LEEP术在绝经后高级别CIN患者诊疗的价值评估
陶恬阗,江海燕
(浙江省衢州市妇幼保健院,浙江 衢州 324000)
LEEP术在绝经后高级别CIN患者诊疗的价值评估
陶恬阗,江海燕
(浙江省衢州市妇幼保健院,浙江 衢州 324000)
[摘要]目的探讨LEEP术在绝经后高级别CIN患者中的诊疗价值。方法对2008年1月至2015年12月于浙江省衢州市妇幼保健院行子宫颈LEEP术的354例患者临床资料进行分析,以绝经后患者36例为实验组,同期1:3选择绝经前患者108例为对照组,分析临床症状、细胞学检查、HR-HPV检查、阴道镜检查及LEEP术后病理结果。结果实验组阴道镜检查满意率显著低于对照组(χ2=17.779,P=0.000)。以LEEP术后病理结果为诊断金标准,实验组LEEP术后病理级别升级者显著高于对照组(χ2=4.866,P=0.027),实验组阴道镜下活检病理的准确性显著低于对照组(χ2=3.992,P=0.046)。实验组患者行LEEP术后病理结果提示切缘阳性率高于对照组,但两组间无显著性差异(χ2=3.416,P=0.065),其中实验组内切缘阳性率明显高于对照组,两组间差异有显著性意义(χ2=5.797,P=0.016);实验组外切缘阳性率高于对照组,但两组间无显著性差异(χ2=0.254,P=0.615)。结论绝经后女性仍建议定期行宫颈癌筛查,包括宫颈TCT及HR-HPV检测。绝经后患者的阴道镜检查满意率及准确性均下降;对阴道镜活检后诊为CIN的患者应行LEEP进一步确诊诊断。
[关键词]子宫颈鳞状上皮内瘤变;子宫颈线圈电切术;高危型人乳头瘤病毒;绝经后
1资料和方法
1.1一般资料
2008年1月至2015年12月就诊于衢州市妇幼保健院医院接受LEEP术的高级别CIN患者共354例,其中绝经后CIN患者36例为实验组,平均年龄约56岁(45~71岁);1:3选取同期接受LEEP术(手术时间±1周)的高级别CIN绝经前患者108例为对照组,平均年龄约35岁(20~52岁)。患者行子宫颈LEEP术前均签署知情同意书。
1.2方法
记录患者术前子宫颈脱落细胞液基细胞学(liquid based cytology,LBC)及高危人乳头瘤病毒(high risk-human palillomavirus,HR-HPV)检查结果、阴道镜检查结果以及最终病理检查结果,并进行比较。HPV-DNA检测采用亚能生物技术有限公司的HPV基因分型检测试剂盒,采用杂交捕获(HC-Ⅱ)技术,检测13种与宫颈癌相关的HR-HPV(包括16、18、3l、33、35、39、45、51、52、56、58、59、68),按试剂盒诊断标准HR-HPV DNA≥1.0pg/mL为阳性。
1.3 LEEP术及病理检查
普通电刀采用ERBE ICC 300(德国Elektromedizin Tubingen产品),频率6~7MHz,电切功率设定为50~55W,电凝功率设定为45~50W。标本自子宫颈12点处将子宫颈纵行打开,由左向右将其展开、固定的子宫颈,根据组织体积取材8~20块,顺时针依次标记。所有病理检查均由专业病理医师做出诊断。出血量评估方法:由术者和麻醉师共同评估负压瓶中的出血量;术中纱布的出血量按大纱每块湿透约50mL,小纱每块湿透30mL估算、辅料的出血量按面积法估算,累计计算术中出血总量。
1.4统计学方法

TIAN Bing, WANG Tie-gong, YANG Peng-fei, YIN Wei, XU Bing, CHEN Lu-guang, LIU Qi, LIU Jian-min, LU Jian-ping
2结果
2.1两组患者术前临床特征
本研究实验组出现临床症状者14例,其中异常阴道流血者9例(25.00%),白带异常者3例(8.33%),不明原因腰酸者2例(5.56%);对照组出现临床症状者51例,其中异常阴道流血者28例(25.93%),白带异常者18例(16.67%),不明原因腰酸者5例(4.63%)。两组间临床症状比较无显著性差异(χ2=0.757,P=0.384)。
2.2两组患者术前实验室检查
实验组中32例接受LBC检查,其中细胞学检查与LEEP术后病检结果相符者为18例(56.3%);对照组中97例接受LBC检查,其中59例与LEEP术后病检结果相符(60.8%)。两组间比较无显著性差异(χ2=0.209,P=0.647)。实验组中25例接受HR-HPV检查,阳性率约80.0%,而对照组中接受HR-HPV者82例,其中阳性率约为89.0%。两组间比较无显著性差异差(χ2=1.372,P=0.241)。
2.3两组患者阴道镜检查满意率及手术前后病理级别比较
实验组共29例接受阴道镜检查+活检,其中提示宫颈慢性炎者3例,低级别CIN者4例,高级别CIN者22例;对照组中共92例接受阴道镜检查+活检,提示宫颈慢性炎者4例,低级别CIN者5例,高级别CIN者83例。实验组阴道镜检查满意率显著低于对照组,两组间差异有统计学意义(P=0.000)。以LEEP术后病理结果为诊断金标准,实验组LEEP术后病理级别升级者显著高于对照组,两组间差异有统计学意义(P=0.027),其中实验组LEEP术后确诊宫颈浸润癌2例,对照组术后确诊宫颈浸润癌者1例;实验组阴道镜下活检病理的准确性显著低于对照组,两组间差异有统计学意义(P=0.046),见表1。
表1绝经前后阴道镜检查满意率及病理级别一致性[n(%)]
Table1Satisfactory rate of colposcopy before and after menopause and the consistency of pathological grade[n(%)]
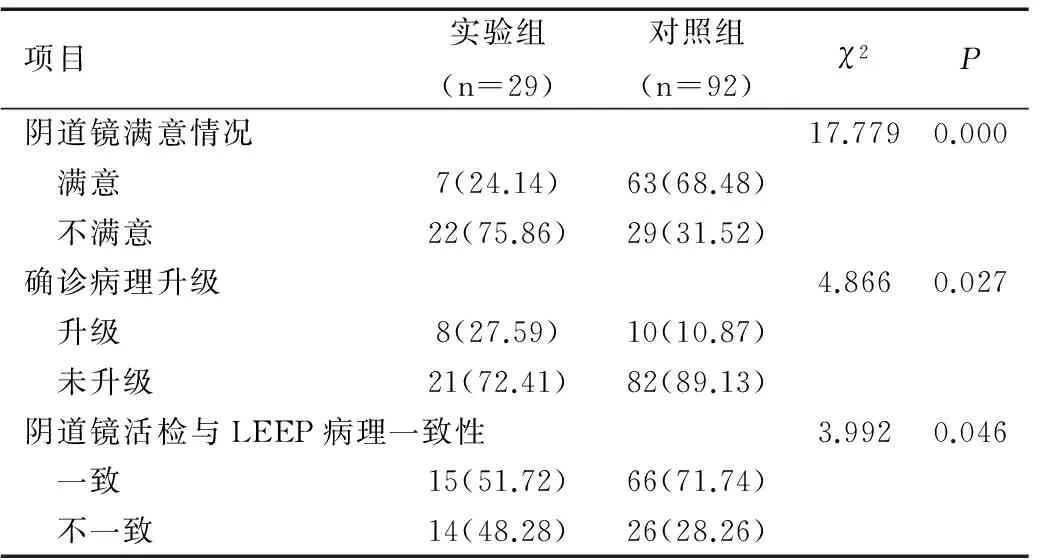
项目实验组(n=29)对照组(n=92)χ2P阴道镜满意情况17.7790.000 满意7(24.14)63(68.48) 不满意22(75.86)29(31.52)确诊病理升级4.8660.027 升级8(27.59)10(10.87) 未升级21(72.41)82(89.13)阴道镜活检与LEEP病理一致性3.9920.046 一致15(51.72)66(71.74) 不一致14(48.28)26(28.26)
2.4两组患者LEEP术后切缘阳性情况比较
实验组患者行LEEP术后病理结果提示切缘阳性率(22.22%)高于对照组(10.18%),但两组间无显著性差异(χ2=3.416,P=0.065),其中实验组内切缘阳性率(11.11%)明显高于对照组(1.85%),两组间差异有显著性意义(χ2=5.797,P=0.016);实验组外切缘阳性率(11.11%)高于对照组(8.33%),但两组间无显著性差异(χ2=0.254,P=0.615)。
2.5两组患者手术的损伤情况比较
出血是LEEP手术的最常见并发症。本研究中实验组、对照组均无宫颈周边脏器的损伤。实验组患者术中出血>10mL 2例(5.56%),对照组患者术中出血>10mL 9例(8.33%),两组间差异无统计学意义(χ2=0.295,P=0.587),两组出血多的患者均可见病变位置深、浅表血管丰富。
3讨论
3.1宫颈细胞学检查及HR-HPV检测在绝经后女性宫颈癌疾病筛查的价值
宫颈细胞学检查及HR-HPV检测是宫颈癌疾病筛查的最主要两项检测手段。本研究中,实验组(绝经后)与对照组(绝经前)患者宫颈细胞学检查及HR-HPV检测阳性率无显著性差异(P>0.05),这提示常规的宫颈癌疾病筛查手段同样适用于绝经后女性。故本研究选择的两组间术前临床特征、实验室检查一致,具有可比性。
3.2阴道镜下活检在绝经后女性宫颈癌疾病筛查的价值
阴道镜下活检是诊断子宫颈癌及癌前病变的一项精准检查。但绝经后女性宫颈转化区上移、宫颈萎缩,阴道镜检查的满意率及准确性均较绝经前患者下降。Suram等[5]学者提出阴道镜检查前使用雌激素或米索前列醇可增加阴道镜检查的满意率,从而佐证这一理论。
3.3LEEP术在绝经后女性宫颈癌疾病诊疗中的价值
针对绝经后高级别CIN患者的诊疗规范目前尚未统一。既往国内外多数医院选择针对绝经后患者行全子宫切除术,但往往过度治疗,且并不降低患者的死亡率。目前,越来越多绝经后患者接受子宫颈锥形切除术作为诊疗手段。本研究中绝经前后患者行LEEP手术的损伤出血无显著性差异,出血因素多见于与病变位置深、浅表血管丰富的患者。同时相应文献也提示绝经后患者切缘阳性率明显高于绝经前人群。Cheng等[6]学者发现101例绝经后且接受子宫颈锥切术的患者中约20.8%出现切缘阳性,相比于绝经前患者(10.9%)有显著性差异。在本研究中,实验组患者切缘阳性率(22.22%)高于对照组(10.18%),但两组间差异无统计学差异(P>0.05),考虑为样本量不足的可能,今后可扩大研究样本进一步讨论。但其中绝经后患者内切缘阳性率(11.11%)明显高于绝经前(1.85%),两组间差异有统计学意义(P<0.05),这与绝经后宫颈管萎缩及转化区上移的生理变化相关,提示临床操作中对于绝经后患者需高度警惕,必要时需加大锥形切除柱高。但通过与阴道镜活检的比较,可发现绝经后宫颈LEEP术后病理级别升级率显著增加。
综上所述,阴道镜下活检诊断ClN,目前尚不能完全替代高频电刀手术。阴道镜是一种视觉技术,有赖于检查者有严格的训练和丰富的经验。由于炎性反应和HPV感染也可产生阴道镜下异常图象,因此阴道镜诊断CIN的敏感性高而特异性低,对阴道镜活检后诊为CIN的患者应行LEEP进一步确诊诊断,以尽量避免过度治疗以及漏诊。
[参考文献]
[1]Oakeshott P,Aghaizu A,Reid F,etal.Frequency and risk factors for prevalent, incident, and persistent genital carcinogenic human papillomavirus infection in sexually active women: community based cohort study[J].BMJ,2012,344:e4168.
[2]Massad L S,Einstein M H,Huh W K,etal.2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors[J].Obstet Gynecol,2013,121(4):829-846.
[3]Castle P E,Gage J C,Wheeler C M,etal.The clinical meaning of a cervical intraepithelial neoplasia grade 1 biopsy[J].Obstet Gynecol,2011,118(6):1222-1229.
[4]Liu H,Liu S,Wang H,etal.Genomic amplification of the human telomerase gene (hTERC) associated with human papillomavirus is related to the progression of uterine cervical dysplasia to invasive cancer[J].Diagn Pathol,2012,7:147.
[5]Suram A,Kaplunov J, Patel P L,etal.Oncogene-induced telomere dysfunction enforces cellular senescence in human cancer precursor lesions[J].EMBO J,2012,31(13):2839-2851.
[6]Cheng X,Feng Y,Wang X,etal.The effectiveness of conization treatment for post-menopausal women with high-grade cervical intraepithelial neoplasia[J]. Exp Ther Med,2013 5(1):185-188.
[专业责任编辑:韩晓兵]
[收稿日期]2016-02-29
[作者简介]陶恬阗(1979-),女,主治医师,主要从事妇产科临床工作。
[通讯作者]江海燕,副主任医师。
doi:10.3969/j.issn.1673-5293.2016.04.037
[中图分类号]R711.7
[文献标识码]A
[文章编号]1673-5293(2016)04-0527-03
Significance evaluation of LEEP for post menopausal women with high grade cervical intraepithelial neoplasia
TAO Tian-tian, JIANG Hai-yan
(Quzhou Maternal and Child Health Hospital, Zhejiang Quzhou 324000, China)
[Abstract]Objective To evaluate the significance of LEEP in the diagnosis and treatment of high-grade cervical intraepithelial neoplasia (CIN) in post-menopausal women. Methods Clinical data of 354 patients undergoing LEEP in Quzhou Maternal and Child Health Hospital were analyzed, including 36 post-menopausal women in experimental group and 108 pre-menopausal patients in control group. Clinical manifestations, cytological examination, HR-HPV examination, colposcopy and pathological results after LEEP were analyzed. Results The satisfaction rate of colposcopy in the experimental group was significantly lower than in the control group (χ2=17.779,P=0.000). The postoperative pathological results after LEEP were taken as gold standards for diagnosis. The pathological levels in the experimental group were significantly higher than those in the control group (χ2=4.866,P=0.027). The accuracy of biopsy under colposcopy was significantly lower in the experimental group than in the control group (χ2=3.992,P=0.046). After LEEP, the positive rate of the cutting edge in the experimental group was higher than in the control group, but no significant difference between two groups was found (χ2=3.416, P=0.065). The positive rate of internal margin in the experimental group was higher, and there was significant difference between two groups (χ2=5.797,P=0.016). The experimental group had higher positive rate of external margin than the control group, but no significant difference was indicated (χ2=0.254,P=0.615). Conclusion Post-menopausal women are suggested to take cervical cancer screening regularly, including TCT and HR-HPV test. Both the satisfaction rate and accuracy of colposcopy decline for post-menopausal women. LEEP is needed for further confirm diagnosis among cases diagnosed with CIN after colposcopic biopsy.
[Key words]cervical intraepithelial neoplasia (CIN); loop electrosurgical excision procedure (LEEP); high risk-human papillomavirus (HR-HPV); post-menopause