Molecules related to diabetic retinopathy in the vitreous and involved pathways
INTRODUCTION
Diabetes mellitus (DM) is a metabolic disorder characterized by chronic hyperglycemia and the damage to vessels. Metabolic disorders in carbohydrates, fats and proteins could cause multi-organ damage, which led to organ dysfunctions, further resulting in diabetic complications.According to the 2019 International Diabetes Federation (IDF)Global Diabetes Map (Ninth Edition), there are currently approximately 463 million people with diabetes worldwide,and the prevalence among adults (aged 20-79y) is 9.3%.Among them, China has the largest population of patients with about 116.4 million, accounting for a quarter of the total number of patients in the world. Among them, 35.5 million people are over 65 years old.
Diabetic retinopathy (DR) is one of the most common complications of diabetes, as well as the most common retinal vascular disease. It was reported that DR was the main blindness-causing diseases in people over 50 years old
. The basic pathological changes of DR are retinal microangiopathy,including fundus neovascularization and fibrous proliferation.Current studies on DR have shown that the core molecule involved in the pathophysiology is vascular endothelial growth factor (VEGF), which can specifically stimulate the proliferation of vascular endothelial cells and promote neovascularization
. A great number of studies have confirmed that concentrations of VEGF in the vitreous of DR patients is significantly higher than that of ordinary people
, and drugs targeting VEGF have already been developed, one of which were anti-VEGF drugs and it has been widely accepted as a mainstream treatment method yet. However, recent studies discovered that there are many deficiencies in the application of anti-VEGF drugs, such as long-term drug resistance, high cost of treatment, and potential retinal detachment risk caused by intraocular injection
. In recent years, molecular research on the pathogenesis of DR has become a hot spot. Existing studies have found that although VEGF is the key molecule in the development of DR, there are hundreds of other molecules in the vitreous that participate in the process. Some of them are VEGF-dependent and others work independently
. Here, we present an overview focusing on the pathways and molecules discovered in the vitreous which are found to involve in the development of DR. We hope this review could reveal the intrinsic relationships between these molecules and provide inspirations for research interests and new therapeutic targets.
农业保险工作,是一项新生事物,既要提高农民自身投保的积极性,又离不开政府的支持和引导。在下步工作中,重点抓好以下方面工作:
VITREOUS AND ITS ROLE IN DIABETIC RETINOPATHY Vitreous and Its Relationship with Diabetic Retinopathy Vitreous is the major content of the eye accounting for 80%of the inner volume of the whole globe which could transmit light to the retina and maintain the shape of the ocular tissue.Nowadays, lots of studies find that vitreous contains a variety of molecules that is associated with the function of other parts of the eye. These molecules can provide nutrition, perform anti-oxidant effect and may play a role in the development of some eye diseases
. For the vitreous body is in direct contact with the retina, the factors involved in the development of DR can diffuse into the vitreous, making it possible to study DR by exploring the relevant factors in the vitreous body
.As is widely accepted that VEGF is the core molecule in the development of DR, knowing how VEGF in the vitreous performs its biological function can greatly elaborate the mechanism of DR progression.
Role of Vascular Endothelial Growth Factor in Diabetic Retinopathy DR is clinically divided into non-proliferative DR (NPDR) and proliferative DR (PDR) according to the emergence of neovascularization, in which VEGF is highly involved. In NPDR stages, hyperglycemia causes damage to small blood vessels in the retina, thus leading to the secretion of VEGF, which acts as a protective role on rescuing the retinal neurons, but it also affects blood vessels negatively
.If the damage factors persist for a longer time, high-level of VEGF breaks the balance between pro-angiogenic and antiangiogenic factors, after which VEGF acts destructively on vascular endothelial cells and stimulates the formation of new blood vessels, which is the symbol of PDR stage
. Meanwhile,VEGF in the vitreous can induce new blood vessels to grow into the vitreous cavity, leading to serious complications such as vitreous hemorrhage and tractional retinal detachment.
综上优缺点所述,根据现场焊缝的实际情况,适宜选择这两种方法或者两者结合进行检测,以符合标准要求和质量要求。
After that extracellular VEGF binds to VEGFR and activates the receptors through transphosphorylation, thereby activating downstream pathways. In this section, we mainly discussed three downstream pathways: phosphatidylinositol diphosphate(PIP2), phosphoinositide-3-kinase (PI3K), and mitogenactivated protein kinase (MAPK) pathway. The detailed pathway and key molecules are presented in Figure 1.
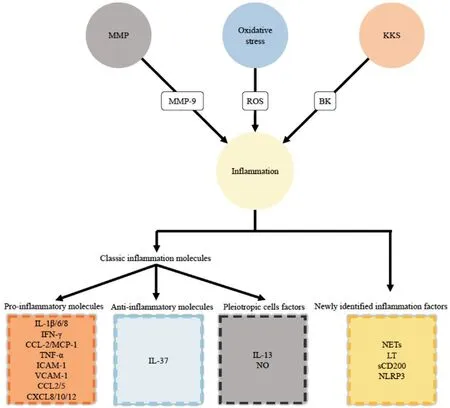
Previous studies have measured various inflammatory molecules in the vitreous specimens and evaluated their role in the development of DR. We divided these inflammatory molecules into three groups: pro-inflammatory molecules,anti-inflammatory molecules and pleiotropic cells factors.Pro-inflammatory molecules referred to factors which can promote inflammation, including interleukin (IL)-1β, IL-6,IL-8, Interferon-γ (IFN-γ), CCL-2/MCP-1, tumor necrosis factor α (TNF-α), intercellular cell adhesion molecule-1(ICAM-1), vascular cell adhesion molecule-1 (VCAM-1),chemokines CCL2, CCL5, CXCL8, CXCL10, CXCL12
,CXCL16, ADAM10 and ADAM17
. Among them, studies have found that the levels of all above factors except IL-6 in the vitreous of patients with DR are higher than those in the control group, but there is no significant difference between IL-6
. However, other studies draw different conclusions.One study has shown that in patients with PDR after partial vitrectomy, the levels of MCP-1/CCL-2 and IL-6 in the vitreous increase. It is speculated that the increase of these two substances in the postoperative period is indicative of longterm inflammation, thus having a certain predictive value on postoperative DME
. Anti-inflammatory molecules referred to factors which can inhibit inflammation, including IL-37.A study pointed out that IL-37 is also elevated in the vitreous of PDR patients, and its content is related to VEGF-A and Ang-2, suggesting that it plays a role in PDR
. Although anti-inflammatory immune regulators like IL-37 are found to be up-regulated, they are more of a passive compensation and are not strong enough to reverse the inflammatory process
.Pleiotropic cells factors referred to factors which can both promote and inhibit inflammation under different conditions,include IL-2, IL-4, IL-13 and NO. Among them, studies have found that IL-13 is down-regulated, NO is up-regulated in the vitreous of PDR patients, and there is no significant difference as for IL-2 and IL-4
.
IRS-2蛋白阳性表达位置主要在细胞质中出现棕黄色颗粒,每例随机观察5个高倍镜(400倍)视野,根据阳性细胞数和着色深度计分,阳性表达<5%为0分,5%~24%为1分,25%~49%为2分,50%~74%为3分,≥75%为4分。阳性细胞表达的着色深度:基本不着色为0分,淡黄色为1分,黄色为2分,棕黄色3分。两者得分相乘,<3分判定为表达阴性,其余判定为表达阳性。所有切片均采用双盲法由2位病理科主任医师阅片,2人结果一致则记录结果,如有争议请第3位病理科医生看片,以2个相同结果为准。
改革开放前,由于当时受技术等因素所限,我国农药工业发展较为缓慢,农药产品供应数量少、生产规模小,适应不了农业发展的需要。上世纪80年代,改革开放促进农业发展与农药市场扩容加快,作为支农行业的农药,国家鼓励和政策支持其引进国外先进技术装备,吸引国外优秀人才来加快企业发展,同时,农业丰收带来的巨大市场需求也推动一部分农药企业走出去、请进来,促使我国农药产量的扶摇而上。
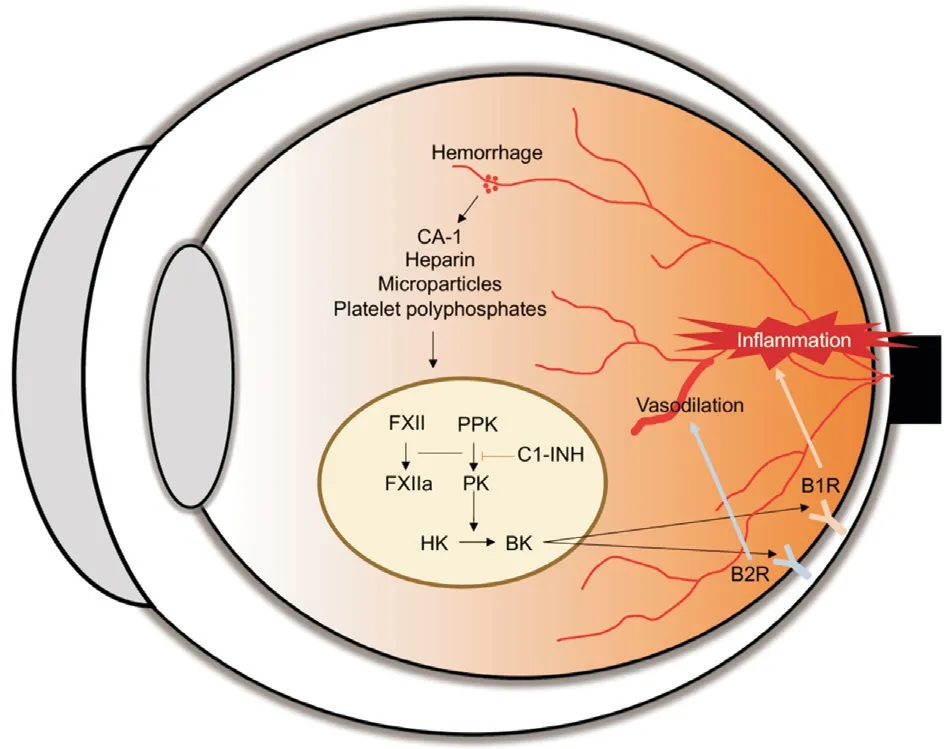
Molecules From Kallikrein-Kinin System KKS is a set of regulatory systems including kallikrein and kinin in the human body. Kallikrein is a collective name for polypeptides including a variety of bradykinins (BK). KKS is composed of two independently regulated proteolytic pathways mediated by tissue kallikrein (TK) and plasma kallikrein (PK) in human,both of which are expressed in eye and found to be related to the progression of DR
the production of bradykinin and spontaneous stimulation of bradykinin receptors
.After the activation of BK receptors, KKS performs a variety of physiological effects such as coagulation, fibrinolysis,angiogenesis,
.
女孩毕业后,这条连接两所大学的窄街拆迁了,煎饼摊被挪到了更偏的地方,很难找。但根深蒂固的记忆帮了女孩,她一路寻一路问:要找那家鏊子有80厘米的煎饼摊,门口,摊煎饼的人放着好几盆茉莉花和珠珠花。对了,就是那个既摊棕色煎饼又摊米黄煎饼的老徐煎饼档。
Up to now, there have been a few studies on the role of KKS in the vitreous of DR patients. In normal eyes, with the function of blood-retinal barrier, some circulating substances can’t diffuse into vitreous. However, under DR conditions,substances diffuse becomes easier since the breakdown of the barrier. A group of molecules in plasma KKS family,including high molecular weight kininogen, prekallikrein(PK), coagulation factor XII (FXII) and complement 1 esterase inhibitor (C1-INH) have been identified to accumulate in the vitreous of DR patients by proteomic analysis
. First three molecules participate in the activation of KKS, while C1-INH can inhibit KKS by preventing PK from activation. In retinal tissues, the activation of KKS promotes the aggregation of neutrophils and microglia
, and at the same time may increase vascular permeability and vascular edema, change the diameter of the vascular and the hemodynamics, and affect inflammation, angiogenesis, and neuronal functions
. The detailed mechanism of KKS system was shown in Figure 3.


大型科学研究仪器设备对前沿科学研究起着重要的保障作用,是进行高精尖科学研究的物质基础,一个国家大型科学仪器设备的数量从一定程度上可以反映该国在科学领域的研究地位。国内高校、科研院所、企事业单位以及军工单位对大型科学仪器设备的购置数量不断增加、品质不断提高。
In this section, we will introduce newly explored molecules in the vitreous which may have relationship with the development of DR, as well as pathways they involved: Kallikrein-Kinin System (KKS), oxidative stress, inflammation and matrix metalloproteinase (MMP). Also some other molecules apart from these four pathways will be briefly introduced in this section (Figure 2).
Currently, no human experiments confirmed that KKS was related to retinal neovascularization, but KKS has been proven to promote angiogenesis in other tissues
. Therefore, the role of KKS in retinal neovascularization needs to be further explored.
When hyperglycemia damages the microvascular in the eye tissue, hypoxia occurs. Meanwhile, the level of intracellular hypoxia-inducible factor 1 (HIF-1), basic fibroblast growth factor (bFGF), platelet derived growth factor (PDGF) and oxygen regulated protein 150 (ORP150) increases
. HIF-1 is a DNA-binding protein that binds to the VEGF gene region and initiates transcription of the VEGF gene, thereby causing a large amount of VEGF to be produced. After that, ORP150 begins to play a role as molecular chaperone which binds to VEGF in the endoplasmic reticulum and transports it to the Golgi apparatus, promoting the release of VEGF to the extracellular matrix.
Molecules Related to Oxidative Stress Diabetes induced oxidative stress in retinal and capillary cells plays a significant role in the development of DR
. Oxidative stress represents the imbalance between oxidants and antioxidants, resulting in generating a huge amount of reactive oxygen species (ROS)
.Excessive ROS can inhibit mitochondrial biogenesis and mitochondrial DNA (mtDNA) repair, lower the levels of antioxidants such as Mn-superoxide dismutase (Mn-SOD)and glutathione (GSH), methylate mtDNA to alter the protein expression, which results in mitochondrial dysfunction and changes the permeability of the outer membrane, thus increasing the release of cytochrome C and further inducing cell apoptosis
. Besides, ROS can promote the production of inflammatory factors such as nuclear factor kappa-B(NF-κB), protein kinase C (PKC), MAPK
, intensifying the inflammatory response
(Figure 4). Recently, oxidative stress related molecules have been focused by many researchers.Some oxidative stress-related biomarkers have been found to have altered concentrations in DR patients, which may help patients get earlier and more precise diagnosis. In plasma and vitreous of patients with PDR, the content of superoxide dismutase (SOD) and lipid hydroperoxidation (LPO) were significantly higher than those in the control group, and there was a positive correlation between the two molecules, while other oxidative stress-related biomarkers such as advanced oxidized protein product (AOPP) and malondialdehyde(MDA) showed no differences between groups. Researchers suggested that the combined increase of SOD and LPO can be a biomarker of the progression of DR
. Animal studies and human studies of DR asymptomatic patients are needed to further confirm the availability.
In addition, some proteomics studies have shown that about 30 kinds of protein related to KKS increased and had significant correlation with diabetic macular edema (DME), and the correlation coefficient was greater than that between VEGF and DME. It is suggested that KKS may be more related to the occurrence of DME than DR
. Besides, KKS and VEGF are thought to act independently in the development of DME, for the levels of PK and VEGF in the vitreous samples of DME patients were not correlated
.
Besides, a newly discovered protein, oxidative stress-responsive apoptosis-inducing protein (ORAIP), was found to play a role in DR progression
. Under the oxidative stress, ORAIP is rapidly secreted from cells and acts as a pro-apoptotic ligand to induce apoptosis. Some studies have found that the ORAIP in the vitreous of patients with PDR is significantly higher than that in the control group. It was speculated that ORAIP may cause retinal damage through oxidative stress, but the specific mechanism needs to be further explored
.

As for the relationship between oxidative stress and VEGF,oxidative stress can change the expression of VEGF
alter the levels of microRNAs (miR) such as miR-126, miR-146a and miR-200b. Oxidative stress downregulate all these three miRs, which promotes the expression of VEGF
. Thus oxidative stress along with VEGF contribute to the progression of DR.
Molecules Related to Inflammation During the development of PDR, infiltration and adhesion of inflammatory cells are common pathological manifestations. Inflammation is the central role in DR, and lots of immune cells, molecular mediators are also involved. In early stages of DR, inflammation plays a protective role against the apoptosis caused by hypoxia,which presents as a defensive reaction of the tissue, but in later stages, uncontrolled inflammation interplays with angiogenesis and coagulation, contributing to the development of DR
. Many inflammatory molecules have been detected in the vitreous of DR patients, and most of them are proteins regulated by nuclear transcription factors such as NF-κB. Here we summarize some inflammatory molecules in the vitreous which are involved in DR.
OTHER DIABETIC RETINOPATHY-RELATED MOLECULES IN THE VITREOUS BODY
In addition, neutrophil extracellular traps (NETs), another inflammation related products, has been found in the vitreous of DR patients. NETs is the product of neutrophil NETosis,a novel process of neutrophil death differing from necrosis and apoptosis. Studies have shown that under the induction of high glucose, NADPH oxidase participates in the formation of NETs in eye tissues, it is found that NETs in the vitreous of PDR patients is higher than those in normal people. Further experiments found that the content of NETs in the vitreous decreased after anti-VEGF treatment, suggesting that NETs may play a certain role in the occurrence and development of PDR and have a certain relationship with VEGF
.
(3) 综合考虑钢箱梁长度变化对主梁受力特性的影响规律以及对工程造价的影响,对于主跨240 m的钢-混凝土混合梁,钢箱梁长度取96 m是最佳选择。
Apart from NETs and LT, other inflammation-related molecules such as sCD200, nucleotide binding domain containing Pyrin domain 3, and leucine-rich repeat receptor (NLRP3)inflammasome have been found to have a higher level in the vitreous of PDR patients than that in control group
, and NLRP3 inflammasome pathway was associated with decreased vitamin D concentrations in the vitreous of PDR patients
.Besides, recent study has shown that content of 7 kinds of oxylipins including lipoxygenase (LOX)- and cytochrome P450 (CYP)-derived oxylipins in PDR patients discriminated from non-diabetic control, indicating an underlying imbalanced inflammation-resolution homeostasis in PDR
.
Another inflammatory mediator leukotriene (LT) also plays a critical role in DR. LTs in retina contribute to inflammatory response, oxidative stress and the expression of pro-angiogenic agents. As for relationship with inflammatory response,hyperglycemia induces inflammation, increases retinal leukostasis, and recruits LTs-producing leukocytes, which further aggravates the inflammatory response and forms a vicious circle. For oxidative stress, after ischemia reperfusion injury of retina, leukocytes produce more LTs which bind to receptors and reduce the scavenging of free radicals and activate NADPH oxidase, thus inducing oxidative stress
.Besides, LTs can activate MAPK pathway and induce the production of TNF-α, which increases the production of VEGF
and MMP-9
, together with Nox-1 after the activation of NF-κB in LTs
, these mechanisms contribute to retinal neovascularization.
In conclusion, inflammatory molecules play an important role in DR, and lots of factors have been identified (Figure 5). For VEGF takes part in the inflammatory response of the tissue,levels of most of these factors have close relationship with VEGF. It’s promising that these inflammatory molecules being the fundament to develop new treatment. But current studies concerning these factors haven’t figured out the exact mechanisms, so further researches are needed.
Molecules Related to Matrix Metalloproteinases MMPs are a large family of proteases that require the involvement of metal ions such as Ca
, Zn
to perform their functions.The concentration of MMPs in tissue is very low in normal adults, but under the condition of inflammation, high glucose or oxidative stress, the concentration of MMPs will be upregulated. Generally, MMPs play a role in tissue remodeling,organ growth and development, angiogenesis, inflammation,and cell migration
.
1、选取授课主题。可以针对农业生产实际问题、机器构造原理等,要抓住学员的兴趣点和共鸣点。例如,在农机安全生产方面,由于涉及学员切身安危,事故触目惊心,使人警醒,学员们在听到有关这些方面的内容案例时,往往注意力非常集中,不时地、不约而同地发出惋惜的声音。培训主题抓住这些兴趣点和共鸣点,能很好的提升授课培训质量。在讲解收割机构造和功能时,抓住问题导向,以收割机作业中的常见故障为切入点,对机具的部件、原理和功能进行讲解,既让学员明白了故障的处理,又让学员熟悉了机器的各个部件。
MMPs are also widely expressed in ocular tissue, and they are involved in the development of various ophthalmic diseases.Many studies have confirmed the vital role of MMPs in the process of DR. Although the specific mechanism is still unclear, it is widely accepted that in the presence of high glucose, hypoxia and inflammation, MMPs in the retina will be upregulated and degrade the extracellular matrix in the basement membrane of microvessels, thereby destroying blood-retinal barrier, leading to the changes in vascular permeability, which is the core pathological change of DR. At the same time, the degradation of the basement membrane will promote the migration of vascular endothelial cells, thereby forming new retinal vessels
. What’s more, MMPs can reshape the extracellular matrix, leading to severe lesions such as retinal hemorrhage, edema, and vitreous hemorrhage during the PDR stage
.
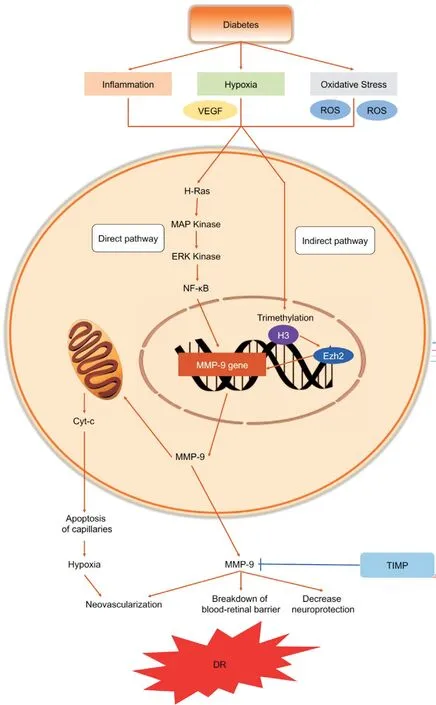
Current studies have found that levels of MMP-1, MMP-7,MMP-9 and MMP-14 are higher in the vitreous of PDR compared with control
. MMP-9, a gelatinase, is thought to be the most important MMPs in DR and has been greatly explored. High glucose induced inflammation, oxidative stress and hypoxia induced VEGF can stimulate MMP-9 through direct ways (induction of transcriptional factors to directly increase the expression of MMP-9) or indirect ways (epigenetic pathways). MMP-9 participates in the DR progression mainly through 3 ways (Figure 6). The first one is the angiogenesis.Interestingly, MMP-9 has dual role in angiogenesis. In early stages of DR, MMP-9 acts as an angiogenesis antagonist,for it can activate the angiostatin, which is an angiogenesis inhibitor
. Besides, MMP-9 contributes to the apoptosis of retinal capillary cells, thus inhibit the angiogenesis. The induction of apoptosis is mainly through the damage of mitochondria. Second, MMP-9 plays its role through the destruction of prominin-1/CD133, which is an important molecule in development, protection and regeneration of retina. The third is the breakdown of blood-retinal barrier.MMP-9 can break junctional complex molecules such as occludins and claudins, as well as degrade components of basement membrane, causing the breakdown of blood-retinal barrier
.
For the inhibition of MMPs, one research has analyzed the differences in the concentrations of four types of tissue inhibitor of matrix metalloprotease (TIMP), including TIMP-1, TIMP-2,TIMP-3, TIMP-4 in the vitreous of PDR patients. The results showed that compared with the control group, levels of TIMP-1 and TIMP-4 in the vitreous of PDR patients were significantly increased, while the TIMP-2 and TIMP-3 presented no significant difference, indicating that different types of TIMPs in the eye tissue expression differently and might play different role in DR
.
In addition to MMPs and TIMPs, some studies have also investigated extracellular MMP inducers (EMMPRIN) in DR.One research found that in the vitreous of PDR patients, the level of EMMPRIN was significantly higher than that of the control group and was positively correlated with MMP-1,MMP-9 and VEGF levels. In human retinal microvascular endothelial cells cultured
, EMMPRIN was found to induce the expression of MMP-1, HIF-1α and its downstream VEGF. It is speculated that EMMPRIN may have similar effect
.
Other Molecules that May be Related to Diabetic Retinopathy Apart from these four groups of molecules introduced above, there are many studies focusing on other molecules recently, but they have not been carried out in depth,so we will briefly introduce these progressions in this section.These molecules include adiponectin, certain specific amino acids, PIWI-like protein, renin receptor, non-coding RNA and so on.
Some researchers have studied the role of adiponectin (APN)in the development of DR. In other tissues throughout the body, APN is closely related to tissue fibrosis, but its effect differs among different tissues. In patients with PDR, the APN concentration in the vitreous was significantly higher than that in the control group, while the concentration in serum was significantly lower than that in the control group. Meanwhile,it was found that intraocular APN has the function of inhibiting new blood vessels, and making DR progress toward fibrosis. In addition, by observing the role of APN in PDR at different periods, the researchers found that APN may play a therapeutic role in the early stages of PDR, while in the later stages, it promotes fibrosis in the posterior segment of the eye,suggesting that APN functions differently in different stages of the disease
.
1.过渡:爸爸妈妈之间的爱都表现在生活中一些极其平凡简单的小事上。下面我们来重点读一读吃饺子这件事。看看在家里他们是怎样互相关爱的?
采用SPSS 19.0软件对数据进行分析处理,计量资料以(均数±标准差)表示,采用t检验;计数资料以(n,%)表示,采用χ2检验,以P<0.05表示差异具有统计学意义。
As for the role of certain amino acids in the development of DR in the vitreous, some studies have tested the concentration of hydroxyproline, proline, lysine, glycine and alanine in the vitreous, and found that the concentration of certain amino acids was significantly higher than that in control group. The possible mechanism for this phenomenon is these amino acids might induce the accumulation of triglycerides and APN,further produce adipogenesis, and at the same time increase the antioxidant capacity and reduce the levels of pro-angiogenic markers that may intensify disease. Therefore, researchers speculated that the increased content of these amino acids in the vitreous may have a protective effect
.
Researchers from India studied the P-element-introduced Wimpy Testis (PIWI) -like protein, Piwi like RNA-mediated gene silencing 2 (HIWI2). Western blot analyses found that the level of HIWI2 protein in the vitreous of PDR patients significantly increased compared to non-PDR patients. Further studies on human retinal pigment epithelial cells cultured
showed that the expression of HIWI2 protein was significantly increased under oxidative stress and VEGF condition, and the expression level was dose-dependent.In addition, after the HIWI2 gene was knocked out, VEGF and growth factor decreased significantly under oxidative stress, which is accompanied with the decrease of epithelial mesenchymal transition (EMT) biomarker. Thus, the HIWI2 protein may play several roles in the development of DR,including the regulation of VEGF, growth factors, and EMT
.New progress has also been made in research on the (pro) renin receptor [(P)RR]. (P)RR is a common receptor for renin and its precursors, and it is also a component of the renin-angiotensin system (RAS). Studies have found that a RAS-related protein system exists in human eye tissues, and the protein system can stimulate the expression of VEGF-A. At the same time,the concentration of (P)RR in the vitreous of PDR patients was positively correlated with renin, and VEGF, and was significantly higher than that in control group, suggesting that(P)RR is also closely related to VEGF-A-driven angiogenesis.This group of researchers also designed an RNA that can inhibit (P)RR, which they hope could depress angiogenesis by inhibit the translation of (P)RR. And further research is needed to clarify its therapeutic ability and feasibility of clinical application
.
Besides these proteins, non-coding RNA was also found to participate in the progression of DR in vitreous. It is reported that increased expression of HOX antisense intergenic RNA (HOTAIR) was observed in vitreous of PDR patients.HOTAIR usually exerted its capabilities by preventing oxidative stress and modulating epigenetic pathways involving histone methylation, histone acetylation, DNA methylation,and transcription factors, thus may function as a critical epigenetic mediator of angiogenesis in DR
. Another research also found that expression of non-coding RNA ANRIL was positively correlated with Ang II, p65 and VEGF expression in the vitreous of PDR patients
, and previous study has found that overexpression of ANRIL may be a result of the activation of the RAS and NF-κB pathway, thus ANRIL was confirmed to be associated with the onset of DR
. Expression of miR-409-5p was also found to increase in vitreous of PDR patients.As overexpression of miR-409-5p promotes the proliferation,migration, and tube formation, and increased VEGF expression and secretion, anti-miR-409-5p therapy may provide a novel strategy in treating DR
.
Another study focused on levels of vitamin C in the vitreous.Vitamin C is an anti-oxidant and thought to be related to oxidative stress in the eye. Researchers found that the level of vitamin C in PDR patients’ vitreous showed a tenfold decrease,and had correlation with the degree of macular ischemia.But whether these two phenomenon has causal relationship remains unknown
.
Other factors include osteoprotegerin (OPG)
, angiopoietinlike Protein 4 (ANGPTL-4)
and ANGPTL-8
, low-density lipoprotein receptor-related Protein 6 (LRP6)
, endocan
,
. have been found to be related to DR progression. These factors are higher in the vitreous of PDR patients than in the control group and are related to VEGF, but further research is needed to reveal their mechanism of action.
CONCLUSION
In the last decade, VEGF related research has made major breakthroughs in the pathogenesis of DR, and thus developed a highly specific anti-VEGF monoclonal antibody therapy,which is a milestone in the history of DR treatment. However,anti-VEGF treatment can only delay the disease progression,and it has problems such as high cost, short effective time,frequent intraocular injection, and drug resistance. Therefore,further exploration of DR-related pathogenesis and targeted treatment options are needed. This article reviews the clinical and basic research on the changes of intravitreal molecules in the development of DR, and summarizes researches on KKS pathway, oxidative stress, inflammation and MMPs-related pathways. In addition, the results of many studies on a single isolated molecule such as APN are also listed. By reviewing the research of DR-related molecules in the vitreous body in recent years, the author aims to provide inspirations for the study of DR mechanism and lay the molecular foundation for new treatment methods. Hope that related research will be applied to the clinic and set the next milestone for DR treatment.
ACKNOWLEDGEMENTS
Supported by the National Science and Technology Major Project (No.2018ZX10101004); Beijing Natural Science Foundation (No.7202229).Conflicts of Interest: Xia HQ, None; Yang JR, None; Zhang KX, None; Dong RL, None; Yuan H, None; Wang YC,None; Zhou H, None; Li XM, None.
1 Simó-Servat O, Hernández C, Simó R. Diabetic retinopathy in the context of patients with diabetes.
2019;62(4):211-217.
2 Wong TY, Cheung CMG, Larsen M, Sharma S, Simó R. Diabetic retinopathy.
2016;2:16012.
3 Liu R, Liu CM, Cui LL, Zhou L, Li N, Wei XD. Expression and significance of MiR-126 and VEGF in proliferative diabetic retinopathy.
2019;23(15):6387-6393.
4 Grauslund J. Vascular endothelial growth factor inhibition for proliferative diabetic retinopathy: Et Tu, Brute?
2017;95(8):757-758.
5 Loukovaara S, Nurkkala H, Tamene F, Gucciardo E, Liu XN,Repo P, Lehti K, Varjosalo M. Quantitative proteomics analysis of vitreous humor from diabetic retinopathy patients.
2015;14(12):5131-5143.
6 Nawaz IM, Rezzola S, Cancarini A, Russo A, Costagliola C, Semeraro F, Presta M. Human vitreous in proliferative diabetic retinopathy:Characterization and translational implications.
2019;72:100756.
7 Hernández C, dal Monte M, Simó R, Casini G. Neuroprotection as a therapeutic target for diabetic retinopathy.
2016;2016:9508541.
8 Wang W, Lo ACY. Diabetic retinopathy: pathophysiology and treatments.
2018;19(6):E1816.
9 Apte RS, Chen DS, Ferrara N. VEGF in signaling and disease: beyond discovery and development.
2019;176(6):1248-1264.
10 Othman R, Cagnone G, Joyal JS, Vaucher E, Couture R. Kinins and their receptors as potential therapeutic targets in retinal pathologies.
2021;10(8):1913.
11 Gao BB, Chen XH, Timothy N, Aiello LP, Feener EP. Characterization of the vitreous proteome in diabetes without diabetic retinopathy and diabetes with proliferative diabetic retinopathy.
2008;7(6):2516-2525.
12 Ehrenfeld P, Millan C, Matus CE, Figueroa JE, Burgos RA, Nualart F,Bhoola KD, Figueroa CD. Activation of kinin B1 receptors induces chemotaxis of human neutrophils.
2006;80(1):117-124.
13 Liu J, Feener EP. Plasma kallikrein-kinin system and diabetic retinopathy.
2013;394(3):319-328.
14 Kita T, Clermont AC, Murugesan N, Zhou QF, Fujisawa K, Ishibashi T, Aiello LP, Feener EP. Plasma kallikrein-kinin system as a VEGF-independent mediator of diabetic macular edema.
2015;64(10):3588-3599.
15 Tang M, He FP, Ma L, Liu P, Wang JW, Zhu XC. Bradykinin receptors in ischemic injury.
2018;15(4):359-366.
16 Hammes HP. Diabetic retinopathy: hyperglycaemia, oxidative stress and beyond.
2018;61(1):29-38.
17 Ighodaro OM. Molecular pathways associated with oxidative stress in diabetes mellitus.
2018;108:656-662.
18 Kowluru RA, Kowluru A, Mishra M, Kumar B. Oxidative stress and epigenetic modifications in the pathogenesis of diabetic retinopathy.
2015;48:40-61.
19 Grandl G, Wolfrum C. Hemostasis, endothelial stress, inflammation,and the metabolic syndrome.
2018;40(2):215-224.
20 Brzović-Šarić V, Landeka I, Šarić B, Barberić M, Andrijašević L,Cerovski B, Oršolić N, Đikić D. Levels of selected oxidative stress markers in the vitreous and serum of diabetic retinopathy patients.
2015;21:649-664.
21 Seko Y, Fujimura T, Yao T, Taka H, Mineki R, Okumura K, Murayama K. Secreted tyrosine sulfated-eIF5A mediates oxidative stress-induced apoptosis.
2015;5:13737.
22 Suzuki Y, Yao T, Okumura K, Seko Y, Kitano S. Elevation of the vitreous body concentrations of oxidative stress-responsive apoptosisinducing protein (ORAIP) in proliferative diabetic retinopathy.
2019;257(7):1519-1525.
23 McArthur K, Feng B, Wu Y, Chen S, Chakrabarti S. microRNA 200b regulates VEGF mediated alterations in diabetic retinopathy.
2011;60(4):1314-1323.
24 Tomasetti M, Nocchi L, Staffolani S, Manzella N, Amati M, Goodwin J, Kluckova K, Nguyen M, Strafella E, Bajzikova M, Peterka M, Lettlova S, Truksa J, Lee W, Dong LF, Santarelli L, Neuzil J.microRNA-126 suppresses mesothelioma malignancy by targeting IRS1 and interfering with the mitochondrial function.
2014;21(15):2109-2125.
25 Dan-Brezis I, Zahavi A, Axer-Siegel R, Nisgav Y, Dahbash M,Weinberger D, Ehrlich R, Livnat T. Inflammation, angiogenesis and coagulation interplay in a variety of retinal diseases.
2019.
26 Capitão M, Soares R. Angiogenesis and inflammation crosstalk in diabetic retinopathy.
2016;117(11):2443-2453.
27 Abu El-Asrar AM, Nawaz MI, Ahmad A, de Zutter A, Siddiquei MM, Blanter M, Allegaert E, Gikandi PW, de Hertogh G, van Damme J, Opdenakker G, Struyf S. Evaluation of proteoforms of the transmembrane chemokines CXCL16 and CX3CL1, their receptors,and their processing metalloproteinases ADAM10 and ADAM17 in proliferative diabetic retinopathy.
2020;11:601639.
28 Tsai T, Kuehn S, Tsiampalis N, Vu MK, Kakkassery V, Stute G, Dick HB, Joachim SC. Anti-inflammatory cytokine and angiogenic factors levels in vitreous samples of diabetic retinopathy patients.
2018;13(3):e0194603.
29 Yoshida S, Kubo Y, Kobayashi Y, Zhou YD, Nakama T, Yamaguchi M,Tachibana T, Ishikawa K, Arita R, Nakao S, Sassa Y, Oshima Y, Kono T,Ishibashi T. Increased vitreous concentrations of MCP-1 and IL-6 after vitrectomy in patients with proliferative diabetic retinopathy: possible association with postoperative macular oedema.
2015;99(7):960-966.
30 Zhao MM, Hu YG, Yu Y, Lin Q, Yang JH, Su SB, Xu GT, Yang TS.Involvement of IL-37 in the pathogenesis of proliferative diabetic retinopathy.
2016;57(7):2955-2962.
31 Wang L, Zhou X, Yin YZ, Mai YX, Wang DS, Zhang XD.Hyperglycemia induces neutrophil extracellular traps formation through an NADPH oxidase-dependent pathway in diabetic retinopathy.
2018;9:3076.
32 Behl T, Kaur I, Kotwani A. Role of leukotrienes in diabetic retinopathy.
2016;122:1-9.
33 Duah E, Adapala RK, Al-Azzam N, Kondeti V, Gombedza F, Thodeti CK, Paruchuri S. Cysteinyl leukotrienes regulate endothelial cell inflammatory and proliferative signals through CysLT2 and CysLT1 receptors.
2013;3:3274.
34 Ichiyama T, Kajimoto M, Hasegawa M, Hashimoto K, Matsubara T,Furukawa S. Cysteinyl leukotrienes enhance tumour necrosis factoralpha-induced matrix metalloproteinase-9 in human monocytes/macrophages.
2007;37(4):608-614.
35 Kim GY, Lee JW, Ryu HC, Wei JD, Seong CM, Kim JH.Proinflammatory cytokine IL-1beta stimulates IL-8 synthesis in mast cells
a leukotriene B4 receptor 2-linked pathway, contributing to angiogenesis.
2010;184(7):3946-3954.
36 Xu Y, Cheng QC, Yang BY, Yu SS, Xu F, Lu L, Liang XL. Increased sCD200 levels in vitreous of patients with proliferative diabetic retinopathy and its correlation with VEGF and proinflammatory cytokines.
2015;56(11):6565-6572.
37 Loukovaara S, Piippo N, Kinnunen K, Hytti M, Kaarniranta K,Kauppinen A. NLRP3 inflammasome activation is associated with proliferative diabetic retinopathy.
2017;95(8):803-808.
38 Lu L, Zou GC, Chen L, Lu QY, Wu M, Li CX. Elevated NLRP3 inflammasome levels correlate with vitamin D in the vitreous of proliferative diabetic retinopathy.
(
)2021;8:736316.
39 Zhao TT, Wang YB, Guo XJ, Li HL, Jiang WM, Xiao YY, Deng B,Sun Y. Altered oxylipin levels in human vitreous indicate imbalance in pro-/ anti-inflammatory homeostasis in proliferative diabetic retinopathy.
2022;214:108799.
40 Solanki A, Bhatt LK, Johnston TP, Prabhavalkar KS. Targeting matrix metalloproteinases for diabetic retinopathy: the way ahead?
2019;20(4):324-333.
41 Cabral-Pacheco GA, Garza-Veloz I, Castruita-De la Rosa C, Ramirez-Acuña JM, Perez-Romero BA, Guerrero-Rodriguez JF, Martinez-Avila N, Martinez-Fierro ML. The roles of matrix metalloproteinases and their inhibitors in human diseases.
2020;21(24):9739.
42 Opdenakker G, Abu El-Asrar A. Metalloproteinases mediate diabetesinduced retinal neuropathy and vasculopathy.
2019;76(16):3157-3166.
43 Chung AWY, Hsiang YN, Matzke LA, McManus BM, van Breemen C,Okon EB. Reduced expression of vascular endothelial growth factor paralleled with the increased angiostatin expression resulting from the upregulated activities of matrix metalloproteinase-2 and-9 in human type 2 diabetic arterial vasculature.
2006;99(2):140-148.
44 Abu El-Asrar AM, Ahmad A, Bittoun E, Siddiquei MM, Mohammad G, Mousa A, de Hertogh G, Opdenakker G. Differential expression and localization of human tissue inhibitors of metalloproteinases in proliferative diabetic retinopathy.
2018;96(1):e27-e37.
45 Abu El-Asrar AM, Ahmad A, Alam K, Siddiquei MM, Mohammad G, Hertogh G, Mousa A, Opdenakker G. Extracellular matrix metalloproteinase inducer (EMMPRIN) is a potential biomarker of angiogenesis in proliferative diabetic retinopathy.
2017;95(7):697-704.
46 Palanisamy K, Raman R, Sulochana KN, Chidambaram S.Adiponectin: a potential candidate for treating fibrosis in posterior segment of the eye.
2019;123:9-12.
47 Vidhya S, Ramya R, Coral K, Sulochana KN, Bharathidevi SR.Free amino acids hydroxyproline, lysine, and glycine promote differentiation of retinal pericytes to adipocytes: a protective role against proliferative diabetic retinopathy.
2018;173:179-187.
48 Sivagurunathan S, Raman R, Chidambaram S. PIWI-like protein,HIWI2: a novel player in proliferative diabetic retinopathy.
2018;177:191-196.
49 Kanda A, Ishida S. (Pro)renin receptor: involvement in diabetic retinopathy and development of molecular targeted therapy.
2019;10(1):6-17.
50 Biswas S, Feng B, Chen SL, Liu JT, Aref-Eshghi E, Gonder J, Ngo V,Sadikovic B, Chakrabarti S. The long non-coding RNA HOTAIR is a critical epigenetic mediator of angiogenesis in diabetic retinopathy.
2021;62(3):20.
51 Chen SZ, Zhong HM, Wang Y, Wang ZH, Liang XQ, Li SQ, Li ZH,Yu ZT, Li LY, Yi GG, Fu M. The clinical significance of long noncoding RNA ANRIL level in diabetic retinopathy.
2020;57(4):409-418.
52 Zhang B, Wang D, Ji TF, Shi L, Yu JL. Overexpression of lncRNA ANRIL up-regulates VEGF expression and promotes angiogenesis of diabetes mellitus combined with cerebral infarction by activating NF-κB signaling pathway in a rat model.
2017;8(10):17347-17359.
53 Wang Y, Lin WW, Ju JH. microRNA-409-5p promotes retinal neovascularization in diabetic retinopathy.
2020;19(11):1314-1325.
54 Park SW, Ghim W, Oh S, Kim Y, Park UC, Kang J, Yu HG. Association of vitreous vitamin C depletion with diabetic macular ischemia in proliferative diabetic retinopathy.
2019;14(6):e0218433.
55 Abu El-Asrar AM, Struyf S, Mohammad G, Gouwy M, Rytinx P, Siddiquei MM, Hernández C, Alam K, Mousa A, de Hertogh G, Opdenakker G, Simó R. Osteoprotegerin is a new regulator of inflammation and angiogenesis in proliferative diabetic retinopathy.
2017;58(7):3189-3201.
56 Lu QY, Zou WJ, Chen B, Zou C, Zhao MJ, Zheng Z. ANGPTL-4 correlates with vascular endothelial growth factor in patients with proliferative diabetic retinopathy.
2016;254(7):1281-1288.
57 Lu QY, Lu L, Chen W, Lu PR. Expression of angiopoietin-like protein 8 correlates with VEGF in patients with proliferative diabetic retinopathy.
2017;255(8):1515-1523.
58 Gao XX, Ma K, Lu N, Xu YS, Hong TT, Peng XY. Elevated LRP6 levels correlate with vascular endothelial growth factor in the vitreous of proliferative diabetic retinopathy.
2015;21:665-672.
59 Abu El-Asrar AM, Nawaz MI, de Hertogh G, Al-Kharashi AS, van den Eynde K, Mohammad G, Geboes K. The angiogenic biomarker endocan is upregulated in proliferative diabetic retinopathy and correlates with vascular endothelial growth factor.
2015;40(3):321-331.
 International Journal of Ophthalmology2022年7期
International Journal of Ophthalmology2022年7期
- International Journal of Ophthalmology的其它文章
- Impact of OCT scan-patterns in identifying morphological features of lamellar macular holes and macular pseudoholes
- Virtual reality training improves accommodative facility and accommodative range
- Short-term effect of 0.01% atropine sulphate eye gel on myopia progression in children
- Reduced choroidal peripapillary capillaries in thyroidassociated ophthalmopathy with early stage of dysthyroid optic neuropathy
- Incidence of ocular manifestations in patients with graft versus host disease after allogeneic stem cell transplant in Riyadh, Saudi Arabia
- Clinical features, surgical outcomes and genetic analysis of ectodermal dysplasia with ocular diseases
