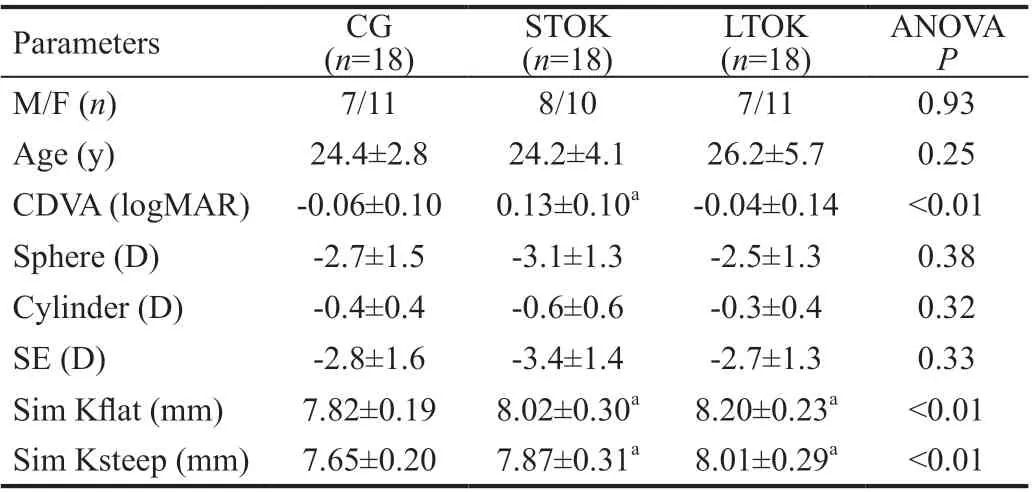
A total of 54 eyes of 54 patients with ages ranging from 18 to 35y (mean age: 24.9±4.4y) were evaluated in the current study.The sample included a total of 22 men (40%) and 32 women(60%). Mean spherical equivalent in the whole sample was-3.00±1.40 D. As previously mentioned, three groups of eyes were differentiated: CG (18 eyes), STOK group (18 eyes), and LTOK group (18 eyes). Table 1 summarizes the main clinical data characterizing these three groups.
SUBJECTS AND METHODS
Demographic, Visual, Refractive, and Corneal Curvature Data No significant differences were found between groups in age (
=0.25) or gender (
=0.93; Table 1). In contrast,significantly poorer CDVA was found in STOK compared to CG and LTOK (
<0.01). Likewise, significantly flatter keratometric readings were obtained in STOK and LTOK groups compared to CG (
<0.01; Table 1).
随着人工智能、大数据技术的发展,作为新资源、新技术和新理念的混合体,大数据不仅在企业的管理过程中,而且在国家、社会治理中其评价、预测、决策功能也发挥着越来越大的价值。这一新技术的应用,也给法学研究带来了新的挑战。其中,如何明确大数据权利属性,如何保护个人信息,如何明确数据法律关系中各主体的行为边界,成为一个非常现实的命题,具有很强的学理与现实意义。
Subjects
This retrospective, observational and comparative study enrolled a total of 54 subjects that were divided into three groups: control group (CG), including 18 non-contact lens wearers; STOK group, including 18 subjects treated with OK with a short time follow-up; and long term OK (LTOK)group, including 18 subjects treated with OK for a long-time follow-up.
Tomographic biomechanical index (TBI): calculated by combining tomographic and biomechanical parameters and using an artificial intelligence approach to optimize ectasia detection
.
Inclusion criteria for all groups were Caucasian men or women with an age between 18 and 35 years old, myopia between 0.75 and 6.00 D, and astigmatism below 2 D. Exclusion criteria included previous ocular surgery, strabismus, keratoconus or any other ectatic corneal disease, active ocular or systemic pathology, and pregnancy. In CG, only healthy non-contact lens wearers with any active ocular or systemic disease were included. In STOK and LTOK groups, patients were treated with OK for two weeks and for more than 1y, respectively.
Clinical Protocol A complete examination was performed in all patients including the following tests and measurements:manifest refraction, measurement of corrected distance visual acuity (CDVA) using an ETDRS chart at 4 metres,measurement of axial length (AXL) and anterior chamber depth (ACD) with an optical biometer (IOL Master 700,Carl Zeiss Meditec, Jena, Germany), corneal topographic analysis (Pentacam HR, Oculus Optikgerate Optikgerate GmbH, Wetzlar, Germany, software version 1.25r15), and measurement of the corneal biomechanical properties with the CorVis
ST system (Oculus Optikgerate GmbH, Wetzlar,Germany, software version 1.6r2223). Three consecutive measurements were performed on each eye by 2 experienced examiners and only those with image quality graded as “OK”were collected. The CorVis
ST is a non-contact tonometer that allows the clinician to analyze the response of the cornea to an air pulse. A high-speed Scheimpflug camera records corneal movements, corneal flattening length, and velocity over time
. This camera captures more than 4300 frames per second, providing reliable measurements of intraocular pressure (IOP) and corneal thickness
. Concerning the biomechanical parameters provided by this system, the following were considered in the current analysis:
First applanation time (AT1): time in which the first applanation is reached.
Amplitude of deformation 1 (AD1): amplitude of deformation at the first applanation time.
式中:Q*,GH,ΔM分别为双堆垛机执行出库任务运行时间的数学期望、货架重心高度、成组货架质量差的绝对值,已于式(10)中详细描述;分别为当代栖息地中,对应各目标函数的最大值。以此为HSI,可以保证:①HSIQ*最大的货位分配方案双堆垛机执行出库任务运行时间的数学期望最小;②HSIGH最大的货位分配方案货架重心高度最低;③HSIΔM最大的货位分配方案成组货架质量差的绝对值最小。
OK does not seem to alter significantly the corneal biomechanical properties, but special care should be taken when analyzing biomechanical parameters influenced by corneal thickness such as amplitude of deformation, ARTh or CBI, because they change significantly after treatment but mainly due to the reduction and pachymetric progression induced by the corneal molding secondary to OK treatment.
Second applanation time (AT2): time in which the second applanation is reached.
Maximum deflection amplitude (MaxDA): the maximum amount of the corneal movement compensating for the whole eye movement during the measurement.
Velocity of corneal apex at the first applanation time (AV1).
Velocity of corneal apex at the second applanation time (AV2).Corneal stiffness parameter (SPA1): resulting pressure on the cornea divided by the deflection amplitude at the first applanation
.
文献[19]显示,当模型的水平范围为8~10倍隧道直径时,即可获得较高的计算精度。本文建立了二维弹塑性动力有限元模型,模型水平方向为80 m,竖直方向为60 m,盾构隧道直径为6 m。
Strain stress index (SSI): this index represents the stress-strain curve and describes the elastic properties of the cornea. The curve is shifted to the right if the cornea is soft, and to the left if the cornea is stiff.
“二表哥吐了一口唾沫,然后把手中的耙子扔在地上,娟儿尖叫了一声。我吓傻了,想跑,但二表哥发现了我,我吓得汗毛都竖了起来。二表哥跑过来,把我拉进柴垛后,我以为他想把我也杀死,但他只是让我脱衣服,我害怕得要死,只好听他的话。
在最新的DNV GL有关浮式风机的规范中指出[10],锚链断裂等故障工况,应该在设计工况中考虑。目前,国内外对浮式风机锚链断裂、舱室破损等特殊故障工况还很少有研究。本文以IEA Wind Task30提出的浮式风机研究模型OC4 DeepCwind半潜式浮式风机为研究对象,采用ANSYS-AQWA计算该浮式风机在故障工况下的运动响应和荷载分析。该型浮式风机适用于我国南海海域,对解决沿海海域和岛礁海域用电问题有积极的意义,为我国建设成为海洋强国的战略目标提供一定的技术支持。
ARTh: standard deviation of Ambrosio’s relational average thickness related to the horizontal profile (temporal-nasal direction).
CorVis
biomechanical index (CBI): combines several parameters to indicate the likelihood of subclinical keratoconus and corneal ectasia
. Specifically, it considers the following data: deformation amplitude ratio at 1 and 2 mm, applanation 1 velocity, standard deviation of deformation amplitude at highest concavity, Ambrósio’s relational thickness to the horizontal profile, and corneal stiffness parameter
.
末次随访时,按照Johner-Wruhs评定标准评定临床疗效见表5。优良率UTN组85.19%,LCP组81.82%,UEF组67.74%。一期采用锁定钢板内固定治疗典型病例见图1。
Biomechanically corrected IOP (bIOP): corrected considering the corneal thickness and stiffness.
Orthokeratology Treatment Eyes in the STOK group were fitted with the Beefree contact lenses (Medmont Internacional Pty Ltd., Nunawading, Australia). This lens has a double reverse geometry design and is made of Boston XO2 material.According to the topographic measurements obtained in the baseline examination, the four curves of variable diameter of the contact lens are defined to obtain the best possible fit. All the eyes on STOK group wore OK lenses for 15 nights.
Eyes in the LTOK group were fitted with the Paragon CRT contact lenses (Paragon Vision Science, Gilbert, USA;distributed in Spain by Interlenco SA). This lens has a reverse geometry design with 3 clearly differentiated zones: optical zone (4 mm), return zone (3 to 3.5 mm), and a landing zone band (3 to 3.5 mm). This lens is made of HDS 100 material(Paragon Vision Science, Gilbert, USA). In the fittings performed in the current study, the diameter of 10.50 mm was always used. In this LTOK group, the mean contact lens wear period was 4.6±3.2y. Specifically, 56% and 44% eyes of LTOK wore OK contact lenses between 1 to 2y and more of 7y, respectively.
Statistical Analysis Before initiating the study, the sample size required for obtaining an acceptable statistical power was calculated using the Granmo 7.12 online calculator (https://www.imim.es/ofertadeserveis/software-public/granmo/).Specifically, according to a previous study by Ambrósio
that analysed the variability of the SPA1 in normal and abnormal corneas, a sample size of 17 per group was found to be necessary assuming an alpha risk of 0.05 and a beta risk of 0.02.
如果要理解这些肿瘤的性别差异的关键在于找出性别差异的原因,而且这将有助于优化性别相关的治疗,揭示可能的保护性或者有害的性别因子,并提出新的治疗策略。尽管一些肿瘤的性别差异源于高度性别化的环境(职业、吸毒等),这使得男性和女性暴露于不同的疾病风险,但还可以寻找在细胞内关键的性别差异,从而降低肿瘤生长的可能性。性激素是主导性别差异的原因,但在这篇文章中,作者更关注细胞内基因组中的性别差异。
Data analysis was performed using Statgraphic Centurion 8 software (StatGraphics.net, Madrid, Spain). The normality of the variables was verified by the Kolmogorov-Smirnov test,using non-parametric statistics in those variables showing nonnormal distributions. Only one eye per patient was randomly selected to avoid the potential bias associated to the correlation between interocular data of each patient. Regarding the comparison between groups of the numerical variables of the study, a one-way analysis of variance (ANOVA) was used if data were normally distributed, using the Bonferroni test for post-hoc comparisons between pairs of groups. When variables were not normally distributed, the Kruskal-Wallis test was used to assess the statistical significance of differences between groups, using the Mann-Whitney
test with the Bonferroni correction for post-hoc comparisons between pairs of groups.The correlation between different variables evaluated in the study was investigated by calculating the Pearson or Spearman correlation coefficient depending on if the normality of the data distributions could be assumed or not, respectively. The level of statistical significance was set at
-value below 0.05.
RESULTS
One of the main reasons for these limited analyses on corneal biomechanical changes after OK is the limited number of technologies clinically available to measure or estimate the biomechanical properties of the cornea, mostly based on the analysis of the corneal response to an air puff
. Furthermore,some factors may have been related to this variability among studies evaluating the corneal biomechanical changes after OK, including the moderate consistency of measurements obtained with air puff-based devices to characterize the corneal biomechanics
and the limited knowledge of the real meaning of those parameters provided by these devices to assess the mechanical properties of the cornea
. The aim of the current study was to investigate the short and long term corneal biomechanical changes after OK and compare them with those occurring in subjects not wearing contact lenses.

Ethical Approval This study was approved by the Clinical Research Ethics Committee of Hospital San Carlos (Madrid)and was conducted following the tenets of the Declaration of Helsinki. All participants were informed about the study and accepted to participate, providing written informed consent.
Pachymetric, IOP, and Corneal Biomechanical Data No significant differences between groups were found in central corneal thickness (CCT), IOP and bIOP values (
>0.05;Table 2). Concerning the biomechanical parameters,significantly lower values of AD1 and ARTh were found in the OK groups compared to CG (
<0.05). Likewise, significantly higher values of CBI were found in STOK and LTOK groups compared to CG (
<0.01; Figure 1, Table 2).
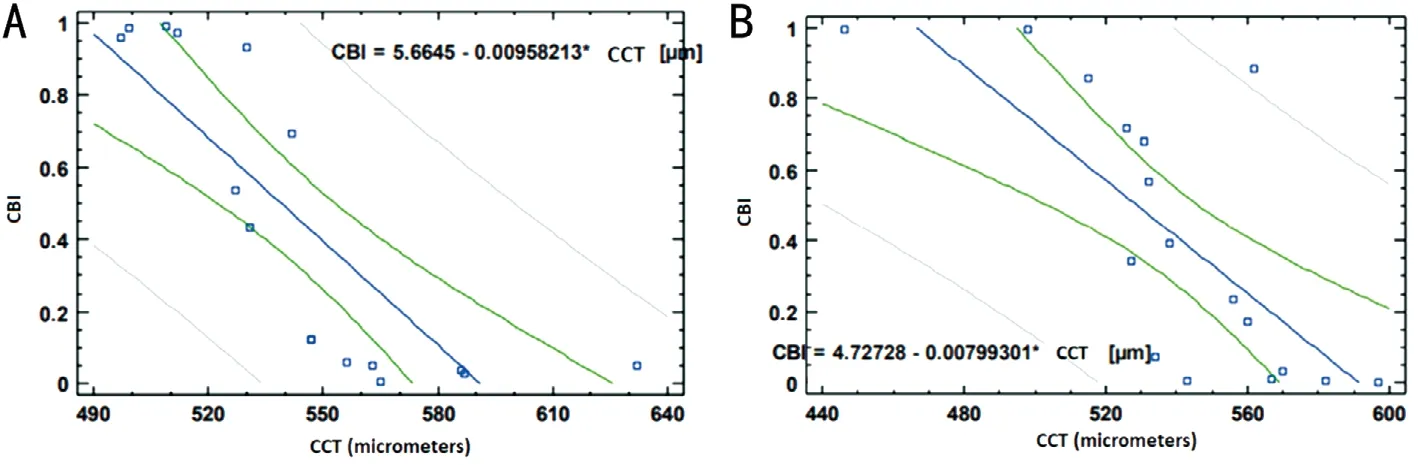

Correlation of Corneal Biomechanical Data with Other Clinical Data A moderate and statistically significant positive correlation was found between CCT and ARTh in STOK(
=0.67,
<0.01) and LTOK groups (
=0.62,
<0.01). Stronger but inverse correlations were found between CCT and CBI in STOK (
=-0.90,
<0.01) and LTOK groups (
=-0.71,
<0.01; Figure 2). Furthermore, a moderate inverse correlation was found between CCT and TBI in STOK group (
=-0.57,
=0.02).
DISCUSSION
In this study, the corneal biomechanical properties were evaluated using the CorVis
ST system in OK users in a population aged between 18 and 35y and compared with the measurements obtained in a CG including non-contact lens wearers. The main research findings show that the biomechanically AD1 and ARTh, was lower in STOK and LTOK users compared to non-contact lens users. Furthermore,PachySlope and CBI showed higher values in STOK and LTOK versus CG. Likewise, there were other biomechanical parameters showing trends of change without reaching a statistically significant difference, such as IOP, bIOP, and IR. Our findings about corrected IOP are in agreement with previous studies
which measured with the ORA system the value of bIOP after OK. The trend of bIOP to decrease may be related to the fact that the OK treatment generates a short and long term decrease in corneal epithelium thickness
. It should be considered that non-contact tonometry is influenced by confounding variables such as corneal thickness
. Indeed,significant reductions of bIOP have been reported after the reduction of corneal thickness occurring with different techniques of corneal refractive surgery, such as laser
keratomileusis (LASIK) and small incision lenticule extraction(SMILE)
. Despite this, the bIOP from the CorVis
ST device after laser corneal refractive surgery has been found to be in closest agreement with those obtained before surgery compared to other measurements of IOP
.
As shown in Table 2, the same mean value of CCT (547 μm)was found in CG and STOK groups despite some level of thinning was expected in the STOK group considering the mechanism of action of OK. Several factors may account for this apparent contradictory outcome, such as the presence of some level of corneal edema in the OK patients when the measurements were taken in the morning, or the inclusion of thicker corneas in the STOK group with a higher pre-fitting CCT. This could be easily confirmed by analyzing the prefitting data, but this information was not available, which can be considered as a limitation of the current study. On the other hand, the reduction in corneal thickness and the change in the pachymetric progression (Pachyslope) in OK users was also a crucial factor explaining the significantly lower ARTh values in STOK and LTOK groups compared to CG.It should be considered that this CorVis
ST parameter has been found to be strongly and significantly correlated with CCT
. Therefore, the pachymetric reduction associated to the orthokeratologic effect is the main factor explaining the significantly lower values of ARTh in STOK and LTOK groups. Indeed, statistically significant correlations among CCT and ARTh were found in the current series in the two OK groups evaluated.
实际上,司马迁不仅不“先黄老而后六经”,在许多事情上,尤其是对历史人物和历史事件的评价上,“至圣”孔子的价值标准还成为司马迁的重要参考,许多时候司马迁甚至直接采用孔子的价值标准来对历史人物和历史事件进行评价。如:
As previously mentioned, significantly lower values of AT1 were found in the OK groups compared to CG. However,it cannot be concluded that the mechanical properties of the cornea are altered after OK according to the change in these parameters since the corneal deformation generated by the air puff is the result of the interaction between the mechanical properties, IOP, and geometry
. Indeed, different combinations of corneal mechanical properties within the human range and IOP could produce the same apical displacement in response to an air-puff
. Furthermore, the values found in the current study of SSI found that corneal elasticity was not significantly different between OK wearers and non-contact lens users. In general, as the CCT decreases below 500 μm, the maximal corneal displacement measured with the CorVis
ST increases rapidly, being three times larger for CCT below 400 μm
. For this reason, significant decreases of AT1 have been reported after laser corneal refractive surgery, especially in those cases in which a more significant reduction of corneal thickness was needed
.Fernández
reported that SMILE surgery induced significant changes in the CorVis
ST parameters of time and deformation amplitude, but these changes were mainly explained by the confounding variable of corneal thickness.Similarly, several previous studies have shown that there is a reduction of CH and CRF measured with the ORA (also based on the delivery of an air puff) with OK
. Indeed,these parameters have been also shown to be correlated with CCT
.
Besides AD1, AT1 and bIOP, significant differences were found between groups in CBI, with values significantly higher in OK groups. This index allows differentiating healthy from ectatic corneas
. The CBI values obtained in the current sample in the OK groups are increased compared to CG, but within the range of normality
. Kataria
define a cutoff value of the CBI for the detection of keratoconus of 0.78 and 0.97 for mild keratoconus. The increase found in CBI in OK groups may be explained by the pachymetric reduction induced with the treatment as a significant and strong correlation was found between CCT and CBI in only STOK and LTOK groups. It can seem contradictory the difference found in the current study in terms of CBI between CG and STOK despite the similarity of CCT. However, this may be due to the differences in the change in the corneal thickness progression from the center to the corneal periphery or even in some pre-fitting differences of the corneal mechanical properties between the corneas of both groups. It should be considered that CBI is not only dependent on CCT. The use of TBI instead of CBI has been shown to be more accurate for the diagnosis of corneal ectasia, being less influenced by pachymetric changes
. This optimized index did not differ significantly between groups as well as the corneal stiffness parameters (AP-1), suggesting that no significant corneal biomechanical changes are present in the short and long term after OK. This is consistent with the results of previous authors reporting no significant changes in corneal stiffness and tangent modulus after OK
. Specifically, Lam
demonstrated using the ORA device that STOK had no significant effect on corneal tangent modulus estimated from the measurements obtained with this device.
This study has some limitations that should be acknowledged.First, this study has the inherent limitations to any retrospective study, but it can be considered as an additional step forward a complete understanding of corneal biomechanical changes occurring with OK, being the first study showing short and long term CorVis
ST biomechanical data associated to this option of refractive correction. Another limitation can be considered the use of different data samples for reporting short and long term biomechanical corneal data after OK,with the use of different types of reverse geometry contact lenses in STOK and LTOK groups. However, as both contact lens designs have an optical zone of 6 mm, the central corneal molding did not seem to differ significantly, with similar levels of central flattening. It should be considered that a similar range of dioptric correction was treated in both OK groups.For this reason, this factor does not seem to be a relevant or critical factor for biasing the outcomes and the conclusions of the study. Finally, the post-fitting evolution of corneal biomechanical parameters was not available in most of patients and consequently we were not able to analyze in STOK and LTOK longitudinal changes occurring in these parameters.Future studies should be conducted to analyze corneal biomechanical changes after OK in the long-term.
In conclusion, overnight OK does not seem to alter significantly the corneal biomechanical properties in the short and long-term wearing. However, care should be taken when analyzing biomechanical parameters influenced by corneal thickness, such as amplitude of deformation or CBI, because they are going to change significantly after OK but mainly due to the pachymetric reduction induced with the treatment. More studies are needed to understand better the impact of OK on the mechanical properties of the cornea using other measuring technologies not based on the analysis of the corneal response to an air pulse.
ACKNOWLEDGEMENTS
Foundation: Supported by the Ministry of Economy, Industry and Competitiveness of Spain within the program Ramón y Cajal, RYC-2016-20471.
Conflicts of Interest: Nieto-Bona A, None; Porras-Ángel P, None; Ayllón-Gordillo AE, None; Carracedo G, None;Piñero DP, None.
1 Bullimore MA, Johnson LA. Overnight orthokeratology.
2020;43(4):322-332.
2 Singh K, Bhattacharyya M, Goel A, Arora R, Gotmare N, Aggarwal H. Orthokeratology in moderate myopia: a study of predictability and safety.
2020;15(2):210-217.
3 Sánchez-García A, Ariza MA, Büchler P, Molina-Martin A, Piñero DP.Structural changes associated to orthokeratology: a systematic review.
2021;44(4):101371.
4 Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology.
2020;103(1):44-54.
5 González-Mesa A, Villa-Collar C, Lorente-Velázquez A, Nieto-Bona A.Anterior segment changes produced in response to long-term overnight orthokeratology.
2013;38(8):862-870.
6 Lam AKC, Hon Y, Leung SYY, Shu-Ho L, Chong J, Lam DCC.Association between long-term orthokeratology responses and corneal biomechanics.
2019;9(1):12566.
7 Lam AK, Leung SY, Hon Y, Shu-Ho L, Wong KY, Tiu PK, Lam DC.Influence of short-term orthokeratology to corneal tangent modulus: a randomized study.
2018;43(4):474-481.
8 Chen RN, Mao XJ, Jiang J, Shen MX, Lian Y, Zhang B, Lu F. The relationship between corneal biomechanics and anterior segment parameters in the early stage of orthokeratology: a pilot study.
2017;96(19):e6907.
9 Yeh TN, Green HM, Zhou YX, Pitts J, Kitamata-Wong B, Lee S,Wang SL, Lin MC. Short-term effects of overnight orthokeratology on corneal epithelial permeability and biomechanical properties.
2013;54(6):3902-3911.
10 Chen D, Lam AKC, Cho P. A pilot study on the corneal biomechanical changes in short-term orthokeratology.
2009;29(4):464-471.
11 González-Méijome JM, Villa-Collar C, Queirós A, Jorge J, Parafita MA. Pilot study on the influence of corneal biomechanical properties over the short term in response to corneal refractive therapy for myopia.
2008;27(4):421-426.
12 Piñero DP, Alcón N. Corneal biomechanics: a review.
2015;98(2):107-116.
13 Wan K, Cheung SW, Wolffsohn JS, Cho P. Repeatability of corneal biomechanics waveform signal parameters derived from Ocular Response Analyzer in children.
2021;44(5):101373.
14 Mercer RN, Waring GO 4th, Roberts CJ, Jhanji V, Wang YM, Filho JS, Hemings RA Jr, Rocha KM. Comparison of corneal deformation parameters in keratoconic and normal eyes using a non-contact tonometer with a dynamic ultra-high-speed scheimpflug camera.
2017;33(9):625-631.
15 Vinciguerra R, Ambrósio R Jr, Elsheikh A, Roberts CJ, Lopes B,Morenghi E, Azzolini C, Vinciguerra P. Detection of keratoconus with a new biomechanical index.
2016;32(12):803-810.
16 Chan TCY, Wang YM, Yu M, Jhanji V. Comparison of corneal tomography and a new combined tomographic biomechanical index in subclinical keratoconus.
2018;34(9):616-621.
17 Ambrósio R Jr, Lopes BT, Faria-Correia F, Salomão MQ, Bühren J,Roberts CJ, Elsheikh A, Vinciguerra R, Vinciguerra P. Integration of scheimpflug-based corneal tomography and biomechanical assessments for enhancing ectasia detection.
2017;33(7):434-443.
18 Nieto-Bona A, González-Mesa A, Villa-Collar C, Lorente-Velázquez A. Biomechanical properties in corneal refractive therapy during adaptation period and after treatment interruption: a pilot study.
2012;5(4):164-170.
19 Ariza-Gracia MÁ, Zurita JF, Piñero DP, Rodriguez-Matas JF, Calvo B. Coupled biomechanical response of the cornea assessed by non-contact tonometry. A simulation study.
2015;10(3):e0121486.
20 Abd El-Fattah EA, El Dorghamy AA, Ghoneim AM, Saad HA.Comparison of corneal biomechanical changes after LASIK and F-SMILE with CorVis ST.
2021;31(4):1762-1770.
21 Bao FJ, Huang W, Zhu R, Lu NJ, Wang Y, Li HC, Wu SA, Lin HN,Wang JJ, Zheng XB, Huang JH, Li YY, Wang QM, Elsheikh A.Effectiveness of the goldmann applanation tonometer, the dynamic contour tonometer, the ocular response analyzer and the corvis ST in measuring intraocular pressure following FS-LASIK.
2020;45(2):144-152.
22 Liu MN, Shi WY, Liu X, Li N, Chen T, Gao H. Postoperative corneal biomechanics and influencing factors during femtosecondassisted laser
keratomileusis (FS-LASIK) and laser-assisted subepithelial keratomileusis (LASEK) for high myopia.
2021;36(8):1709-1717.
23 Fernández J, Rodríguez-Vallejo M, Martínez J, Tauste A, Piñero DP.Corneal thickness after SMILE affects scheimpflug-based dynamic tonometry.
2016;32(12):821-828.
24 Kataria P, Padmanabhan P, Gopalakrishnan A, Padmanaban V,Mahadik S, Ambrósio R Jr. Accuracy of Scheimpflug-derived corneal biomechanical and tomographic indices for detecting subclinical and mild keratectasia in a South Asian population.
2019;45(3):328-336.
 International Journal of Ophthalmology2022年7期
International Journal of Ophthalmology2022年7期
- International Journal of Ophthalmology的其它文章
- Impact of OCT scan-patterns in identifying morphological features of lamellar macular holes and macular pseudoholes
- Virtual reality training improves accommodative facility and accommodative range
- Short-term effect of 0.01% atropine sulphate eye gel on myopia progression in children
- Reduced choroidal peripapillary capillaries in thyroidassociated ophthalmopathy with early stage of dysthyroid optic neuropathy
- Incidence of ocular manifestations in patients with graft versus host disease after allogeneic stem cell transplant in Riyadh, Saudi Arabia
- Clinical features, surgical outcomes and genetic analysis of ectodermal dysplasia with ocular diseases
