Goal-directed fluid therapy in gastrointestinal cancer surgery: A prospective randomized study
Duygu Akyol, Zafer Cukurova, Evrim Kucur Tulubas, Güneş Özlem Yıldız, Mehmet Süleyman Sabaz
1Department of Anesthesiology and Reanimation, Başakşehir Çam and Sakura City Hospital, Istanbul, Turkey
2Department of Anesthesiology and Reanimation, Bakirkoy Dr.Sadi Konuk Training and Research Hospital, University of Health Sciences, Istanbul, Turkey
3Department of Critical Care Medicine, Marmara University Pendik Training and Research Hospital, Marmara University School of Medicine, Istanbul, Turkey
ABSTRACT Objective: To investigate the effects of perioperative goal-directed fluid therapy (GDFT) on intraoperative fluid balance, postoperative morbidity, and mortality.Methods: This is a prospective randomized study, and 90 patients who underwent elective open gastrointestinal cancer surgery between April 2017 and May 2018 were included.Patients were randomized into 2 groups that received liberal fluid therapy (the LFT group, n=45) and goal-directed fluid therapy (the GDFT group, n=45).Patients’ Colorectal Physiologic and Operative Severity Score for the enUmeration of Mortality and Morbidity (CR-POSSUM) physiological score, Charlson Comorbidity Index (CCI), perioperative vasopressor and inotrope use, postoperative AKIN classification, postoperative intensive care unit (ICU) hospitalization, hospital stay, and 30-day mortality were recorded.Results: The volume of crystalloid used perioperatively and the total volume of fluid were significantly lower in the GDFT group compared to the LFT group (P<0.05).CR-POSSUM physiological score and CCI were significantly higher in the GDFT group (P<0.05).Although perioperative vasopressor and inotrope use was significantly higher in the GDFT group (P<0.05), postoperative acute kidney injury development was not affected.Postoperative mortality was determined to be similar in both groups (P>0.05).Conclusion: Although GDFT was demonstrated to be a good alternative method to LFT in open gastrointestinal cancer surgery, and it can prevent perioperative fluid overload, and the postoperative results are comparable in the two groups.
KEYWORDS: Goal-directed fluid therapy; Liberal fluid therapy; Stroke volume variation; Open gastrointestinal cancer surgery
1.Introduction
Gastrointestinal cancer surgery management strategy in open abdominal surgery affects anesthesia management both in the preoperative and perioperative periods.One of them is perioperative fluid management.Optimal fluid therapy and adequate organ and tissue perfusion is the priority of Enhanced Recovery After Surgery protocol.Perioperative fluid management in gastrointestinal cancer surgeries affects morbidity and mortality and requires a multidisciplinary approach.Many studies are currently being carried out for fluid treatments, and new fluid management protocols are being developed instead of traditional methods[1,2].In the management of perioperative fluid overload and restrictive fluid, goal-directed fluid therapy (GDFT) and euvolemic fluid replacement have recently been recommended due to increased postoperative complications and increased hospital stay[3].There are many studies demonstrating that perioperative GDFT help decreasing postoperative morbidity and hospital stay, and improve postoperative outcomes[4-6].Pulse contour analysis method, which is a minimally invasive method, and stroke volume variation (SVV) and noninvasive pleth variability index method can be used for the optimization of cardiac output in GDFT.FloTracVigileo® monitoring is a minimally invasive cardiac output monitor that calculates SVV by performing arterial wave analysis[7].It can be considered as a good predictor in assessing SVV fluid response[8].
The primary aim of our study is to assess the effect of GDFT on intraoperative fluid balance and hemodynamics in open gastrointestinal cancer surgeries.The secondary aim is to compare their effects on postoperative mortality and morbidity.
2.Patients and methods
2.1.Study design and ethical consideration
This study is a single-center, prospective, and randomized clinical trial.Our study was designed per the Declaration of Helsinki, and the local ethics committee approval was obtained from Bakırköy Dr.Sadi Konuk Training and Research Hospital (approval number: 2017-165, approval date: 19.06.2017).Written informed consent was obtained from all patients in this study before the enrollment in the study.
2.2.Inclusion and exclusion criteria
Patients aged 18-64 years, who underwent open gastrointestinal cancer surgery between April 2017 and May 2018, with an American Society of Anesthesiologists (ASA) score of Ⅱ-Ⅲ were included in the study.
The Patients with peripheral arterial disease, preoperative left ventricular ejection fraction <40% and those with heart failure, cardiac arrhythmias, the patients requiring massive blood transfusion, and patients with severe hepatic and renal failure were excluded from the study.
2.3.Grouping
The patients were randomized into two groups at the ratio of 1:1 using the MedCalc 18.2.1 software in an electronic environment: the GDFT group (SVV-guided fluid management) and the LFT group (conventional observational fluid management) (Figure 1).Although the gastrointestinal surgical team was the same, randomization could not be applied to the surgeon who performed the operation primarily and the primary surgeon could not be selected.
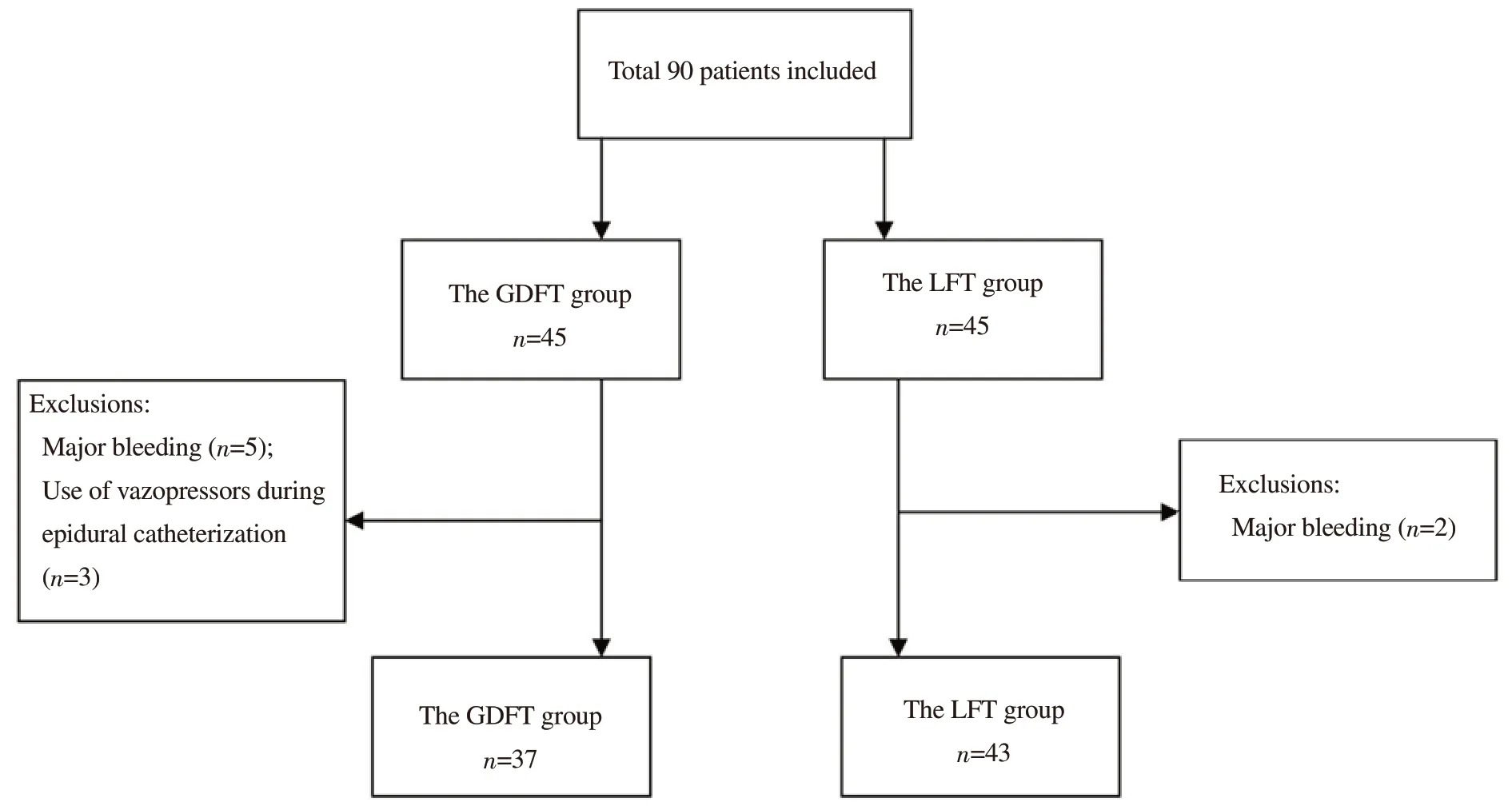
Figure 1.The study flowchart.GDFT: Goal-directed fluid therapy; LFT: Liberal fluid therapy.
2.4.Pre-operation management
Routine intraoperative monitoring [heart rate (HR), blood pressure (BP), electrocardiogram (ECG), oxygen saturation (SpO2)] was performed for each patient taken to the operating table following the ASA guideline.Crystalloid (isolyte) infusion was started routinely at 5 mL/kg/h for the patients and continued perioperatively.For postoperative analgesia, an epidural catheter was inserted through the thoracic 10-11 space.Sedation was performed for the patients with 0.03 mg/kg midazolam and arterial monitoring was provided with radial artery cannulation.
Induction was performed for all the patients with 1-2 μg/kg fentanyl and 2-3 mg/kg propofol, and they were curarized with 0.6 mg/kg rocuronium and intubated orotracheally.Volume control mode was set by adjusting the tidal volume to 8 mL/kg, positive end-expiratory pressure: 5, and respiratory rate end-tidal carbon dioxide pressure to 35-45 mmHg according to the ideal body weight of the patients.Then, a right internal jugular vein catheter was inserted under ultrasound guidance, following the rules of asepsis.Sevoflurane (MAC 0.7-1) and remifentanyl infusion (0.05-0.3 μg/kg/min) were used for anesthesia.
Minimally invasive monitoring ( FloTracVigileo® Edwards Lifesciences SL 4.0) was performed by providing radial artery cannulation (20 G) and internal jugular vein catheterization in the GDFT group, and continuous mean arterial pressure (MAP), peak heart rate, SVV, central venous pressure (CVP), Systemic Vascular Resistance Index and Cardiac Index (CI) were measured with this monitoring.After monitoring, blood gas was taken and the initial value was considered as Time-1 (T1).MAP was recorded every 5 min; CVP, CI, SVV, blood gas values (lactate), partial oxygen pressure (PaO2) at 30-minute intervals in a time frame of 240 min (T1, T2, T3, T4, T5, T6, T7, T8, T9) were recorded.
In the LFT group, monitoring was performed with radial artery cannulation and central jugular venous catheterization, and MAP was recorded at 5-minute intervals, and CVP, blood gas values (lactate, PaO2) at 30-minute intervals in a time frame of 240 min (T1, T2, T3, T4, T5, T6, T7, T8, T9) were recorded.
2.5.Perioperative fluid management
2.5.1.The GDFT group
Fluid management was performed according to SVV and CI followup.When the SVV was >10% (n=21) in the patients, 250 cc colloid was given, and when the SVV≤10% in the control measurement, standard (5 mL/kg/h) crystalloid infusion was continued.If the SVV was still >10% in the control measurement, 250 cc of colloid were administered as a second fluid bolus, and standard crystalloid infusion was administered when the SVV was <10%.
If SVV is still >10% after mini food challenges, erythrocyte suspension and fresh frozen plasma were replaced with a target hemoglobin value of 7-9 g/dL when Hct was <30% in patients with coronary artery disease (CAD), and when Hct was 25% in other patient groups[22].If SVV>10%, despite blood product replacement, and CI was below 2.5 L/min/m2, noradrenaline infusion was started.When SVV<10% and CI was <2.5 L/min/m2, dopamine infusion was started (Supplementary Figure 1).
2.5.2.The LFT group
Fluid management was performed according to MAP, HR, and urine output.Fluid bolus was administered when <0.5 mL/kg/h, MAP 65 mmHg, HR 100/min, and CVP decreased by 20% compared to the basal value in the perioperative urine volume follow-up.When Hct was <30% in patients with coronary artery disease and 25% in others, erythrocyte suspension and fresh frozen plasma were replaced with a target hemoglobin value of 7-9 g/dL.Vasopressor and inotrope infusion (noradrenaline and dopamine) was started for the patient who was hemodynamically unstable despite adequate fluid and blood product replacement.
In both groups, the duration of the operation, the volume of fluid, and the number of blood products were recorded.The patients who were admitted to the postoperative intensive care unit and indicated for intensive care after the preoperative examination were admitted as planned hospitalization and the patients with perioperative surgical complications who were hemodynamically unstable, the patients using vasopressor and inotrope, and the patients with respiratory problems despite no preoperative intensive care indication were admitted as unplanned hospitalization.The creatinine, neutrophil/lymphocyte values were recorded in all patients at the postoperative 1st and 24th hours.AKIN (acute kidney injury network) classification was made according to the creatinine values measured on the 1st preoperative and postoperative days.Postoperative hospital stay, surgical and pulmonary complications, vasopressor and inotrope requirement, and the length of stay in the intensive care unit (ICU) if hospitalized in the intensive care unit were monitored.
2.6.Statistical evaluation
Analyses were performed using NCSS 11 (Number Cruncher Statistical System, 2017 Statistical Software).In our study, frequency and percentage values were given for the variables.Mean±standard deviation, median (IOR), values were given for continuous variables.The normal distribution test of continuous variables was performed with the Kolmogorov-Smirnov test.Chi-square analysis was used for the relationship between categorical variables.Categorical variables were assessed with Fisher’s exact test and Fisher Freeman Halton test when appropriate.An independent sample t-test was used to compare two groups in continuous independent variables with normal distribution.The Mann-Whitney U test was used in the comparison of two independent groups for the variables that did not meet the assumption of normal distribution.The significant level of this study was set α=0.05.
3.Results
A total of 90 patients who undergone open gastrointestinal cancer surgery during the study period were divided into two groups as the GDFT group (n=37) and the LFT group (n=43).The demographic data, physiological and surgical scores, and operative time of the patients are presented in Table 1.Mean age, body mass index, and operative time were found to be similar in both groups (P>0.05).Considering the surgical diagnoses, the diagnoses of colon, stomach, pancreatic, and liver cancers were similar (P=0.28).In the GDFT group, it was determined that there were more males and that CR-POSSUM physiological score and CCI were higher (P<0.05).
Although the perioperative crystalloid use and total fluid volume were less in the GDFT group, the volume of colloid used was found to be higher (P<0.01).Vasopressor and inotrope use was found to be more frequent in the GDFT group (P<0.01).The volume of perioperative urine, total bleeding, and the volume of blood product used were found to be similar in both groups (Table 2). Perioperatively evaluated blood gas values (lactate, PaO2), CVP and MAP values are presented in Figure 2.The CVP values in the GDFT group were found to be statistically and significantly higher at T2, T3, T4 time periods (P<0.05).PaO2and MAP values were found to be similar in both groups (P>0.05).
The comparison of preoperative and postoperative creatinine and neutrophil/lymphocyte values between and within groups and the staging of AKIN between groups were conducted.Although preoperative and postoperative creatinine values were found to be significantly higher (P<0.05) in the GDFT group, the postoperative AKIN staging was similar (P>0.05).It was observed that postoperative neutrophil-lymphocyte ratio (NLR) increased significantly in both groups compared to preoperative values (P<0.01) (Figure 3).

Figure 3.Peroperative central venous pressure, mean arterial pressure, lactate, and PaO2. CVP: Central venous pressure; MAP: Mean arterial pressure.Lactate, central venous pressure, and PaO2 at 30-minute intervals in a time frame of 240 min (T1, T2, T3, T4, T5, T6, T7, T8, T9) were recorded, and mean arterial pressure was recorded at 5-minute intervals.*: P<0.05.
Mortality, anastomotic leakage, vasopressor and inotrope use were similar in both groups in the postoperative 30-day period.The length of stay in the intensive care unit and hospital was found to be similar in both groups (P>0.05) (Table 4).

Table 1.Comparison of patients’ demographic data, diagnosis, operative times, CR-POSSUM staging, mortality,and CCI scoring.

Table 2.Comparison of perioperative volume of fluid administered, bleeding, blood products, and patients using vasopressor and inotrope.
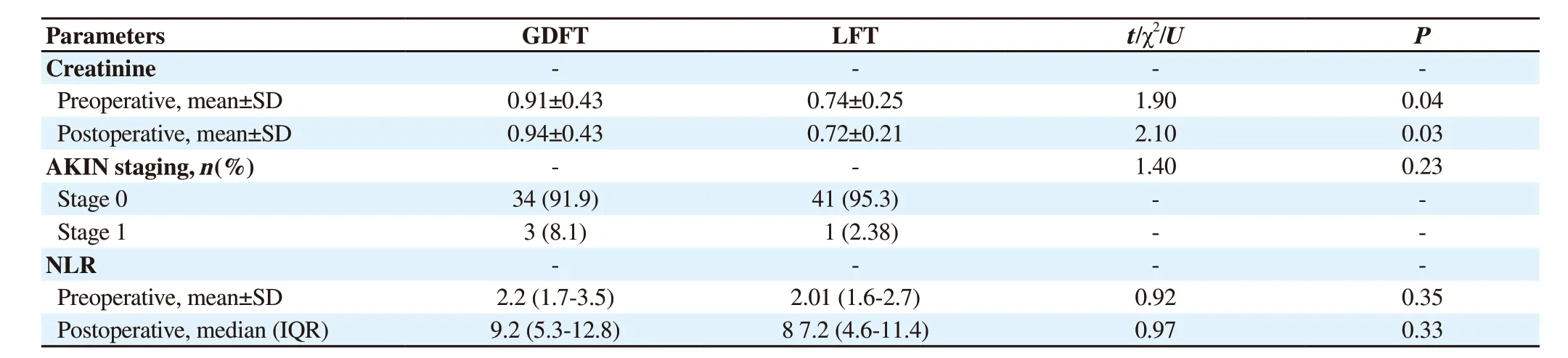
Table 3.Preoperative and postoperative creatinine and neutrophil/lymphocyte of the two groups.
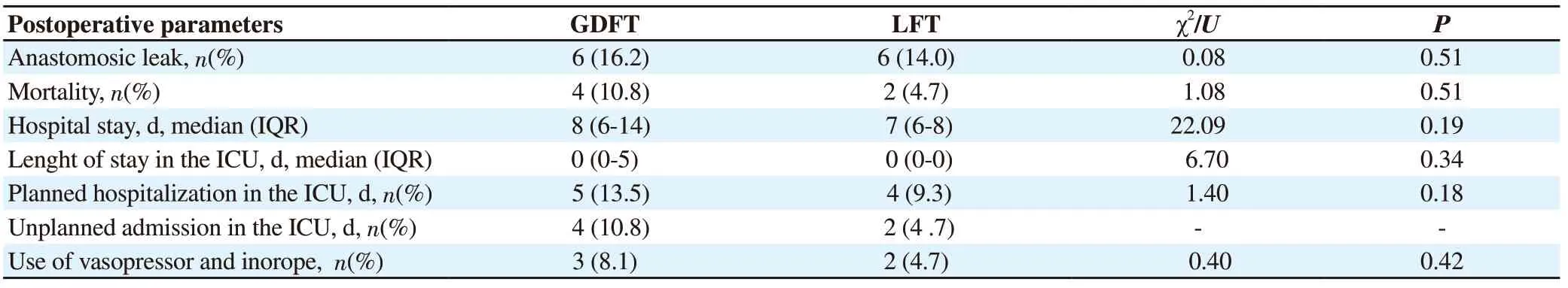
Table 4.Comparison of postoperative parameters between groups.
4.Discussion
In this study, we compared the effect of GDFT and LFT on intraoperative fluid balance, postoperative morbidity, and mortality in open gastrointestinal cancer surgeries, and the perioperatively used crystalloid and total fluid load were found to be at a lower level in the GDFT group.The effect of perioperative fluid management on the postoperative period in major gastrointestinal open cancer surgeries was discussed.Undesirable results may occur due to hypovolemia (decrease in CO, decrease in splenic perfusion, deterioration in tissue oxygenation) with restrictive fluid treatment and due to excessive fluid load (weight gain, pulmonary-peripheral edema, deterioration in oxygenation) with liberal fluid therapy.Consequently, the length of hospital stay, postoperative cost, morbidity, and mortality will rise[9].To avoid these terrible situations, much effort was pooled to protect patients from the undesirable effects of hypervolemia or hypovolemia, thus, the GDFT method has gained currency[3].With the patients being euvolemic, this fluid balance has positive effects on postoperative recovery, early mobilization, postoperative complications, and length of hospital stay[10-13].
More colloid was used in the GDFT group as we applied colloid bolus to provide hemodynamic stability in patients according to SVV and CI.Although many studies have demonstrated that the use of colloids is higher with GDFT than with crystalloids, the total volume of fluid used has been found to be less[12-16].Kumar et al.have found that the total volume of fluid used in the SVV group was less in patients undergoing major surgery[17].In our study, we provided perioperative oxygenation and hemodynamic stability in the GDFT group similar with the other group, with less fluid therapy and by protecting the patients from fluid overload, to dampen the side effects of hypervolemia.
There are various assumptions that affect postoperative complications, such as preoperative patient characteristics, perioperative hemodynamic follow-up, fluid management strategy, and surgical management.Although the CCI and CR-POSSUM physiological scores were higher due to the high comorbidities of the patients included in the GDFT group in our study, the results were similar between the groups in terms of postoperative morbidity and complications, and our results are in line with many other studies[18-22].In the meta-analyses performed, the superiority of GDFT could not be demonstrated in the assessment of the length of stay in the hospital and the intensive care unit and postoperative mortality[23,24].Although the patients in the preoperative GDFT group were at higher risk, we think that postoperative results were improved by optimizing perioperative hemodynamic follow-up and fluid management.
In our study, although the preoperative creatinine value was higher in the GDFT group (P<0.05), we found no statistical difference according to AKIN staging.Süner et al.have determined in their study that the preoperative and postoperative creatinine values are similar in the patients undergoing major surgery[25].This demonstrated that, although the preoperative creatinine values of the patients in the GDFT group are high, postoperative renal failure can be prevented by perioperative fluid optimization.
Previous studies have demonstrated the prognostic importance of NLR in cancer patients in terms of postoperative morbidity and mortality[26,27].Also in our study, preoperative and postoperative NLR were similar, and postoperative complications and mortality were similar between the groups.
Limitations of our study: The inhomogeneity between the two groups in terms of preoperative CCI and Physiological POSSUM caused confusion in the assessment in terms of postoperative complications.In our prospective randomized study, no special distinction was made regarding gender selection in the separation of patients groups.Although randomization was performed electronically using MedCalc 18.2.1 software, male gender was significantly higher in the GDFT group than in the LFT group.The gender difference also limits our generalization of our results.Furthermore, the fact that our study was conducted in a single center affected the generalization of the results.For GDFT to become a standard protocol in major or high-risk surgery, there is a need for more homogeneous study groups and prospective randomized studies with larger samples.
Although GDFT was demonstrated to be a good alternative method to LFT in gastrointestinal cancer surgery, and it was demonstrated to prevent perioperative fluid overload, but it was not demonstrated to be better in terms of postoperative results.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
D.A.: Concept, design, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing and manuscript review; Z.C.: Literature search, clinical studies, manuscript preparation, manuscript editing and manuscript review; E.K.T.: Concept, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing and manuscript review; G.Ö.Y.: Manuscript preparation, manuscript editing and manuscript review; M.S.S.: Literature search, data analysis, statistical analysis, manuscript preparation, manuscript editing and manuscript review.
 Journal of Acute Disease2022年2期
Journal of Acute Disease2022年2期
- Journal of Acute Disease的其它文章
- Electrocardiographic abnormalities in prevalent infections in tropical regions: A scoping review
- Comparative study on effects of dexmedetomidine and dexamethasone on the incidence of postoperative nausea and vomiting in patients undergoing laparoscopic surgery
- Effect of cold weather on carotid artery stenosis and occlusion: A retrospective observational study
- Body mass index and COVID-19 outcomes: A retrospective crosssectional study at a tertiary care center in India
- Mortality characteristics during the two waves of COVID-19 in India: A retrospective observational study
- An alveolate kidney: A case report of emphysema pyelonephritis
